Chapter Summary, Questions Answers - Metabolic Effects of Insulin and Glucagon
| Home | | Biochemistry |Chapter: Biochemistry : Metabolic Effects of Insulin and Glucagon
The integration of energy metabolism is controlled primarily by insulin and the opposing actions of glucagon and the catecholamines, particularly epinephrine.
CHAPTER SUMMARY
The integration of
energy metabolism is controlled primarily by insulin and the opposing actions
of glucagon and the catecholamines, particularly epinephrine (Figure 23.17).
Changes in the circulating levels of these hormones allow the body to store
energy when food is abundant or to make stored energy available in times of
physiologic stress (for example, during “survival crises,” such as famine).
Insulin is a peptide hormone produced by the β cells of the islets of
Langerhans of the pancreas. It consists of disulfide-linked A and B chains. A
rise in blood glucose is the most important signal for insulin secretion. The
catecholamines, secreted in response to stress, trauma, or extreme exercise,
inhibit insulin secretion. Insulin increases glucose uptake (by muscle and
adipose) and the synthesis of glycogen, protein, and triacylglycerol: it is an
anabolic hormone. These actions are mediated by binding to its tyrosine kinase
receptor. Binding initiates a cascade of cell-signaling responses, including
phosphorylation of a family of proteins called insulin receptor substrate
proteins. Glucagon is a monomeric peptide hormone produced by the α cells of
the pancreatic islets (both insulin and glucagon synthesis involves formation
of inactive precursors that are cleaved to form the active hormones). Glucagon,
along with epinephrine, norepinephrine, cortisol, and growth hormone (the
“counterregulatory” hormones), opposes many of the actions of insulin. Glucagon
acts to maintain blood glucose during periods of potential hypoglycemia.
Glucagon increases glycogenolysis, gluconeogenesis, fatty acid oxidation,
ketogenesis, and uptake of amino acids: it is a catabolic hormone. Glucagon
secretion is stimulated by low blood glucose, amino acids, and the
catecholamines. Its secretion is inhibited by elevated blood glucose and by
insulin. Glucagon binds to high-affinity receptors of hepatocytes. Binding
results in the activation of adenylyl cyclase, which produces the second
messenger cyclic adenosine monophosphate (cAMP). Subsequent activation of
cAMP-dependent protein kinase A results in the phosphorylation-mediated
activation or inhibition of key regulatory enzymes involved in carbohydrate and
lipid metabolism. Both insulin and glucagon affect gene transcription.
Hypoglycemia is characterized by low blood glucose accompanied by adrenergic
and neuroglycopenic symptoms that are rapidly resolved by the administration of
glucose. Insulin-induced, postprandial, and fasting hypoglycemia result in
release of glucagon and epinephrine. The rise in nicotinamide adenine
dinucleotide (NADH) that accompanies ethanol metabolism inhibits
gluconeogenesis, leading to hypoglycemia in individuals with depleted stores.
Alcohol consumption also increases the risk for hypoglycemia in patients using
insulin. Chronic alcohol consumption can cause fatty liver disease.
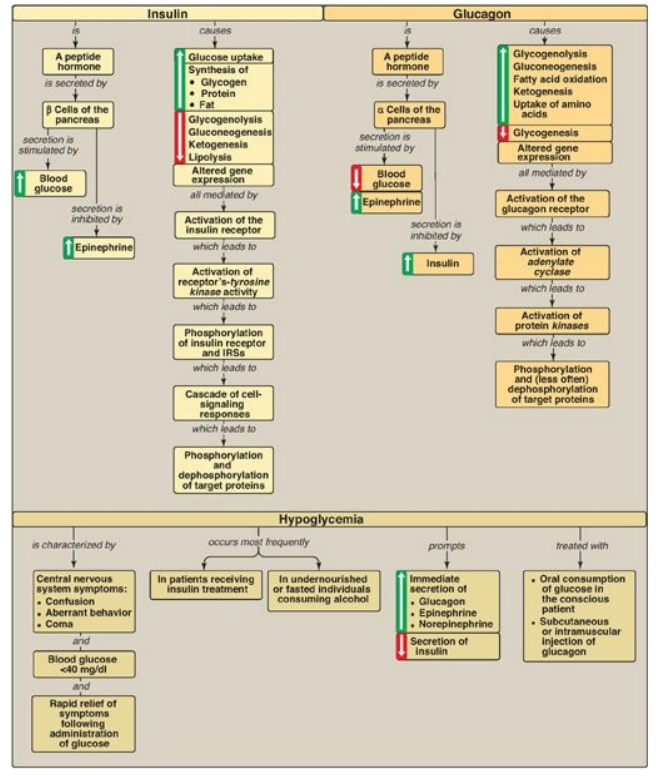
Figure 23.17 Key concept map
for the metabolic effects of insulin and glucagon, and hypoglycemia. IRSs =
insulin receptor substrates.
Study Questions
Choose the ONE best answer.
23.1 Which of the following statements is true for
insulin but not for glucagon?
A. It is a peptide
hormone secreted by pancreatic cells.
B. Its actions are
mediated by binding to a receptor found on the cell membrane of liver cells.
C. Its effects include
alterations in gene expression.
D. Its secretion is decreased by the
catecholamines.
E. Its secretion is
increased by amino acids.
F. Its synthesis
involves a nonfunctional precursor that gets cleaved to yield a functional
molecule.
Correct answer = D. Secretion of insulin by pancreatic
β cells is inhibited by the catecholamines, whereas glucagon secretion by the α
cells is stimulated by them. All of the other statements are true for both
insulin and glucagon.
23.2 In which one of the following tissues is
glucose transport into the cell insulin dependent?
A. Adipose
B. Brain
C. Liver
D. Red blood cells
Correct answer = A. The glucose transporter (GLUT-4)
in adipose (and muscle) tissue is dependent on insulin. Insulin results in
transport of GLUT-4 from intracellular vesicles to the cell membrane. The other
tissues in the list contain GLUTs that are independent of insulin because they
are always located on the cell membrane.
23.3 A 39-year-old woman is brought to the
emergency room complaining of weakness and dizziness. She recalls getting up
early that morning to do her weekly errands and had skipped breakfast. She
drank a cup of coffee for lunch and had nothing to eat during the day. She met
with friends at 8 p.m. and had a few drinks. As the evening progressed, she
soon became weak and dizzy and was taken to the hospital. Laboratory tests
revealed her blood glucose was 45 mg/dl (normal = 70– 99). She was given orange
juice and immediately felt better. The biochemical basis of her alcohol-induced
hypoglycemia is an increase in:
A. fatty acid
oxidation.
B. the ratio of the reduced-to-oxidized forms of
nicotinamide adenine dinucleotide.
C. oxaloacetate and
pyruvate.
D. use of acetyl
coenzyme A in fatty acid synthesis.
Correct answer = B. The oxidation of ethanol to
acetate by dehydrogenases is accompanied by the reduction of nicotinamide
adenine dinucleotide (NAD+) to NADH. The rise in NADH shifts
pyruvate to lactate and oxaloacetate (OAA) to malate, decreasing the
availability of substrates for gluconeogenesis and resulting in hypoglycemia.
The rise in NADH also reduces the NAD+ needed for fatty acid
oxidation. The decrease in OAA shunts any acetyl coenzyme A produced to
ketogenesis. Note that the inhibition of fatty acid degradation results in
their reesterification into triacylglycerol that can result in fatty liver.
23.4 A patient is diagnosed with an insulinoma, a
rare neuroendocrine tumor, the cells of which are derived primarily from
pancreatic β cells. Which of the following would logically be characteristic of
an insulinoma?
A. Decreased body
weight
B. Decreased connecting
peptide in the blood
C. Decreased glucose in the blood
D. Decreased insulin in
the blood
Correct answer = C. Insulinomas are characterized by
constant production of insulin (and, therefore, of C-peptide) by the tumor
cells. The increase in insulin drives glucose uptake by tissues such as muscle
and adipose that have insulin-dependent glucose transporters, resulting in
hypoglycemia. The hypoglycemia is insufficient to suppress insulin production
and secretion, however. Insulinomas, then, are characterized by increased blood
insulin and decreased blood glucose. Insulin, as an anabolic hormone, results
in weight gain.
23.5 In a patient with an even rarer
glucagon-secreting tumor derived from the α cells of the pancreas, how would
the presentation be expected to differ relative to the patient in Question
23.4?
A glucagon-secreting
tumor of the pancreas (glucagonoma) would result in hyperglycemia, not
hypoglycemia. The constant production of glucagon would result in constant
gluconeogenesis, using amino acids from proteolysis as substrates. This results
in loss of body weight.
Related Topics
