Leukocytes or white blood cells (WBCs)
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Blood
1. Explain the five types of WBCs. 2. Which type of WBCs are the most active phagocytes? 3. Explain the term white blood cell count. 4. Which type of WBCs turns into a macrophage in the tissues?
Formed Elements
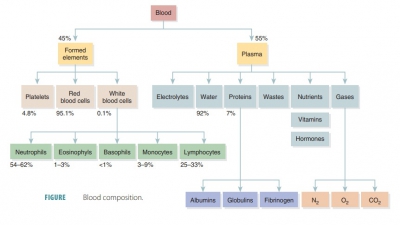
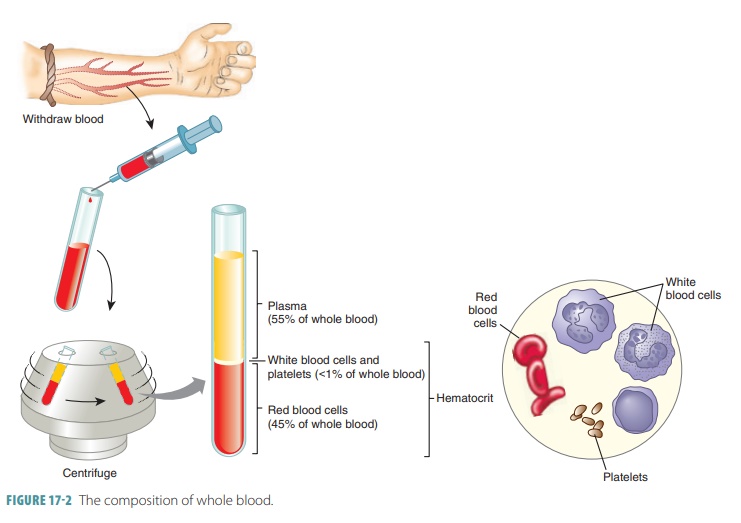
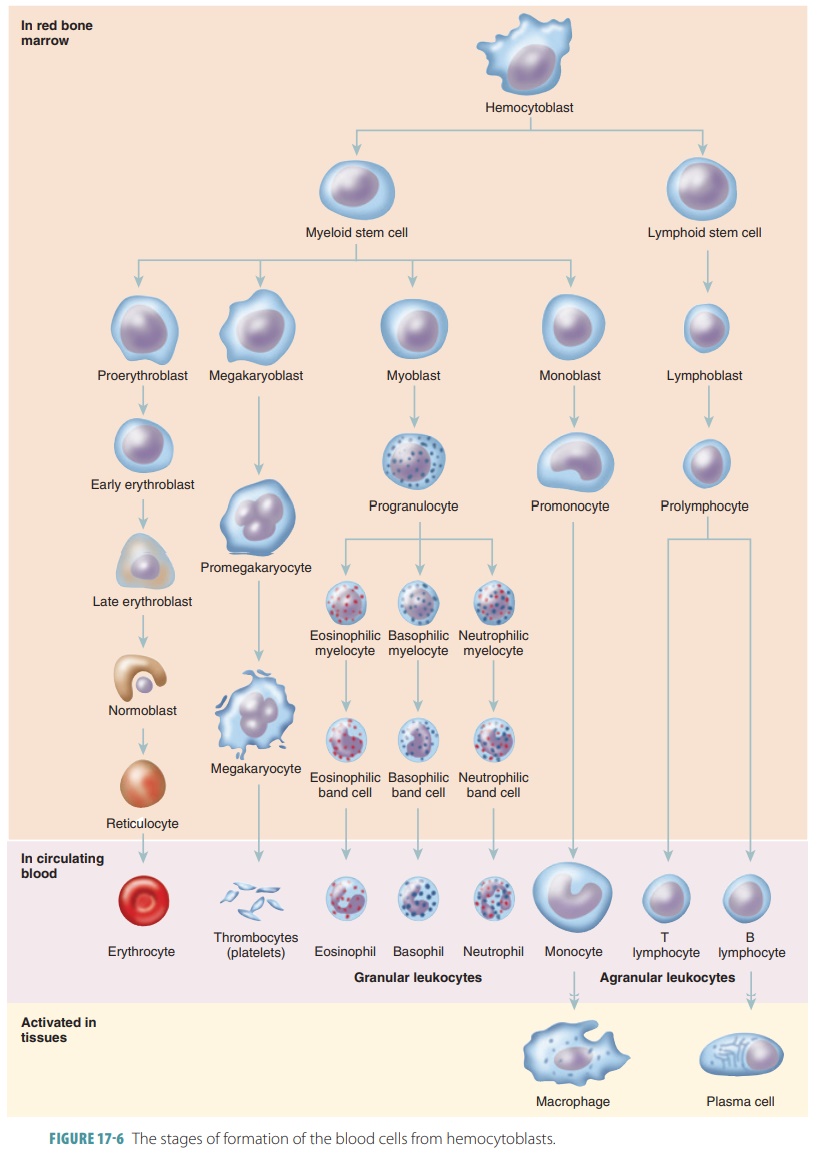
The formed elements of blood include erythrocytes, leukocytes, and platelets. Red blood cells make up about 45% of blood volume, which is known as the hematocrit. The RBCs have no nuclei or organelles,meaning that they are not considered “true cells.” Platelets are only cell fragments. Only leukocytes are complete cells. Leukocytes and platelets make up less than 1%. The remainder is plasma. Most blood cells do not divide. Instead they are replaced when stem cells continuously divide in the bone marrow. All formed elements arise from the hematocytoblasts, also called hematopoietic stem cells, which are undifferen-tiated precursor cells in the red bone marrow. Most formed elements only survive in the bloodstream for a few days. Different modes of maturation of formed elements exist. Once a cell becomes committed to a certain blood cell pathway, it is unable to change. Membrane surface receptors appear, which signal the cell’s commitment to one blood cell pathway. The receptors respond to specific growth factors or hor-mones. These assist the cell in becoming even more specialized. In a healthy male adult the normal hema-tocrit value is 47%, plus or minus 5%. In a healthy female adult, it is 42%, plus or minus 5%. Less than 1% of blood volume consists of platelets and leukocytes. Most of the remaining 55% of whole blood is made up by the plasma (FIGURE 17- 2). The components that make up whole blood can be separated or fractionated to be clinically analyzed.
Leukocytes
Leukocytes
or white
blood cells (WBCs) protectthe body against bacteria, viruses,
parasites, cancer cells, and toxins. They develop from hemocytoblasts in the
red bone marrow. Normally, there are 5000 to 10,000 WBCs in a microliter of
human blood. This is called a white blood
cell count, abbreviated as either WBCC
or WCC. White blood cell counts
are of inter-est to determine patients’ clinical conditions.
Percentages of the types of leukocytes in a blood sample are
listed in a differential WBC count,
which is useful to determine more exactly the type of condition. Bacterial
infections usually cause neutrophil counts to increase, whereas certain
parasitic infections cause the number of eosinophils to increase. AIDS causes
certain types of lymphocyte counts to drop sharply. The four primary
characteristics of circulating WBCs are as follows:
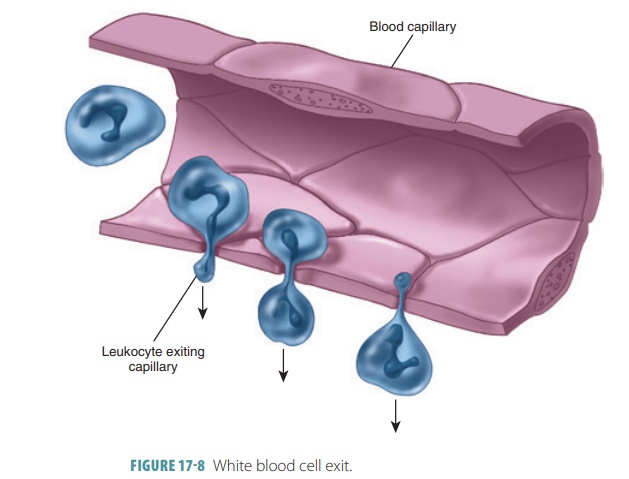
■■ All WBCs are able to migrate out of the blood-stream: When they contact and stick to the ves-sel walls, the process is known as margination; when they later interact with endothelial cells to become activated and squeeze between the cells to enter surrounding tissue, the process is known as emigration or diapedesis(FIGURE 17-8).
■■ All
WBCs can use amoeboid
motion: Thisis a gliding movement related to the flow of cytoplasm
into thin cellular processes extend-ing in the direction of movement; as a
result, WBCs move through endothelial linings into peripheral tissues.
■■ All
WBCs are attracted to certain chemical stim-uli: This is known as positive chemotaxis and moves WBCs to invading pathogens,
other active WBCs, and damaged tissues.
Generally, five types of WBCs are found in cir-culating blood, differing in size, cytoplasm nature, nucleus shape, and staining characteristics. Leuko-cytes with granular cytoplasm are called granulo-cytes; those without it are called agranulocytes.Most granulocytes, including eosinophils, baso-phils, and neutrophils, are about two times as large as a RBC. Like RBCs, granulocytes develop in the red bone marrow but only live about 12 hours. To various degrees, all granulocytes are phagocytes. Agranulocytes include lymphocytes and mono-cytes, which lack visible cytoplasmic granules. Their nuclei are usually kidney shaped or spherical. The process of lymphocyte production is known as lymphopoiesis.
Neutrophils
Neutrophils have small granules that appear lightpurple in neutral stain. Older neutrophils are some-times called segs and have lobed nuclei in three to six segments connected by thin chromatin strands. Because of the structure of the nucleus, a neutrophil may be referred to as polymorphonuclear, or sim-ply as a poly. Younger neutrophils have C-shaped nuclei and are called bands (Figure 17-6). Neutro-phils make up 50% to 70% of the leukocytes in most adults. Neutrophils are highly mobile and, because of this, they are usually the first type of WBCs to arrive at an injury site. They are very active cells in attacking and digesting bacteria. An acute bac-terial infection causes the numbers of neutrophils to greatly increase. They are active phagocytes that are chemically attracted to areas of inflam-mation and primarily target bacteria and also cer-tain fungi. The process of this attraction is called a respiratory burst, in which the cells metabolizeoxygen. This creates strong oxidizing substances such as hydrogen peroxide and bleach, which kill the invaders. When granules containing of neutro-phils defensins merge with a phagosome containing microbe, defensin-mediated lysis occurs. Spear-like structures are formed by the defensins, which make holes in the membranes of the ingested patho-gens. Neutrophils are approximately twice as large as erythrocytes. The process of reducing the number of granules in cytoplasm via interaction with defensins is known as degranulation.
Most neutrophils have a short life span, surviving in the
bloodstream for only about 10 hours. When they actively engulf debris or
pathogens, they may last for only up to 30 minutes. Each neutrophil dies after
engulfing between 1 and 2 dozen bacteria. As a neu-trophil breaks down, it
releases chemicals that attract other neutrophils to the site. A mixture of
dead neu-trophils and cellular debris forms pus,
which is associ-ated with infected wounds. The production of WBCs is known as leukopoiesis.
Eosinophils
Eosinophils
have coarse, same-sized gran-ules that appear dark red in the
acidic eosin stain (Figure 17-6). Because the granules also stain with other
acid types, they are sometimes called aci-dophils.
Their nuclei usually have just two lobes,which is called bilobed, and they make up only 2% to 4% of circulating leukocytes.
The eosinophil granules resemble lysosomes and are filled with a specific type
of digestive enzymes. Eosinophils are similar in size to neutrophils.
Eosinophils are partic-ularly effective against multicellular parasites, such
as parasitic flukes, including flatworms and tape-worms, and roundworms,
including hookworms and pinworms, which are too big to engulf. The number of
circulating eosinophils increases dramat-ically during a parasitic infection.
Eosinophils also increase in number during an allergic reaction and asthmatic
conditions.
Basophils
Basophils
are similar to neutrophils or eosinophils.However, they are more
irregular and become deep blue or purple in basic stain (Figure 17-6).
Basophils usually account for less than 1% of circulating leu-kocytes. They
migrate to sites of injury and cross the capillary endothelium to accumulate in
the damaged tissues, where they release the inflammatory chemi-cal histamine, which dilates blood vessels.
Histamine also attracts other WBCs to areas of inflammation.
Therefore, antihistamines
work by opposing this effect. Basophils also release heparin, a compound that prevents blood clotting. Stimulated
basophils release these chemicals into the interstitial fluids. These chemicals
enhance the local inflammation ini-tiated by mast cells. Although the same compounds are released by mast cells in
damaged connective tis-sues, both mast cells and basophils originate
differ-ently from each other. The cytoplasm of basophils holds
histamine-containing granules that are large and coarse. These granules have an
affinity for basic types of dye. The nuclei of basophils are usually “S” or “U”
shaped and have either one or two visible constrictions. The nuclei of mast
cells are more oval in shape instead of being lobed. Both mast cells and
basophils bind to immunoglobulin E, which is the antibody that causes histamine
release.
Monocytes
Monocytes
are agranulocytes that are the larg-est type of blood cells, up to
three times as large as RBCs (Figure 17-6). Their average diameter is 18 micrometers
(μm). They have nuclei that may be either kidney- shaped, lobed, oval, or
round. Their cytoplasm is abundant and pale-blue in color, whereas their
“U”-shaped or kidney -shaped nuclei stain dark purple. Monocytes usually make
up 3% to 8% of circulating leukocytes and live for either weeks or months. A
single monocyte remains in the circu-lation for only about 24 hours before it
enters the peripheral tissues. There it becomes a tissue macro-phage. Macrophages are aggressive phagocytes thatare
very important in the defense against viruses, chronic infections such as
tuberculosis, and certain intracellular bacterial parasites. They often attempt
to engulf items as large as themselves. When they are involved in phagocytosis,
they release chemicals that attract and stimulate neutrophils, monocytes, and other
phagocytic cells.
Lymphocytes
Lymphocytes
are agranulocytes that are usually onlya little larger than RBCs.
They have large, round nuclei inside a thin cytoplasm rim (Figure 17-6).
Lymphocytes make up between 20% and 30% of circulating leukocytes and may live
for years. They continuously migrate from the bloodstream, through the
peripheral tissues, and back to the bloodstream. They are the second most
abun-dant leukocytes in the blood. Circulating
lymphocytes represent a very small fraction of all lymphocytes. At any
particular moment most of the body’s lymphocytes are in other connective
tissues and organs of the lymphatic sys-tem. Their nuclei stain dark purple and
appear so large they take up nearly all of the cell volume. Lymphocytes are
named because of their close association with the lymph nodes, spleen, thymus,
and the red bone marrow.
The circulating blood contains two functional classes of
lymphocytes:
■■B cells or
B lymphocytes are responsible forhumoral immunity, which is a specific defense
mechanism that involves the production of anti-bodies. Activated B cells
differentiate into plasmacells,
which are specialized to secrete antibodies.
■■ T cells or
T lymphocytes are responsible for cell-mediated immunity and activate B cells.
They act directly against tumor cells and virus-infected cells.
1. Explain the five types of WBCs.
2. Which type of WBCs are the most active phagocytes?
3. Explain the term white blood cell count.
4. Which type of WBCs turns into a macrophage in the tissues?