Blood Pressure
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Vascular System
1. Explain blood pressure and how it is calculated. 2. Contrast systolic and diastolic blood pressure. 3. Describe the differences between arterial and venous blood pressure. 4. What is net filtration pressure?
Blood
Pressure
Blood
pressure is the pressure exerted by the blood’scirculating volume on
the walls of the arteries, veins, and heart chambers. It is regulated by the
body’s homeostatic mechanisms, involving blood volume, the lumens of arteries
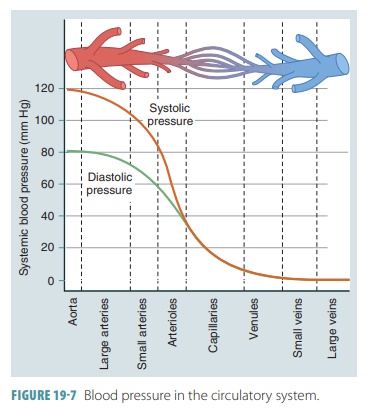
and arterioles, and the force of cardiac contraction. The systemic blood pressure is at its highest level in the aorta,
declining along the blood pathways, until it is at 0 mm Hg in the right atrium.
The largest drop in blood pressure occurs in the arteri-oles, which have the
most resistance to blood flow. The pressure gradient continues, even though it
is small, allowing blood to flow all the way back to the heart.
Arterial Blood Pressure
Arterial blood pressure rises and falls accord-ing to cardiac
cycle phases. It is important in the maintenance of blood flow through the
capillary beds. Arterial blood pressure must always be sufficient in order to
overcome peripheral resistance. Arterial blood pressure is equivalent to the
term “blood pres-sure.” The maximum pressure during ventricular contraction is
called the systolic
pressure, averag-ing 120 mm Hg in a healthy adult. FIGURE 19- 7 shows changes in blood pressure as
distance from the left ventricle increases. The lowest pressure that remains in
the arteries before the next ventricular contrac-tion is called the diastolic pressure, which averages between 70 and 80
mm Hg in a healthy adult. There-fore, systole
refers to periods of contraction, whereas diastole
refers to periods of relaxation. The cardiaccycle includes atrial systole
and diastole, followed by ventricular systole and diastole. An
electrocar-diogram illustrates all these mechanical events. The cardiac cycle
is signified by continual pressure and blood volume changes within the heart.
In diastole, the aortic valve closes. Blood cannot flow back
into the heart. There is a recoiling of the walls of the aorta and other
elastic arteries. There is enough pressure maintained so the blood can flow
into the smaller vessels. Aortic pressure drops to its lowest level at this
time, which is described as the dia-stolic pressure. The difference between the
systolic and diastolic pressures is known as pulse pressure. During systole, it is felt in an
artery as a throbbing pul-sation.
This is due to ventricular contraction, whichforces blood into the elastic
arteries, expanding them. Pulse pressure is temporarily raised by increased
stroke volume and quicker blood ejection because ofincreased contractility from
the heart. Pulse pressure is chronically increased by atherosclerosis. This is
because of the loss of elasticity in the elastic arteries. A single blood
pressure value is reported by using meanarterial
pressure (MAP).This
is calculated by addingone-third of the pulse pressure to the diastolic pres-sure,
as follows:
MAP = Diastolic pressure + (Pulse pressure/3)
If the systolic pressure is 120 mm Hg and the
diastolic pressure is 90 mm Hg, the MAP would be calculated as follows:
MAP = 90 + [(120 – 90)/3] = 90 + 10 = 100 mm Hg
Healthy individuals have a normal range of sys-tolic and
diastolic pressures. When these pressures become abnormal, clinical problems
develop. Hyper-tension describes
abnormally high blood pressure, and hypotension
describes abnormally low blood pressure.Hypertension is much more common than
hypotension. However, many cases of hypotension are caused by use of
antihypertensive drugs that is excessive. According to the American Heart
Association, adult hypertension exists when the blood pressure reaches 140/90.
Blood pressure of 120/80 or less is normal. Blood pressure between 121/81 and
139/89 signifies pre-hypertension.
For pre-hypertensive patients, it is recommended that dietary changes and drug
therapy are used in order to prevent hypertension from developing.
Hypertension greatly increases the heart’s work-load,
resulting in gradual enlargement of the left ventricle. With more muscle mass,
the body has a greater demand for oxygen. When coronary cir-culation is not
sufficient, there will be signs and symptoms of coronary ischemia. Increased arterial pressure puts physical stress
upon the body’s blood vessel walls. The increases or encourages devel-opment of
arteriosclerosis, as well as risk of heart attack, stroke, and aneurysms.
Arterial blood pressure is measured with a device called a sphygmomanometer or blood pressure cuff. Its results
are reported as a fraction of the sys-tolic pressure over the diastolic
pressure. The upper or first number
indicates the arterial systolic pressure in mm Hg, and the lower or second number indi-cates the arterial
diastolic pressure, also in mm Hg. A millimeter of mercury is a unit of
pressure equal to 0.001316 of normal atmospheric pressure. This means a blood
pressure of 120/80 displaces 120 mm of Hg on a sphygmomanometer, showing the
systolic pressure, and also displaces 80 mm of Hg on the same device, showing
diastolic pressure.
The artery walls are distended as blood surges into them
from the ventricles, but they recoil almost immediately. This expansion and
recoiling can be felt as a pulse in
an artery near the surface of the skin. Most commonly, the radial artery is
used to take a person’s pulse, although the carotid, brachial, and femoral
arteries also can be used. Arterial blood pressure depends on heart rate,
stroke volume, blood volume, peripheral resistance, and blood viscosity. The
recoil-ing of arteries to their original dimensions is known as elastic rebound.
Capillary Blood Pressure
In the capillaries blood pressure drops off to only
approximately 35 mm Hg, with the ends of capil-lary beds having only 17 mm Hg
of pressure. This is important because the capillaries are fragile and eas-ily
ruptured. They are also extremely permeable, and low capillary pressures can
cause filtrate to be forced out of the bloodstream into the interstitial space.
Venous Blood Pressure
The venous blood pressure is steady and regular. It does not
pulsate with the ventricular contractions like the arterial blood pressure. In
the veins, the pres-sure gradient is only approximately 15 mm Hg. Con-sider
that from the aorta to the ends of the arterioles, the pressure is
approximately 60 mm Hg. Venous blood pressure is usually too low to cause
venous return to be adequate. Therefore, the muscular pump, respiratory
pump, and sympathetic
venoconstriction are used.
The muscular
pump uses skeletal muscle activity to contract and relax around
the veins, moving blood toward the heart. Each vein valve keeps blood that has
passed from flowing backward. As pressure changes in the body’s ventral cavity
during breathing, the respi-ratory
pump moves blood toward the heart. Inha-lation
increases abdominal pressure, squeezing local veins and forcing blood to the
heart. Simultaneously, the chest pressure decreases. The internal and external
thoracic veins then expand and increase blood entry into the right atrium. The
volume of blood in the veins is then reduced by sympathetic venoconstriction. Sympathetic control
causes the smooth muscle layer around the veins to constrict, reducing venous
vol-ume. Blood is therefore pushed toward the heart. Together, the muscular
pump, respiratory pump, and sympathetic venoconstriction increase venous return
and stroke volume.
Total Peripheral Resistance
The difference in pressure over the entire systemic circuit
is sometimes called circulatory pressure.
This is approximately 100 mm Hg. Total
peripheral resistance is defined as the resistance of the entire
cardiovascular system. For circulation to occur, the circulatory pres-sure must
overcome the total peripheral resistance. The relatively high pressure of the
arterioles is mostly reflected by the large pressure gradient of the arterial
network, which is about 65 mm Hg. Total peripheral resistance combines vascular
resistance, blood viscos-ity, and turbulence. Vascular resistance is the most important component of
total peripheral resistance and involves vessel length and diameter. Viscosity, or the resistance to blood
flow caused by interactions among molecules and suspended materials, is the
second component. Turbulence is
defined as changes that increase resistance and slow down the blood flow,
including irregular surfaces, high flow rates, and sud-den changes in the
diameters of blood vessels.
Net Filtration Pressure
The net
filtration pressureis the difference between the net osmotic pressure and the
net hydrostatic pres-sure. At arterial ends of capillaries, this is usually 10
mm Hg. This positive value shows that fluid usu-ally moves out of capillaries,
into the interstitial fluid. This means that filtration is occurring. However,
at the venous ends of capillaries, the net filtration pressure is usually –7 mm
Hg. This negative value shows that fluid usually moves into the capillaries,
meaning that reabsorption is occurring. Whenever net filtration pressure is
zero, hydrostatic and osmotic forces are equal. Therefore, the transition
between filtration and reabsorption occurs where capillary hydrostatic
pres-sure is 25 mm Hg.
Tissue Perfusion
Blood flow through tissues is also known as tissueperfusion. This occurs by
homeostatic regulationof cardiovascular activities so that needs for oxygen and
nutrients are met. The factors affecting tissue per-fusion are cardiac output,
peripheral resistance, and blood pressure. Cardiovascular regulation ensures
that blood flow changes occur at appropriate times in areas of the body that
require it without significantly changing blood pressure and flow to the vital
organs.
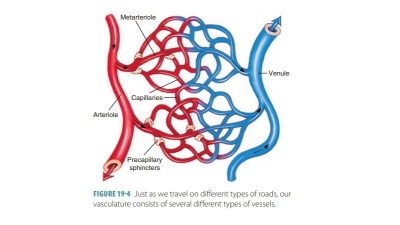
The three mechanisms that are involved include
autoregulation, neural mechanisms, and endocrine mechanisms. Autoregulation involves local factors
that alter blood flow inside capillary beds, with pre-capillary sphincters
opening and closing because of chemical changes in interstitial fluids. Neural mecha-nisms occur in response to
arterial pressure changesor blood gas level changes in certain areas. Endocrinemechanisms involve hormones
that enhance short-term changes and that also balance long-term changes in
cardiovascular activities.
Dilation of precapillary sphincters are promoted by vasodilators. At the tissue level, local vasodilators help to speed up
blood flow through their tissues of origin. Local vasodilators include acids
from tissue cells, such as lactic acid; increased carbon dioxide or decreased
tissue oxygen levels; increased concen-trations of hydrogen or potassium ions
in interstitial fluid; endothelial cells releasing nitric oxide; elevations in
local temperature; and release of chemicals, such as nitric oxide or histamine
during local inflammation. Also, localvasoconstrictors, such as thromboxanes,
prostaglandins, and endothelins, stimulate precapil-lary sphincters to
constrict. Together, local vasodila-tors and vasoconstrictors balance blood
flow in single capillary beds. Higher concentrations of these factors affect
arterioles as well.
Blood
Volume
Blood volume is defined as the sum of formed ele-ments and
plasma volumes in the vascular system. Blood volume varies with age, body size,
and gen-der. Most adults have approximately 5 liters of blood, which makes up
8% of the body’s weight in kilograms. This is only slightly more than 1 gallon
of blood. Blood pressure and volume are usually directly proportional. Any
changes in volume can initially alter pressure. When measures are taken to
restore normal blood volume, normal blood pressure can be reestablished. Fluid
balance fluctuations may also affect blood vol-ume. The entire blood supply
pumps through each side of the heart about once per minute.
1. Explain blood pressure and how it is calculated.
2. Contrast systolic and diastolic blood pressure.
3. Describe the differences between arterial and venous blood
pressure.
4. What is net filtration pressure?