Epithelial Tissues
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Levels of Organization : Tissues
Epithelial tissues include epithelia and glands. Epithelium covers the surface of the skin and organs, forms the inner lining of the body’s cavities, and also lines hollow organs.
Types of Tissues
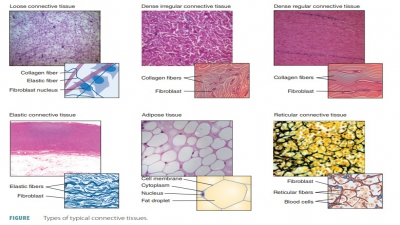
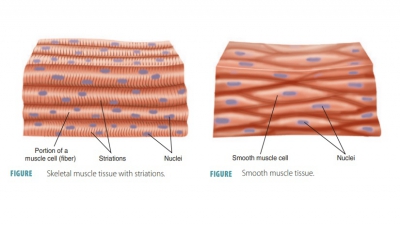
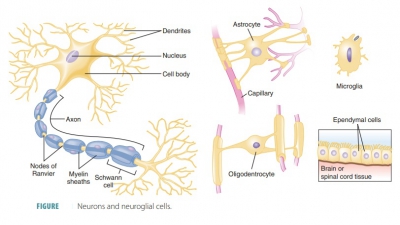
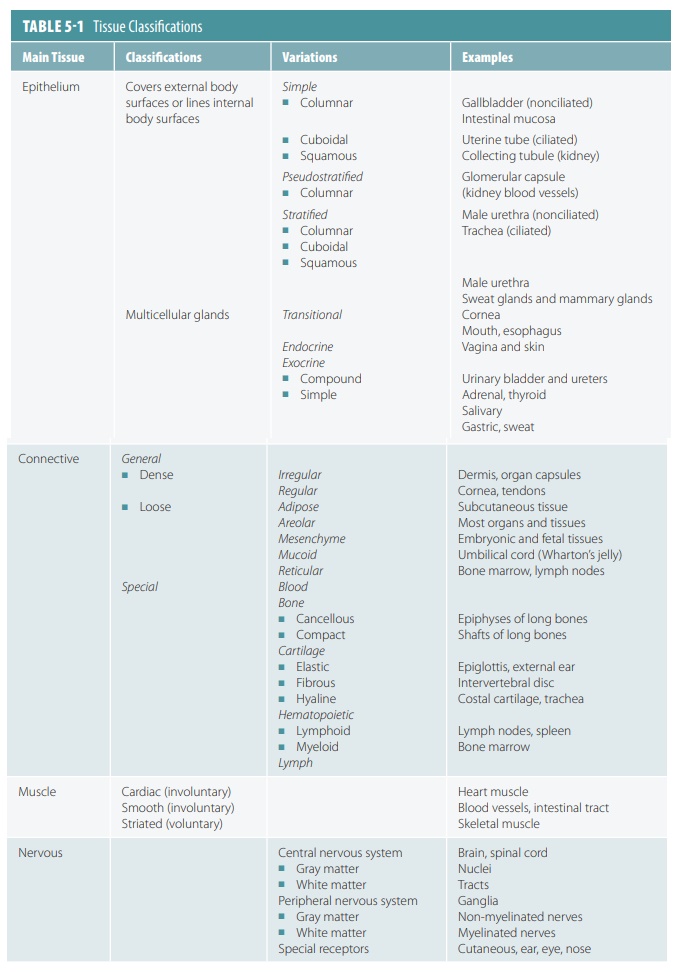
The human body is primarily made up of four major types of tissues: epithelial, connective, muscle, and nervous. Epithelial tissues cover body surfaces, cover and line internal organs, and make up the glands. Connective tissues are widely distributed throughout the body, filling internal spaces, and func-tion to bind, support, and protect body structures. Muscle tissues are specialized for contraction and include the skeletal muscles of the body, the heart, and the muscular walls of hollow organs. Skeletal muscles are attached to bones and are used for movement of the body. Nervous tissues carry information from one part of the body to another via electrical impulses. They are found in the brain, spinal cord, and nerves (TABLE 5-1).
The human body is primarily made up of four major types of tissues:
1. epithelial,
2. connective
3. muscle, and
4. nervous.
Epithelial Tissues
Epithelial tissues include epithelia and glands. Epithelium covers the surface of the skin and organs, forms the inner lining of the body’s cavities, and also lines hollow organs. Throughout the body, epithelial tissues are anchored to connective tissues by a basement membrane. An epithelium is an avascular layer of cells that forms a barrier, provid-ing protection and regulating permeability. Glands are secretory structures derived from epithelia.
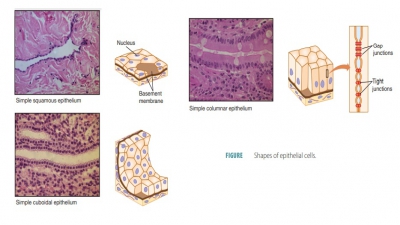
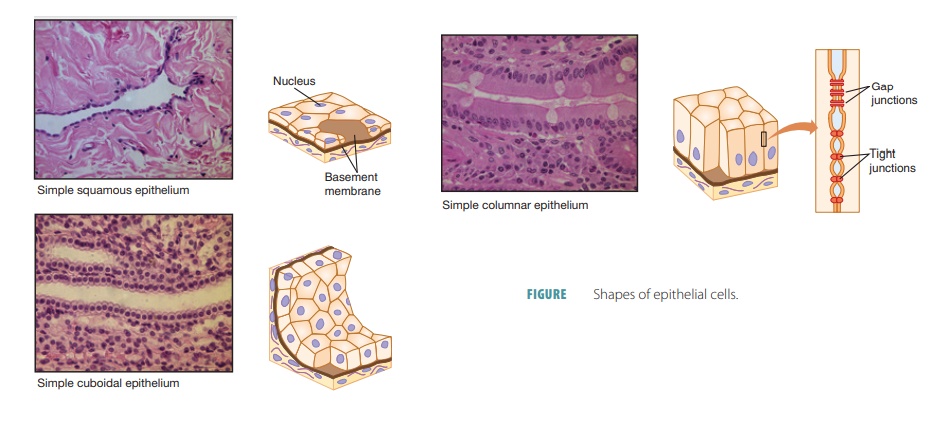
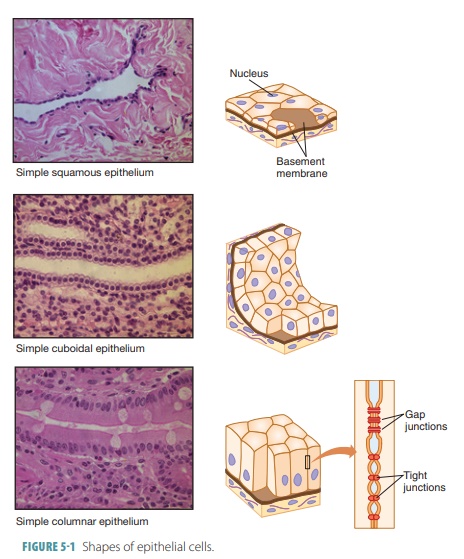
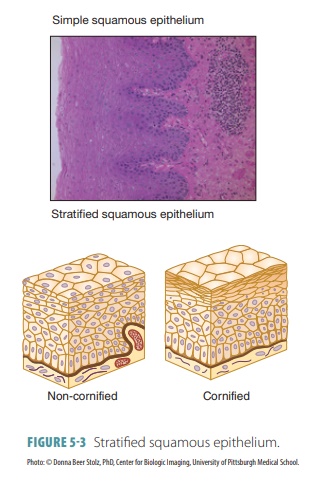
Epithelial cells divide quickly, aiding in wound healing and replacement of cells when damage occurs. Tightly packed epithelial cells protect body structures such as the outer skin and the lining of body cavities such as the mouth. Epithelial tissues are involved in secretion, absorption, and excretion. They also pro-vide sensation, and are classified according to the shape of their cells and the number of cell layers that exist (FIGURE 5-1). Different types of epithelial tissues are summarized in TABLE 5-2.
Epithelia perform many functions:
■■ Physical protection: Epithelia protect exposed and internal surfaces from abrasion, dehydration, and destruction from biologic or chemical agents. Smooth, tightly interlocked epithelial cells of the circulatory system reduce friction between the blood and the walls of the blood vessels.
■■ Absorption: Epithelia also control absorption, which is related to permeability. Examples of epi-thelia that absorb or secrete substance are those that line the kidney tubules and intestine. In the intestine, certain epithelia absorb nutrients from the digestion of food.
■■ Filtration: Some epithelia have tiny, motile cilia that propel substance along free surfaces, as part of filtration. These include epithelia lining the trachea and other air passages. Also, a thin supporting sheet adjacent to the basal surface of an epithelium is called the basal lamina, which acts as a selective filter. It determines which mol-ecules that diffuse from underlying connective tissue can enter the epithelium.
■■ Excretion: In the kidneys, epithelia excrete waste products and also reabsorb needed materials from the urine. In the skin, the epithelia of sweat glands excrete sweat.
■■ Sensation: Most epithelia are very sensitive to stimulation because they have a large sensory nerve supply. Sensory stimuli penetrate special-ized epithelia. Such tissue is found in the eyes, ears, skin, nose, and on the tongue.
■■ Specialized secretions: Epithelial cells that produce secretions are called gland cells, and individual cells of this type are scattered among other types of cells in an epithelium. Most or all of the epithelial cells in a glandular epithelium produce secretions, which are either discharged onto the surface of the epi-thelium or released into the surrounding interstitial fluid and blood. These secretions include enzymes, hormones, and lubricating fluids.
■■ Permeability: Any substance entering or leaving the body must cross an epithelium, so the epithe-lia control permeability. Some epithelia are rela-tively impermeable, whereas others are crossed easily by compounds of various sizes. In response to stimuli, the epithelial barrier may be modified and regulated. Hormones can affect ion and nutri-ent transport through epithelial cells. Physical stress can also alter the structure and properties of epithelia. An example is the formation of calluses on the hands after repeated manual labor.
■■ Regeneration: Epithelia have a strong ability to regenerate because they are often exposed to friction, acids, bacteria, smoke, and other envi-ronmental substances or factors. They begin to reproduce quickly when their apical–basal polar-ity and lateral contacts are destroyed. Epithelia can replace lost cells (due to cell division) for as long as they receive enough nutrition.
Classification of Epithelia
There are two names for each type of epithelium: one describes how many cell layers are present and the other describes the shape of the cells that make up the epithelium. Simple epithelia have one cell layer and are usually found in areas where absorption, filtration, and secretion occur. In these areas, only a thin epithelial barrier is needed. Stratified epithe-lia are made of two or more cell layers stacked on each other. They are usually found in areas of high abrasion that require protection. Examples of these areas include the lining of the mouth and the skin surfaces. All stratified epithelial cells have six irregu-lar sides, resembling the appearance of a honeycomb. As a result of their shapes, these cells can be loosely packed together. The shape of each epithelial cell’s nucleus resembles the overall cell shape. Simple epi-thelia are easier to classify because of shapes that are nearly identical (Figure 5-1). The cell shape of strat-ified epithelia, however, is different based on each layer. Therefore, stratified epithelial are named based on how cells are shaped in their apical layer. The following are the various forms of epithelial tissues:
Simple Squamous Epithelium
Simple squamous epithelium consists of a single layer of thin and laterally flattened cells with flattened, disc-like nuclei. It lines areas where filtration or rapid diffusion occurs, including the alveoli of the lungs and in the kidneys. It forms capillary walls, lines blood and lymph vessels, and covers membranes that line body cavities. Squamous cells have a scale-like appearance. The cytoplasm of simple squamous epithelium is sparse and often permeable. In the kidneys, it makes up part of the filtration membrane, and in the lungs, it forms the walls of the alveoli.
Two types of simple squamous epithelia are named according to their locations. Endothelium provides a slick lining in lymphatic vessels and in the hollow organs of the cardiovascular system, where it reduces friction. These organs include the blood vessels and heart. The capillaries are completely made up of endothelium. Its thin structure allows for efficient nutrient and waste exchanges between surrounding tissue cells and the bloodstream. The mesothelium is the epithelium inside serous mem-branes, which line the ventral body cavity and cover its organs.
Simple Cuboidal Epithelium
Simple cuboidal epithelium consists of a single layer of cube- shaped cells with round nuclei. When stained, these nuclei become dark and the cell layer resembles a string of pearls. It covers the ovaries, lines many kidney tubules and glandular ducts, and functions in secretion and absorption. Cuboidal cells appear to be approximately the same size in height and width.
Simple Columnar Epithelium
Simple columnar epithelium consists of cells that are longer than wide, composed of a single cellular layer with elongated nuclei, located near the basement membrane, and may have cilia on their surfaces. It is found in the female reproduc-tive tubes, uterus, and most digestive tract organs, being involved in secretion and absorption. Simple columnar cells, specialized for absorption, usually have tiny, cylinder-shaped processes (microvilli) that extend from their surfaces and increase the sur-face area of the cell membrane. Often, special flask-shaped glandular cells (goblet cells ) are scattered among the columnar cells, secreting mucus on the tissue surface (Figure 5-1).
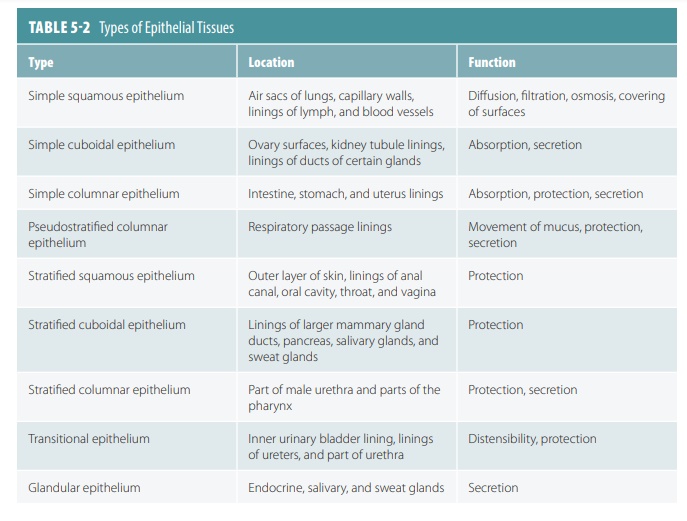
Pseudostratified Columnar Epithelium
Pseudostratified columnar epithelium appears as if it is layered (hence the word “pseudostratified”) because the nuclei are located at different levels (FIGURE 5-2). The cells vary in shape and usually reach the basement membrane. Pseudostratified colum-nar epithelium usually has cilia and lines respiratory system passages as well as being involved in secretion and absorption. Goblet cells are found throughout this tissue.
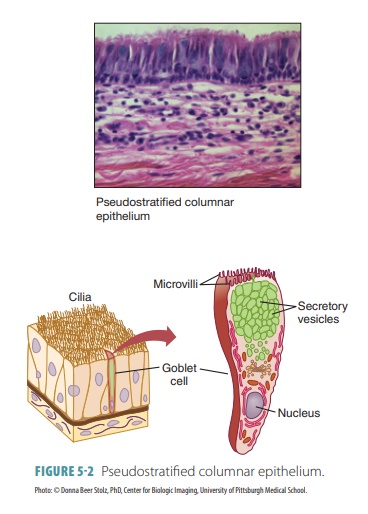
Stratified Squamous Epithelium
Stratified squamous epithelium is a thick layer with cells that flatten as they are pushed outward. It forms the epidermis, with cells hardening as they age (keratinization). It also lines the mouth, esophagus, vagina, and anus, where the cells do not harden but remain soft and moist. Stratified epithelia regener-ate from below, with basal cells dividing and push-ing apically, replacing older surface cells. They are much more durable than simple epithelia. Strati-fied squamous epithelium is the most widespread of all stratified epithelia. Interestingly, the cells of its deeper layers are columnar or cuboidal. Although the epidermis is keratinized, other areas of stratified squamous epithelium in the body are nonkerati-nized. This is also described as “cornified” or “non-cornified” (FIGURE 5-3).
Stratified Cuboidal Epithelium
Stratified cuboidal epithelium consists of usually two but may have up to three layers of cubed cells. It lines the mammary gland ducts, sweat glands, salivary glands, pancreas, and the developing ovaries and sem-iniferous tubules. This type of epithelium is rare in the body compared with other types.
Stratified Columnar Epithelium
Stratified columnar epithelium consists of several layers of either columnar or cubed shapes. It is found in the male urethra, ductus deferens, and areas of the pharynx, but in few other areas of the body. It occurs at junctions or transition areas between two other types of epithelia. In this type, only the apical layer of cells is columnar.
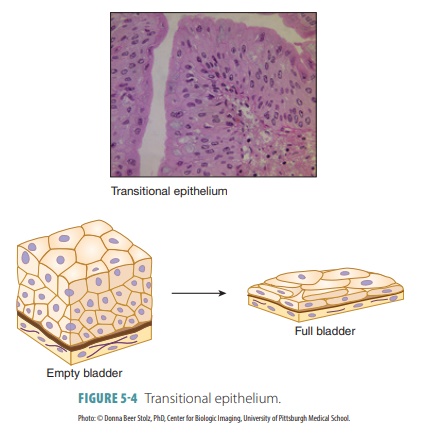
Transitional Epithelium
Transitional epithelium changes in appearance in response to tension. It lines the urinary bladder, ure-ters, and superior urethra and prevents urinary tract contents from diffusing back into the internal body environment. The cells of its basal layer are colum-nar or cuboidal. Apical cells have different appear-ances, based on how much distention occurs in the specific organ in which they are found. For example, distention of the bladder with urine causes it to thin from approximately six cell layers to only three, with the dome-like apical cells flattening to appear like squamous cells (FIGURE 5-4). This transitional ability allows for greater volumes of urine to be stored in the bladder or in tube-like organs for more urine to flow through.
Glandular Epithelium
Glandular epithelium consists of specialized cells that produce and secrete substances into ducts or body fluids. It is usually found in exocrine glands (which open onto surfaces or into the digestive tract) or in endocrine glands (which secrete into tissue fluid or blood). The basic term gland is defined as one or more cells making and secreting a certain product (secretion). Most secretions are water-based (aqueous) fluids, often containing proteins; however, some con-tain lipids or steroids.
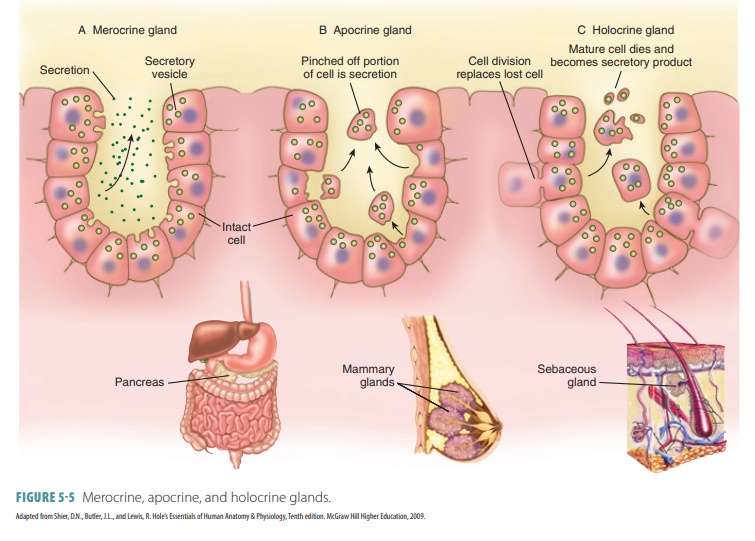
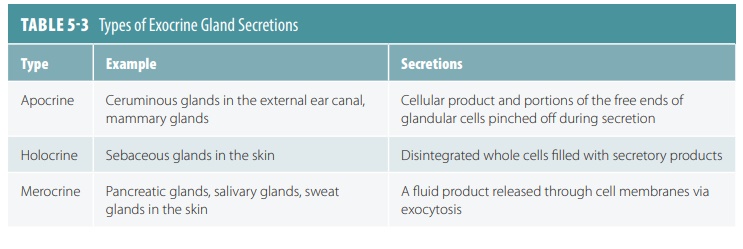
Exocrine glands produce exocrine, which is released onto epithelial surfaces, usually through tubular ducts. These ducts empty onto skin surfaces or epithelium that line internal passageways com-municating with the exterior. The three types of exocrine glands are merocrine, apocrine, and holo-crine (FIGURE 5-5). Merocrine glands release fluid by exocytosis, apocrine glands lose parts of their cell bodies during secretion, and holocrine glands release entire cells that disintegrate to release secre-tions. Merocrine secretion is the most common type. Watery perspiration is an example of mero-crine secretion. When the gland is unicellular, exo-cytosis is the process used for secretion. When the gland is multicellular, an epithelium-walled duct is used to transport secretions to the epithelial surface. The products of exocrine glands include mucus, oil, sweat, saliva, bile (in the liver), digestive enzymes (in the pancreas), and many others.
Unicellular exocrine glands are only exemplified by goblet and mucus cells. They are found in the linings of the respiratory and intestinal tracts, near colum-nar cells that have different functions. They produce mucin, which is a complex glycoprotein. It dissolves in water when secreted, forming mucus, which pro-tects and lubricates surfaces with its slimy texture. Mucus also traps foreign particles and microorgan-isms, and during swallowing, coats food and reduces friction. Although most multicellular epithelial glands are formed by inward growth (invagination) of an epithelial sheet into the underlying connective tissue, unicellular glands are simply scattered inside epithe-lial sheets. Most glands have ducts (initially), which are connections to epithelial sheets. These connections are tube-like in appearance. TABLE 5-3 lists the types of exocrine secretions.
Secretion is an active process that occurs as glandular cells obtain needed blood substances, and then chemically transform them. These substances are then discharged. The term secretion refers to the products of glands as well as the processes of these products being manufactured and released. Though multicellular exocrine glands may be simple secre-tory sheets, they are usually more complex, with a duct derived from epithelium and an acinus (secre-tory unit) made up of secretory cells. Supportive connective tissue usually surrounds the secretory unit, supplying it with nerve fibers and blood vessels. This forms afibrous capsule, extending into the gland to divide it into lobes . Examples of multicellular exo-crine glands include the mucin-secreting cells lining the stomach, protecting it from its own enzymes and acids. The majority of other multicellular exocrine glands lie inside pockets set back from the epithelial surface. Their secretions move through one or sev-eral ducts to the surface. These include the salivary glands, producing mucins and digestive enzymes. The structure of multicellular exocrine glands can be described as:
■■ Duct Structure: If there is a single duct that does not divide on its way to glandular cells, the gland is called “simple”; if the duct divides one or several times, the gland is called “compound.”
■■ Shape of the Gland’s Secretory Portion: The tubes are straight or coiled in glands with cells that form tubes—these are called “tubular”; if blind pockets are formed, the glands are called “alveolar” or “acinar”; if the secretory cells form tubes as well as pockets, the glands are called “tubuloalveolar” or “tubuloacinar.”
■■ Interaction Between Ducts and Glandular Areas: If several secretory areas—tubular or acinar—share a duct, the glandular area is “branched.” Most glands produce either exocrine or endocrine secretions, but the digestive tract, pancreas, and other complex organs produce both types of secretions. Therefore the pancreas is an example of mixed gland.
The merocrine type produces their secretions without any structural alteration, such as in the pan-creas, salivary glands, and most sweat glands. In the holocrine glands, the secretory cells collect their secretions until they rupture and then die. The only true examples of holocrine glands are the oil (sebaceous) glands of the skin. In order to continue to secrete, holocrine gland cells must be replaced via the division of stem cells. Apocrine glands also accumulate their products, but just beneath their free surfaces, with the apical portion pinching off to release secretory granules and tiny amounts of cytoplasm. The production of milk in the mammary glands combines both merocrine and apocrine secretions. These secretions leave cells mostly intact, so that they can continue secreting.
Endocrine glands eventually lose their ducts and are therefore termed ductless glands. They produce hormones, secreted by exocytosis, directly into the extracellular space. The hormones then enter the lymphatic fluid or blood, traveling to spe-cific target organs to prompt them to act in a cer-tain way. For example, intestinal hormones such as secretin may cause the pancreas to release digestive enzymes. Endocrine glands are usually not only compact and multicellular, but also consist of indi-vidual hormone-producing cells such as in the brain or mucosa of the digestive tract. This is described as the diffuse endocrine system. Endocrine secre-tions range from glycoproteins to steroids and from amino acids to peptides. Not all endocrine glands derive from epithelia.
1. List five important characteristics of the epithelial tissue.
2. Describe the type of epithelial organization that exists in the mouth, esophagus, anus, and vagina.
3. Describe transitional epithelium.
4. Identify goblet cells.
5. Explain the three types of exocrine glands.