Keys to Infection Prevention and Control
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Public Health Microbiology: Infection Prevention And Control
There is no single ‘silver bullet’ to solve the challenge of HCAI. Infection prevention and control requires a combination of actions and activities, each of which provides an essential component to the whole.
KEYS TO INFECTION PREVENTION AND CONTROL
There is no single ‘silver bullet’ to solve the challenge of HCAI.
Infection prevention and control requires a combination of actions and
activities, each of which provides an essential component to the whole.
Management And Organizational Commitment
The commitment of senior management to making infection prevention and
control a high priority sets a culture of a health of social care organization.
Management should monitor surveillance and audit data at all levels of the organization
(‘from board to ward’) and ensure that all the staff play their part. This
helps general a culture of pride in delivery of a quality service.
Surveillance
Up-to-date surveillance data on the incidence of key infections should be
collected, analysed and returned to the clinical units with minimum delay. In
this way the data are seen to be ‘real’ by the staff responsible for the care
of the patients. It is now mandatory in several countries to collect
surveillance data on MRSA infections (particularly bacteraemias), CDI, and some
type of surgical site infections. Although national data collection is focused
on whole hospitals or hospital groups, effective action within hospital depends
upon the data being assessed and acted upon in individual wards or other
clinical units, The essential nature of surveillance data is encapsulated in
the dictum ‘you have to measure it to manage it’.
Clinical Protocols
There are two main reasons why patients are at risk of developing an HCAI—their
underlying medical condition making them vulnerable to infections and the
treatment and clinical interventions they are subjected to. These interventions
often include invasive procedures that bypass the normal defences of the skin,
urinary and respiratory tract. It is, therefore, essential that clinical staff
exercise all due care and attention when performing these procedures. To this
end, an approach to clinical practice has been developed variously known as
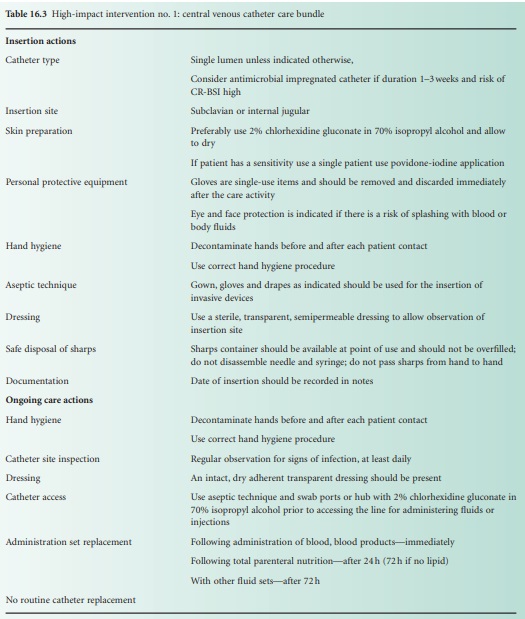
‘care bundles’ (in the USA in particular) and ‘high-impact interventions’ (HII;
the UK approach). These bundles are care protocols setting out in a simple
bullet-point format the five or six essential elements needed to minimize the
infection risk associated with the individual aseptic procedures. The aim is
for each element to be performed correctly on every occasion and the care
bundle/HII incorporates a simple audit tool for self-or peer-assessment on a
frequent and regular basis of the performance of the clinical staff doing those
procedures. The procedures that had been the main focus of the bundles comprise
the following invasive interventions:
central intravenous catheter insertion
and maintenance (Table 16.3)
•
peripheral intravenous cannula
insertion and maintenance
•
renal dialysis catheter insertion and
maintenance
•
surgical site infection (wound) care
•
care of ventilated patients
•
urinary catheter insertion and care.
For the HCAI programme in England these were set out in packages called
‘Saving Lives’ for secondary care and ‘Essential Steps’ for primary care use.
The packages were complemented by a care bundle for CDI and guidance presented
in a similar way based upon key elements for antibiotic prescribing, isolation
and cohorting of infected patients and the collection of blood cultures which
form the basis of the diagnosis of a bacteraemia.
Isolation And Segregation
One of the most basic and ancient approaches to preventing the spread of
infection (or ‘contagion’ in previous centuries) is isolation of the affected
patient. Segregation of infected patients from those vulnerable to infection
(including various forms of quarantine) is an essential element of all
infection prevention and control practice. It is particular important in HCAIs
where the infection often occurs in vulnerable or debilitated patients and in a
setting where transmission of infection between patients can occur readily. In
many hospitals, the number of single rooms available for patient isolation is
limited. The best use of the available rooms should be made for those with
infections, but where the capacity of single rooms is exceeded by the number of
cases of infection, it may then be necessary and appropriate for patients with
the same infection to be nursed together in a cohort ward physi-cally separated
from other ward areas and with dedicated staff who do not move between the
cohort ward and other clinical areas (i.e. cohorting should apply to nursing
staff as well as patients).
Hand Hygiene
One of the main routes of transmission
of HCAI pathogens such as MRSA is via the hands of healthcare workers as they
move between patients. For many years staff were recommended to wash their
hands between patient contacts and especially before and after performing
clinical procedures. However, very frequent hand washing is time consuming, can
damage the skin if done as often as should be required, and can also be quite
impracticable when there is inadequate provision of wash-hand basins for staff.
The answer to this problem has been the introduction of alcohol hand rubs that
can be used repeatedly and quickly at every point of patient contact. Alcohol
is highly effective against vegetative bacteria causing HCAI such as MRSA and
the Gram-negative bacteria. The hand rubs should be made available at every
patient bedside and in every clinical area, and at the entrance to cubicles and
single rooms. Personal dispensers can also be carried attached to a belt or the
clothing of healthcare staff to use as they move between patients. In many hospitals,
alcohol hand rub dispensers have also been placed at the hospital entrance
and/or at every ward entrance to emphasize to patients and visitors, as well as
staff, the absolute importance of hand hygiene. However, the crucial times and
places for hand hygiene relate to direct clinical contact with patients. The
hand hygiene campaign based on alcohol hand rubs has been promoted
internationally by the World Health Organization (WHO) and in the UK by the
National Patient Safety Agency through its ‘cleanyourhands’ campaign.
The WHO campaign high-lights the five opportunities (and requirements) for hand
hygiene:
• before touching a patient
• before clean/aseptic procedures
• after body fluid exposure/risk
• after touching a patient
• after touching patient surroundings.
The need for effective and appropriate hand hygiene has also been
included in all the care bundles/HIIs (see above).
However, in one area of infection
prevention and control, hand hygiene with alcohol hand rubs does not replace
the absolute requirement for hand washing: this is in relation to diarrhoeal
infections caused by norovirus or Cl. difficile. Alcohol
is not effective against norovirus or against the spores of Cl. difficile, so for these common diarrhoeal infections,
hand washing is essential before and after each patient contact or contact with
the environment around infective patients.
The audit of hand hygiene (alcohol hand rub and hand washing) is an
important part of monitoring compliance with clinical protocols for infection
prevention and control and should include direct observation of all grades of
healthcare staff and also measurement of the volume of alcohol hand rub and
liquid soaps used as a general proxy measurement of hand hygiene practice.
Environmental Cleanliness And Disinfection
Whenever there are problems or outbreaks
of HCAI, there is popular outcry over dirty hospitals, giving the impression
that environmental cleanliness equates to prevention of infection. Whereas
there is no question that hospitals and other healthcare premises should be clean
and that a clean environment promotes good healthcare practice, there is less
of a direct correlation between general cleanliness and rates of HCAI. However,
there is good evidence that bacteria and viruses from infected patients
contaminate the general environment around those patients from where they can
be picked up, e.g. on the hands, by other vulnerable patients or by healthcare
workers and transmitted to other patients. The evidence is particularly clear
with C. difficile spores, which can be found on all
environmental services in rooms where there are patients with CDI. They are particularly
prevalent around toilets, or on commodes, or near bed pan washers.
General hospital cleaning is based on a
detergent and water cleaning regimen, but when there are patients with known
HCAIs, it is advisable to supplement detergent cleaning with use of
environmental disinfectants. This is particularly the case in outbreaks of
norovirus or CDI. The most effective disinfectants for these viruses and for
the spores of Cl. difficile are those based
on chlorine-releasing agents. These should be used routinely in areas where
there are cases of norovirus or CDI.
Antibiotic Prescribing
Good antibiotic stewardship and the prudent
use of these valuable drugs is an important part of the prevention and control
of HCAI. Most bacterial HCAIs are caused by antibiotic-resistant organisms that
flourish under the selective pressure of antibiotic use, and because of the
fact that many of the bacteria are resistant to several different types of
antibiotic, even the use of individual antibiotics can select for bacteria
resistant to a wide range of agents. Furthermore, many of the resistance genes
are carried on transferable genetic elements that can transfer among bacterial
populations, particularly in a selective environment such as a hospital. There
are many examples of links between use of particular antibiotics and cases of
HCAI caused by resistant organisms. There are also more general links between
use of agents such as the fluoroquinolone antibiotics and the rising incidence
of MRSA colonization and infection. With CDI, the link is even more direct with
the use of broad-spectrum antibiotics being a key precipitating factor for this
disease. Outbreaks of CDI have been linked to widespread use of cephalosporins
and, more recently, fluoroquinolone antibiotics when the Cl. difficile strains such as ribotype 027 have
been specifically resistant to these agents.
All healthcare organizations should have antibiotic prescribing
protocols to promote and audit good stewardship. This is a requirement of the
statutory Code of Practice in England. The guidance in the ‘Saving Lives’
package recommends that antibiotic stewardship programme should have the
following elements:
• a prescribing and management policy for antimicrobials
• a strategy for implementing the policy
• an antimicrobial formulary and guidelines for antimicrobial treatment
and prophylaxis
• decision to prescribe should be clinically justified and recorded
• intravenous therapy should only be used for severe infections or where
oral antimicrobials are not appropriate
• intravenous antimicrobials should only be used for 2 days before
review and switch to an oral agent where possible and appropriate
• all antimicrobial prescriptions should include a stop date—generally a
maximum of 5–7 days without represcription
• daily review of antimicrobial treatment
• antimicrobial treatment reviewed on the basis of microbiological
results
• minimize the use of broad-spectrum antimicrobials
• a single dose at induction of anaesthesia for most operations where
antimicrobial prophylaxis is indicated
• training in implementing antimicrobial prescribing guidance for all
prescribers
Training And Education
The implementation of the range of infection prevention and control
practices in any health or social care setting can only be successful if there
is a comprehensive approach to staff education and training through which all
can learn that everyone has a role to play in preventing HCAI. Basic training
in infection prevention and control is mandatory for all staff in many hospitals
and healthcare settings in the UK, Europe and North America, usually with
regular (generally annual) required updates and specialist training for
particular professional groups. Completion of this training is generally a
requirement for successful appraisal and performance review for all staff.
Audit
Whereas surveillance of key HCAIs is necessary for monitoring the changing
pattern and the incidence of infections, audit of implementation of clinical
protocols is equally necessary for maintaining a high level of infection
prevention and control practice. There should be regular audits of hand hygiene
compliance, adherence to antibiotic prescribing guidelines and the implementation
of the clinical protocols in the care bundles/HIIs. The results of these audits
should be reviewed in a timely manner at all levels of management in the health
and social care organizations so that those implementing the protocols have
ownership of the procedures and their effective application. Performance
management at all levels depends upon a combination of the data from
surveillance of the infections and audit of the clinical practice.
Related Topics
