Other Glands, Organs, or Tissues
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Endocrine System
Other organs in the body produce hormones, but their main functions are not to produce these hormones. These structures include the thymus, reproductive organs, digestive glands, pancreas, heart, kidneys, adipose tissue, skeleton, and skin.
Other
Glands, Organs, or Tissues
Other organs in the body produce hormones, but their main
functions are not to produce these hormones. These structures include the
thymus, reproductive organs, digestive glands, pancreas, heart, kidneys,
adipose tissue, skeleton, and skin.
Thymus
The thymus, located
deep inside the mediastinum posterior to the sternum between the lungs, is
larger in children than in adults. It shrinks with age and is import-ant in
early immunity. The lobulated thymus secretes hormones called thymosins, affecting production and
differentiation of lymphocytes as well as thymulin and thymopoietins.
Although considered hormones, thesesubstances primarily act locally as paracrines.
By the time of old age, the thymus has changed to a structure made
of adipose and fibrous connective tissues.
Reproductive Organs
The reproductive organs important for hormone secretion
include the ovaries, which produce estrogens and progesterone; the testes, which
produce testosterone
in
their interstitial cells; and the placenta, which pro-duces estrogens,
progesterone, and gonadotropins. The
placenta is a temporary endocrine organ that sustains the fetus during
pregnancy and secretes steroid and protein hormones that regulate pregnancy.
Gonado-tropins regulate the release of gonadal hormones. Estro-gens help the
reproductive organs to mature and cause the appearance of the secondary sex
characteristics of females at the time of puberty. Along with progester-one,
estrogens promote the menstrual cycle and breast development. In males at
puberty, testosterone initiates maturation of reproductive organs and
appearance of secondary sex characteristics as well as sex drive. It is also
required for normal production of sperm and to maintain reproductive organs in
adult males.
Digestive Glands
The digestive glands that secrete hormones are found in the
linings of the stomach and small intestine. For example, the stomach secretes gastrin and ghrelin. The duodenum releases secretin, cholecystokinin, and incretins.
Pancreas
The pancreas
functions as two things: an exocrine gland secreting digestive juice and an
endocrine gland releasing hormones. It is an elongated, slightly flattened
organ posterior to the stomach, behind the parietal peritoneum. It is joined to
the duodenum of the small intestine, transporting digestive juice into the
intestine (FIGURE
16-18).
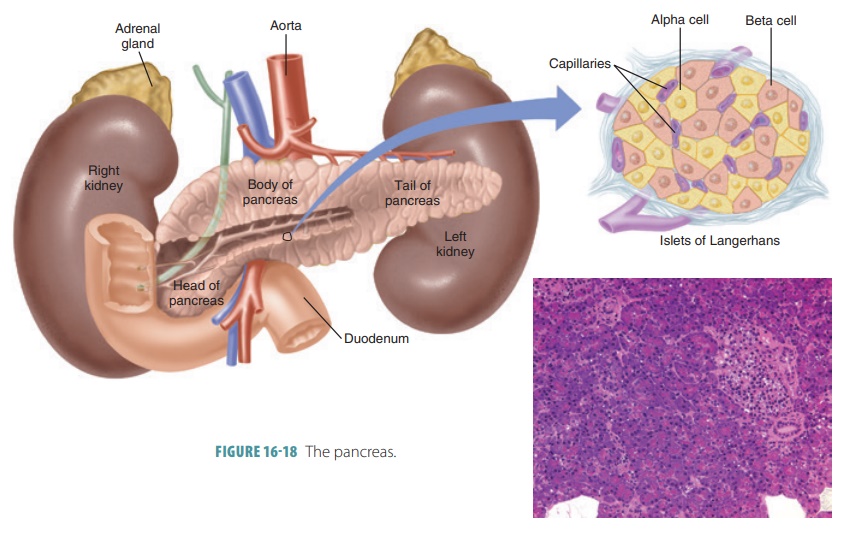
The endocrine part of the pancreas consists of groups of
cells called pancreatic
islets or islets
ofLangerhans. Of these cells,alpha
cellssecrete the hor-mone glucagon and beta cells secrete the hormone insulin. Delta cells produce a peptide hormone
that is identical to GH-inhibiting
hormone. It suppresses release of glucagon and insulin and slows food
absorp-tion and enzyme secretion in the digestive tract. F cells produce pancreatic
polypeptide, a hormone that inhib-its gallbladder contractions while
regulating pancre-atic enzyme production. Glucagon, a 29-amino-acid polypeptide, stimulates the liver to
break down glyco-gen in the process known as glycogenolysis and to con-vert certain noncarbohydrates, including
amino acids, into glucose in the process called gluconeogenesis. This raises the blood sugar concentration
much more effectively than epinephrine is able to do. Gluca-gon secretion is
regulated by negative feedback and prevents hypoglycemia from occurring when
glu-cose concentration is relatively low. Glucagon is so powerful that just
one molecule can trigger the release of 100 million glucose molecules into the
bloodstream. Humoral stimuli cause the alpha cells to secrete gluca-gon,
although stimulation from the sympathetic ner-vous system and rising amino acid
levels also play a role. The release of glucagon is suppressed by insulin,
somatostatin, and rising blood glucose levels.
Insulin,
a 51-amino-acid protein, works in amanner opposite of glucagon by stimulating
the liver to form glycogen from glucose and inhibiting conver-sion of
noncarbohydrates into glucose. It consists of two amino acid chains that are
linked by disulfide or -S-S- bonds
and is synthesized as part ofproinsulin,
alarger polypeptide chain. Insulin decreases blood glu-cose concentration,
promotes amino acid transport into cells, increases protein synthesis, and
stimulates adipose cells to make and store fat. Insulin secretion is also
controlled by negative feedback and insulin pre-vents high blood glucose
concentrations by promot-ing glycogen formation. Insulin secretion decreases as
glucose concentrations fall. Just after we eat, insulin lowers blood glucose
levels and also influences pro-tein and fat metabolism. Insulin enhances
membrane transport of glucose into primarily fat and muscle cells, inhibits
glycogen breakdown into glucose, and inhibits conversion of fats or amino acids
to glucose.
Because the brain, kidneys, and liver have easy access to
blood glucose, no matter what the insulin level currently is, insulin is not
required for glucose entry into these organs. In the brain it plays roles in
feeding behaviors, learning, memory, and neuronal development. Insulin and
glucagon function together to maintain stable blood glucose concentration, even
though the amount of carbohydrates ingested by a person may vary widely. Nerve
cells are partially sen-sitive to blood glucose concentration changes. Such
changes can alter brain functions.
Prior to the development of type 2 diabetes, most patients develop prediabetes, which is blood glu-cose levels that are higher than
normal but not high enough to be diagnosed as diabetes. Prediabetes may be
referred to as impaired glucose tolerance
or impairedfasting glucose. This
condition increases the risk fordeveloping type 2 diabetes and cardiovascular
disease. Prediabetes exists when the average blood glucose via the A1C test is revealed to be between 5.7%
and 6.4%. Prediabetes can also be diagnosed via a fasting plasmaglucose test, oral glucose tolerance test, or a random plasma glucose test. There may
be no clear symptomsof prediabetes. Early treatment is able to return blood
glucose levels to normal. It is possible to lower the risk for type 2 diabetes
by losing 7% of body weight and by exercising moderately such as brisk walking
for 30 minutes a day, five days per week.
Heart
The atria of the heart secrete atrial natriuretic peptide
(ANP), which stimulates urinary sodium excretion. This peptide decreases sodium
in the extracellular fluid, reducing blood pressure and volume. It also
reduces the sensation of thirst, and suppresses ADH secretion.
Kidneys
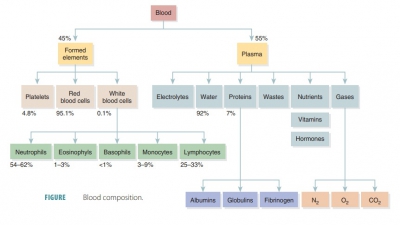
The kidneys secrete erythropoietin, which is a red blood cell GH.
Erythropoietin is a glycoprotein hor-mone that causes the bone marrow to
increase pro-duction of red blood cells. They also release renin, initiating the renin–angiotensin–aldosterone mech-anism of
aldosterone release. Therefore, the enzyme renin is responsible for the
activation of angiotensin.
Adipose Tissue
The adipose cells release leptin, which is a peptide hormone. Leptin functions to inform the
body how much stored fat is present that may be used for energy. Blood levels
of leptin are higher when there is more stored fat. It helps to control
appetite and stimulate increased expenditure of energy. Two other adipose cell
hormones play different roles. Resistin is an
insu-lin antagonist, whereas adiponectin enhances
the sensitivity to insulin.
Skeleton
The bones via their osteoblasts secrete osteocalcin, which causes pancreatic beta cells
to divide, secreting more insulin. Osteocalcin restricts fat storage by the
adipocytes and triggers adiponectin release, improv-ing handling of glucose and
reducing body fat. Insulin encourages the conversion of inactive osteocalcin to
active osteocalcin in the bones. This forms a two-way mode of communication
between the bones and the pancreas. In type 2 diabetes, osteocalcin levels are
low. Increasing the level of osteocalcin may be an effective form of treatment
for type 2 diabetes.
Skin
In the skin, cholecalciferol, which is
an inactive form of vitamin D3, is produced because of ultraviolet
radi-ation exposure. Eventually, cholecalciferol becomes fully activated by the
kidneys, forming calcitriol, which is
required to regulate how intestinal cells absorb calcium from the diet. Without
calcitriol, the bones soften and weaken. Osteocalcin is also involved in
regulating the mineralization of the bones and teeth. Vitamin D is involved
with immune functions. It also decreases inflammation and can reduce risks for
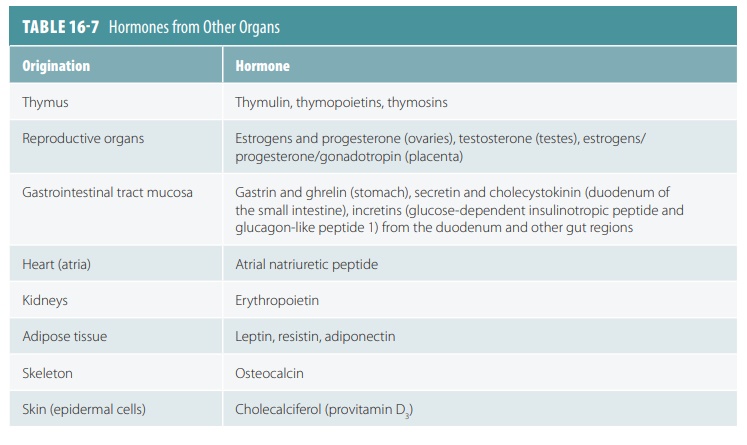
cancer. TABLE 16-7
illustrates the hormones pro-duced by other organs.