Physiology of the Female Reproductive System
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Reproductive System
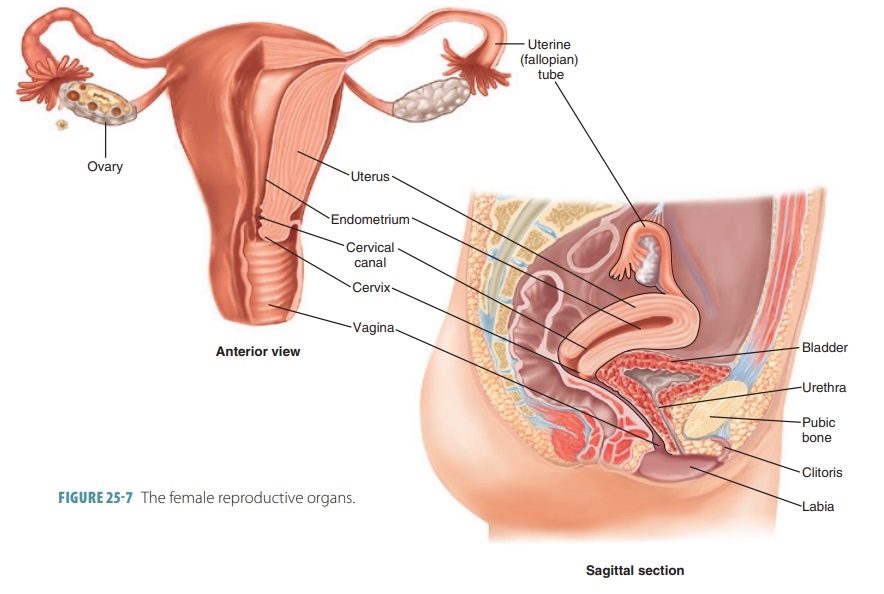
Physiology and Function of the Female Reproductive System : Oogenesis, Ovarian Cycle, Follicular Phase, Ovulation, Luteal Phase, Hormonal Regulation of the Ovarian Cycle, Uterine Cycle, Estrogen, Progesterone, and Female Reproductive Function, Female Sexual Response
Physiology
of the Female Reproductive System
Females release egg cells only from puberty to meno-pause,
which occurs on average at around age 51. Although today we know that egg stem
cells continue to survive throughout life, it has not yet been proven that the
cells are viable for reproduction. Physiology of the female reproductive system
includes the pro-cesses of oogenesis, the ovarian cycle, hormonal reg-ulation,
the uterine or menstrual cycle, and
the female sexual response.
Oogenesis
Oogenesis
is the process of egg cell formation, pro-ducing female sex cells.
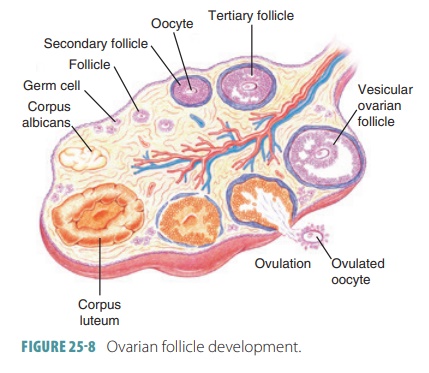
During the fetal period, the diploid stem cells of the ovaries or oogonia multiply quickly via
mitosis. Eventually, primordial
follicles appear, whereas the oogonia change into primary oocytes. They are surrounded by
one layer of flat-tened follicle cells.
The first meiotic division is begun by the primary oocytes. However, they stall
in the late part of prophase I and do
not complete their division.
At birth, a female infant is believed to have a cer-tain
finite amount of primary oocytes. Although there were seven million oocytes
originally, at birth about one million have survived programmed death. They are
located in the cortical region of each immature ovary. By puberty,
approximately 300,000 oocytes remain. Primordial follicles change into an
enlarging collection of primary
follicles over time. This process starts during the fetal period and
continues until there are no more primordial follicles. At this time, meno-pause begins. In rare conditions,
menopause occurs before age 40 and is
known as premature menopause.
Oogenesis in the ovaries at puberty takes years for
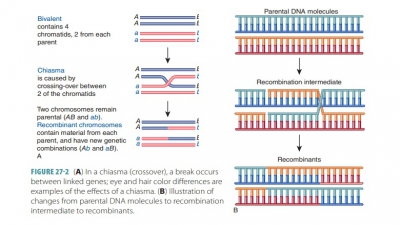
completion. During this time, some primary oocytes continue meiosis, with 23
chromosomes in their nuclei like their parent cells. When they divide, the
distribution of the oocyte cytoplasm is unequal. The cells that result are
different in size. FSH protects small numbers of growing follicles from
programmed cell death every month. In every cycle, one of these fol-licles
becomes the dominant
follicle and continues meiosis I. This eventually produces two
haploid cells, with each having 23 replicated chromosomes, which are very
different in size.
The secondary
oocyte is large, whereas the first polar
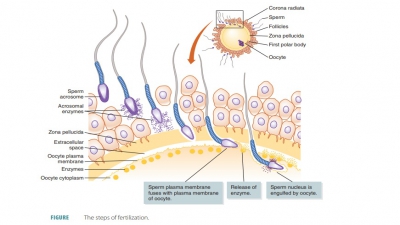
body is small (FIGURE 25-11). The large secondary oocyte
can be fertilized by a sperm cell. Maturing folli-cles that were
not selected undergo atresia. These events mean that the polar body receives
nearly no cytoplasm or organelles. A spindle forms at the edge of the oocyte,
and a small nipple-like structure also appears. The chromosomes from the polar
body move into it.
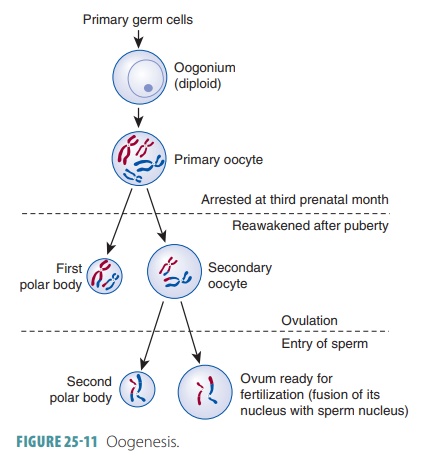
The first polar body may continually develop and undergo
meiosis II, with two smaller polar bodies being produced. The secondary oocyte
stops func-tioning in metaphase II, and this is the cell that is ovulated. When
no sperm penetrates an ovulated sec-ondary oocyte, it deteriorates. However, if
penetration by a sperm occurs, the oocyte completes meiosis II quickly. This
produces a tinysecond
polar body and a large fertilized egg cell called a zygote. The joining of the egg and sperm nuclei constitutes fertilization.
The polar bodies soon degenerate. They allow for production
of egg cells with massive amounts of cyto-plasm and abundant organelles that
carry the zygote through its first cell divisions, still with the right num-ber
of chromosomes.
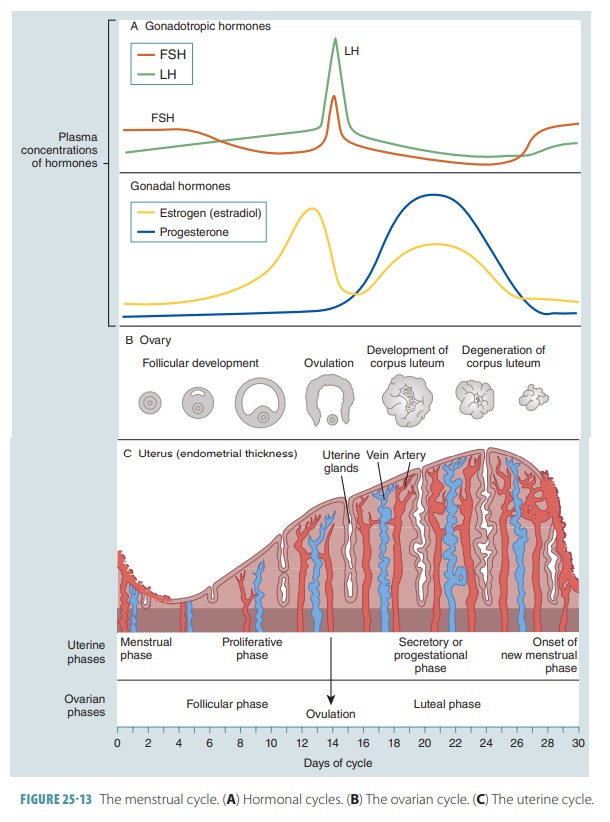
Ovarian Cycle
The ovarian cycle
is the monthly series of events linked to maturation of an egg. It has two
consecutive phases: the follicular phase
and the luteal phase. In the
follic-ular phase, the dominant follicle is selected and starts to secrete
significant amounts of estrogens. This lasts from day one to 14, typically
followed by ovulation.
Interestingly, only 10% to 15% of women actu-ally have 28-day cycles. The ovarian cycle may range between 21 and 40 days in actuality. When this is the case, there are variations in the length of the follicu-lar phase and the timing of actual ovulation. However, the luteal phase always begins on the 14th day after ovulation and lasts to the cycle’s end.
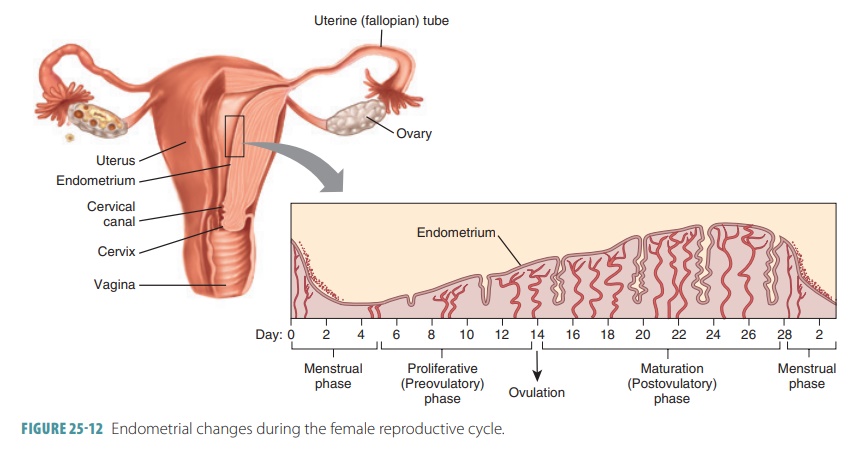
In younger females, estrogens stimulate devel-opment of the
secondary sex characteristics. They maintain and develop these characteristics
as time passes. Increased estrogens during the first week of a reproductive
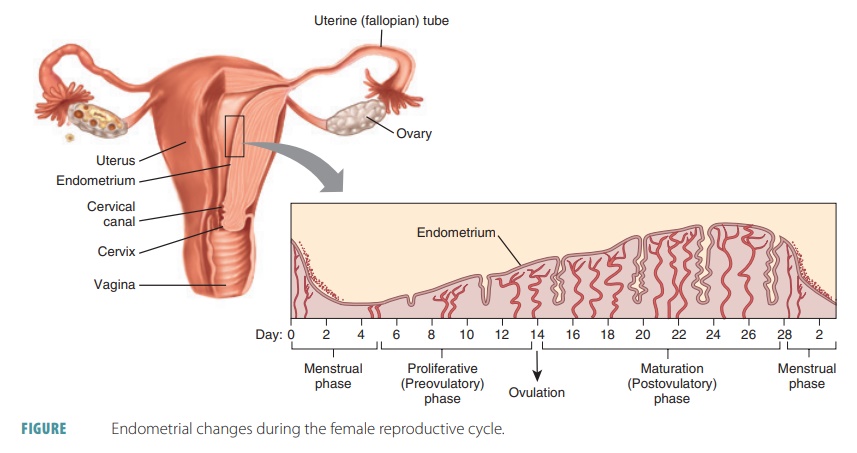
cycle thicken the glandular endo-metrium of the uterine lining. This is known
as the proliferative phase. FIGURE
25-12 shows the various phases of the female reproductive
cycle.
Follicular Phase
The first part of the follicular
phase is known as the pre-antral
phase, which is not dependent on gonadotropin. This is when cytokines, growth factors, and other intra-follicular
paracrines control development of oocytes and follicles. The second antral phase is controlled by FSH and
LH. Activated follicles grow greatly, and the primary oocyte in the dominant
follicle restarts meiosis I.
In the follicular phase,
the developing follicle matures, and by approximately day 14 of the cycle, it
appears on the surface of the ovary as a blister-like bulge. Follicular cells
inside the follicle loosen and fol-licular fluid accumulates. The maturing
follicle secretes estrogens that inhibit the anterior pituitary from releasing
LH but allow it to be stored. Anterior pituitary cells become more sensitive
to GnRH secreted from the hypothalamus in rhythmic pulses. The stored LH is
released, weakening and rupturing the bulging follicu-lar wall. This sends the
secondary oocyte and fluid from the ovary in the process of ovulation. The space con-taining the
follicular fluid fills with blood, which clots.
Near the end of follicle maturation, the primary oocyte finishes meiosis I. A secondary oocyte and first polar body are formed, readying the cycle for ovulation. The granulosa cells signal the oocyte to stop the comple-tion of meiosis. Follicle growth from the primordial stage to this point is believed to take about one year. Therefore, each follicle that ovulates was actually beginning to grow between 10 and 12 ovarian cycles previously.
Ovulation
The primary oocyte undergoes oogenesis, developing a
secondary oocyte and first polar body. This is known as ovulation. This process releases these
developed structures along with one or two layers of follicular cells from the
mature follicle. Anterior pituitary gland hormones trigger ovulation, swelling
the mature folli-cle while weakening its wall. The wall ruptures, allow-ing the
fluid and secondary oocyte to be expelled into the peritoneal cavity while
still surrounded by the corona radiata. There may be a slight pain in the lower
abdomen at the moment this occurs. Although the cause is unknown, it may be due
to extreme stretching of the ovarian wall and irritation of the peritoneum by
blood or fluid from the ruptured follicle.
Every adult woman has several follicles that are continually
at different stages of maturation. Because of this, one follicle is at the
perfect stage of maturation when LH stimulates ovulation. Antral follicles
sur-vive because of FSH, which helps to select the dom-inant follicle, although
this actual process is not fully understood. It is believed to add the largest
amount of gonadotropin receptors, attaining the most FSH sensitivity at the
fastest rate. Other follicles undergo apoptosis and are reabsorbed by the body.
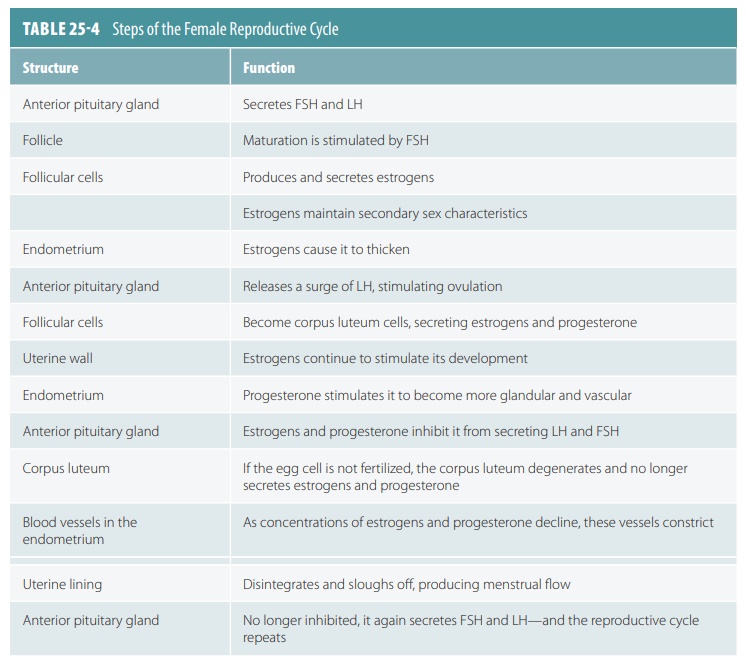
Luteal Phase
The follicular cells enlarge to form a temporary corpus luteum after
the ruptured follicle or corpus hemorrhagicum
is absorbed. Thisluteal
phase is when the corpus luteum
is active. Corpus luteum cells secrete large amounts of progesterone and
estrogens during the last half of the cycle, and blood proges-terone
concentration increases sharply. Progesterone causes the endometrium to become
more vascular and glandular while stimulating uterine gland secre-tion of more
lipids and glycogen. This is known as the secretory
phase. Endometrial tissues fill with fluids that are made up of nutrients and electrolytes, which support
embryo development.
LH and FSH release is then inhibited, and no other follicles
develop when the corpus luteum is active. If no egg cell is fertilized, on the
24th day of the cycle the corpus luteum begins to degenerate, to be replaced by
connective tissue. The leftover remnant is called a cor-pus albicans. Then, estrogens and progesterone decline in level, and the endometrium
constricts its blood vessels. The uterine lining starts to disintegrate and
slough off. Damaged capillaries create a flow of blood and cellular debris,
which passes through the vagina. This is called the menstrual flow. It usually begins approximately on the 28th day of
the cycle, continuing for three to five days while estrogen concentrations are
low. TABLE 25-4
summarizes the female reproduc-tive cycle. However, if the oocyte is
fertilized, resulting in pregnancy, the corpus luteum continues to develop
until the placenta assumes its hormone production duties. This occurs in
approximately three months.
1. Distinguish the function of estrogens and progesterone in
the female reproductive system.
2. What is menarche?
3. What is a
corpus luteum?
Hormonal Regulation of the Ovarian Cycle
The female reproductive system is controlled by hor-mones,
involving interplay between the pituitary gland and gonadal secretions. Female
hormonal regu-lation is much more complicated than male hormonal regulation
because it coordinates both the ovarian and uterine cycles.
The maturation of female sex cells, develop-ment and
maintenance of secondary sex character-istics, and changes during the monthly
reproductive cycle is controlled by the hypothalamus, anterior pituitary gland,
and ovaries. Until about age 10, the female body is reproductively immature.
When the hypothalamus begins to secrete more GnRH, the anterior pituitary
releases FSH and LH, controlling female sex cell maturation and producing
female sex hormones. The ovaries, adrenal cortices, and placenta secrete sex
hormones during pregnancy that include estrogens and progesterone. The most
abundant of the estrogens is estradiol,
fol-lowed by estrone and estriol. Also, onset of puberty is
linked to amounts of adipose tissue. Leptin
is the hormone that informs the hypothalamus about these amounts. Puberty is
delayed if blood levels of lipids and leptin are low.
In childhood, the ovaries are growing with con-tinuous
secretion of only a small amount of estrogens. These keep the hypothalamus from
releasing GnRH. With normal leptin levels, the hypothalamus becomes less
sensitive to estrogen as puberty approaches. It starts to release GnRH
rhythmically, with this hor-mone stimulating the anterior pituitary to release
FSH and LH. As a result, the ovaries begin to secrete estrogens and other
hormones in higher quanti-ties. Gonadotropin levels increase continuously for
approximately four years. Females at this stage are still not ovulating and
pregnancy is not possible. In non-pregnant females, the ovaries are the main source
of estrogens. Hormonal interactions stabilize eventually and the adult ovarian
cycle begins.
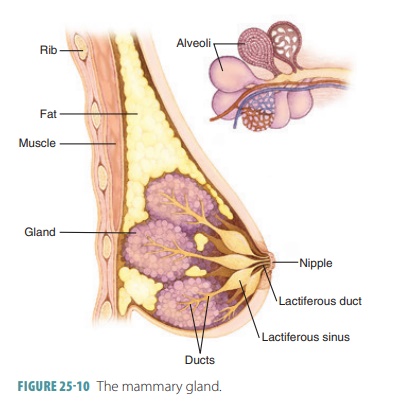
Estrogens and related hormones stimulate enlargement of
accessory sex organs and develop and maintain the female secondary sex
characteristics:
■■ Development of breasts and the
mammary gland ductile systems
■■ Increasing adipose tissue
deposition in the subcutaneous layer, breasts, thighs, and buttocks
■■ Increasing skin vascularization
The ovaries are also the main source of progesterone in
nonpregnant females. Progesterone promotes uterine changes during the monthly
cycle, affects the mammary glands, and helps regulate gonadotropin secretion.
Con-centrations of androgen in females at puberty produce different changes,
including increased hair growth in the pubic region and armpits. The female
skeleton responds to low androgen concentration by narrowing the shoul-ders and
widening the hips.
Uterine Cycle
Controlled by estrogen, the uterine glands, blood vessels,
and epithelium change with the phases of the menstrual cycle, which is also called
the uterine cycle. It
is coordinated with the ovarian cycle. The changes in this cycle can be divided
up into a menstrual phase, proliferative or preovulatory phase, and a
secretory, postovulatory phase (FIGURE
25-13).
The menstrual phase
occurs during days one to five. The uterus sheds all except the deepest part of
its endometrium. Ovarian hormones are at their low-est normal levels, but
gonadotropins are increasing. The functional layer of the endometrium is thick
and depends on hormones. It detaches from the uterine wall, resulting in
bleeding for three to five days. Blood and detached tissue flow out through the
vagina. By day five, more estrogen is being produced by the ovarian follicles
as they grow.
The proliferative
phase occurs during days six to 14. The endometrium is rebuilt, influenced
by the rise of estrogens in the blood. Its basal layer gener-ates a new
functional layer, which thickens. Its glands increase in size and the spiral
arteries become more numerous. As a result, the endometrium returns to its
earlier state: It is soft, smooth, thick, and well supplied with blood vessels.
Estrogens cause the endometrial cells to synthesize progesterone receptors.
This makes them ready for interaction with progesterone.
Cervical mucus is usually sticky and thick. However, as
estrogen levels increase, it thins to form channels allowing sperm to pass into
the uterus. Ovu-lation takes only five minutes, occurring on or about day 14 in
the ovary as a response to a sudden release of LH by the anterior pituitary.
The ruptured follicle is converted by LH to a corpus luteum.
The secretory phase
occurs during days 15–28. This phase is not as variable as the others. The
endo-metrium is readied for an embryo to be implanted. The corpus luteum
increases progesterone levels, which affect the endometrium by causing the
spiral arteries to become more extensive and by converting the functional layer
into a secretory mucosa. In an effort to sustain an embryo, the endometrial
glands become larger and coiled. They secrete nutrients into the uterine
cavity.
A cervical plug is
formed as progesterone levels rise and make the cervical mucus viscous once
more. The plug helps to block entry of pathogens, other for-eign materials, and
sperm. Progesterone also helps to ready the uterus for the task of supporting
an embryo. Increasing levels of progesterone and estrogen inhibit LH release
from the anterior pituitary.
When no fertilization occurs, the corpus luteum degenerates, LH blood levels are reduced, progester-one levels are decreased, and the endometrium no longer has the hormones it needs to support a preg-nancy. Its spiral arteries become kinked and spasm. The ischemic endometrial cells die because of a lack of oxygen and nutrients. The glands regress, preparing menstruation to begin on day 28. The spiral arteries constrict for a final time, suddenly relaxing and open-ing wide. Blood flows into the weak capillary beds and they fragment. The functional layer is then sloughed off and the uterine cycle begins again with this new menstrual flow.
1. List the hormones most important for the regulation of the
ovarian cycle.
2. Which hormone, if lower than normal, will delay the onset
of puberty?
3. Explain the three phases of the uterine cycle.
Estrogen, Progesterone, and Female Reproductive Function
Estrogens are to females what testosterone is to males. Both
these hormones generate reproductive function. Two things happen when estrogen
lev-els rise during puberty in a female’s body: Oogen-esis is promoted with
follicle growth in the ovaries and anabolic effects occur in the female
reproduc-tive tract. The tract is readied for supporting a pregnancy, with
enhanced motility occurring in the uterine tubes and uterus. There is
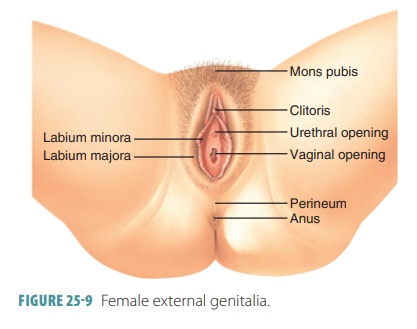
thickening of the vaginal mucosa and maturation of the external genitalia.
Because of estrogens, girls between the ages of 11 and 12 experience “growth
spurts,” which are more dramatic than those seen in boys. However, this is a
shorter term process for females, because increasing estrogen levels also cause
a faster closure of the epiphy-ses of the long bones. Girls usually reach their
full height between the ages of 13 and 15, whereas boys usually reach their
full height between the ages of 15 and 19.
Secondary sex characteristics included by estro-gen include
breast development; widening and lightening of the pelvis for future
childbirth; and increased deposition of subcutaneous fat, mostly in the breasts
and hips. The various types of estrogen also help to maintain low total blood
cholesterol lev-els and high -density lipoprotein levels. They facili-tate
calcium uptake, keeping the skeleton’s density intact. All these effects begin
in puberty, yet are not true secondary sex characteristics.
Progesterone helps to establish and regulate the uterine
cycle. It causes changes to occur in the cer-vical mucus. Mostly in pregnancy
but in other times as well, progesterone inhibits uterine motility and assists
estrogen in preparing the breasts for lactation. The term progesterone actually means “for gestation.” In the majority of
pregnancies, it is the placenta and not the ovaries that supplies most
progesterone.
Female
Sexual Response
The erectile tissues of the clitoris and vaginal entrance
respond to sexual stimulation. Parasympa-thetic nerve impulses release nitric
oxide to dilate the erectile tissues, increase blood inflow, and swell the
tissues. The nipples become erect and the vagina expands and elongates. If
sexual stimulation is sufficiently intense, parasympathetic impulses cause the
vestibular glands to secrete mucus into the ves-tibule, moistening and
lubricating the surrounding tissues and lower vagina. This facilitates
insertion of the penis.
Just as in males, touch and psychological stim-ulation
increase sexual excitement along autonomic nerve pathways. The clitoris
responds to local stim-ulation, culminating in an orgasm if stimulation is
sufficient. Females do not ejaculate, but do experi-ence increased muscle
tension, raised blood pres-sure and pulse rate, and uterine contractions. Just
before orgasm, the outer one -third of the vagina is engorged with blood. This
increases friction on the penis, with orgasm initiating reflexes directed by
the sacral and lumbar spinal cord. The muscles of the perineum and walls of
both the uterus and uterine tubes contract rhythmically. This helps transport
sperm through the female reproductive tract toward the upper uterine tubes.
Females experience intense pleasure that is fol-lowed by
relaxation, which is the same for males, but do not have a refractory period
after orgasm. Therefore, females can experience multiple orgasms during one
sexual experience. However, orgasm is not required for conception. It is now
understood that female libido is not primarily influenced by the male sex
hormone testosterone. It is instead influenced by dehydroepiandrosterone, which
is an androgen produced by the adrenal cortex.
1. Which
hormones generate reproductive function in females?
2. Explain
why girls experience growth spurts that are more dramatic but shorter in
overall duration than boys.
3. Describe
the female sexual response and identify differences between it and the male
sexual response.