Prophylactic Use of Antimicrobials
| Home | | Pharmacology |Chapter: Essential pharmacology : Antimicrobial Drugs: General Considerations
This refers to the use of AMAs for preventing the setting in of an infection or suppressing contacted infection before it becomes clinically manifest. AMAs are frequently given prophylactically, but in a number of circumstances this is at best wasteful if not harmful.
PROPHYLACTIC USE OF ANTIMICROBIALS
This refers to the use of AMAs for preventing the setting in of an
infection or suppressing contacted infection before it becomes clinically
manifest. AMAs are frequently given prophylactically, but in a number of
circumstances this is at best wasteful if not harmful. The difference between
treating and preventing infections is that treatment is directed against a specific
organism infecting an individual patient, while prophylaxis is often against
all organisms capable of causing infection. The valid as well as improper
prophylactic uses may be categorized as:
1. Prophylaxis Against Specific Organisms
In general highly satisfactory;
the choice of drug is clearcut.
(a) Rheumatic fever:
group A Streptococci: long acting
penicillin G is the drug of choice for preventing recurrences.
(b) Tuberculosis:
Children, HIV positive and other susceptible contacts of open cases: Isoniazid alone
or with rifampin is recommended.
(c) Mycobacterium avium
complex (MAC): HIV/ AIDS patients with low CD4 count may be protected
against MAC infection by azithromycin/ clarithromycin.
(d) HIV infection:
Health care workers exposed to blood by needle stick injury: zidovudine +
lamivudine ± indinavir. Offspring of HIV positive woman can be protected by
zidovudine given to pregnant mother and then to the newborn for 6 weeks.
(e) Meningococcal meningitis: during an epidemic, especially in
contacts; rifampin/ sulfadiazine/ceftriaxone may be used.
(f) Gonorrhoea/syphilis:
before or immediately after contact: ampicillin/ceftriaxone.
(g) Recurrent genital herpes simplex: Acyclovir prophylaxis may
be given when four or more recurrences occur in a year.
(h)Malaria: for
travellers to endemic areas with high transmission rate:
chloroquine/mefloquine.
(i) Influenza A2
: during an epidemic, especially in contacts: amantadine.
(j) Cholera: tetracycline prophylaxis may be given to close
contacts of a case.
(k) Whooping cough:
non-immunized child contact
during the incubation period: erythromycin can abort clinical disease.
(l) Plague: contacts curing an epidemic: doxycycline.
(m)Pneumocystis jiroveci pneumonia: Transplant recipients on immunosuppressants/leukaemia/ AIDS patients may be
protected by cotrimoxazole.
2. Prevention
Of Infection In High Risk Situations
It may be valid and
satisfactory in certain situations, but
controversial in others.
(a)Dental extraction,
tonsillectomy, endoscopies cause damage to mucosa harbouring bacteria → bacteremia occurs. In
patients with valvular defects, this can cause endocarditis: appropriate
prophylaxis with amoxicillin or clindamycin may be given few hours before to
few hours after the manipulation.
(b)Catheterization or
instrumentation of urinary tract: cotrimoxazole or norfloxacin. Patients with
valvular lesions may be protected with ampicillin, gentamicin or vancomycin
during catheterization.
(c)To prevent
recurrences of urinary tract infection in patients with abnormalities of the
tract: cotrimoxazole or nitrofurantoin may be given on a long-term basis since
the organism mostly is E. coli.
(d)Chronic
obstructive lung disease, chronic bronchitis: ampicillin/doxycycline/ciprofloxacin
has been used to prevent acute exacerbations: but are of doubtful value.
(e)Immunocompromized
patients (receiving corticosteroids or antineoplastic chemotherapy, neutropenic
patients): penicillin/cephalosporin ± an aminoglycoside or fluoroquinolone are
often used to prevent respiratory tract infections and septicaemia, but
incidence of superinfections is high.
Prophylaxis Of Surgical Site Infection
Surgical site
infection (SSI) includes superficial incisional infections (e.g. stitch
abscess), deep incisional infection (of soft tissue) and organ/ space infection.
The purpose of surgical prophylaxis is to reduce the incidence of SSI with
minimal alteration of normal microbial flora of the host and minimal adverse
effects.
For grading the need
and intensity of antimicrobial prophylaxis, the operative wounds have been
classified into 4 categories with increasing risk of SSI (see box).
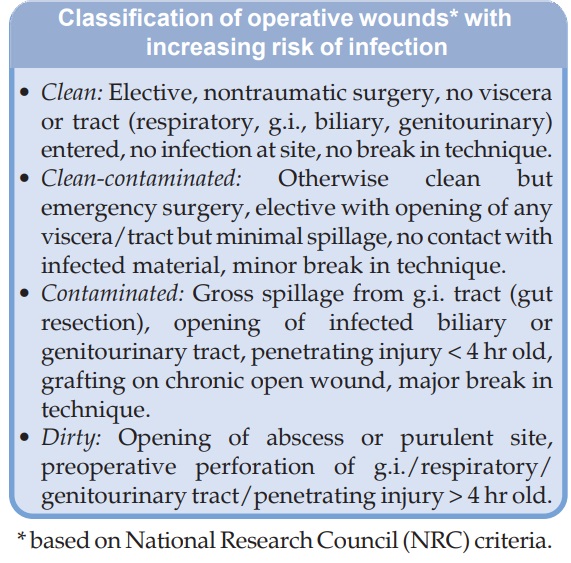
Wound infection occurs
due to microbial contamination of the surgical site. It is important for the
surgeon to see that the wound left after surgery does not get infected. Use of
sterile instruments, cross-infection control measures (antiseptic/disinfectant,
etc.) and good surgical technique to minimise tissue damage, haematoma and
devascularization are the primary, and often the only, measures needed.
However, extensive, prolonged and often combined use of AMAs is made for
prophylaxis of infection after practically all surgeries. Such misuse is
particularly rampent in developing countries, probably because of unreliability
of infection control measures. The SSI is directly related to the number of
bacteria present in the surgical wound at the time of closure. Systemic antimicrobial
prophylaxis should be employed only when there is clear risk of SSI. In
general, it is not required for clean surgery, except in patient at special
risk. Clean surgery in otherwise healthy subjects is associated with very low
risk of SSI.
Incidence of
postoperative infection is higher when surgery had lasted 2 hours or more.
Prophylaxis should be given for surgeries in which a prosthesis is inserted
into the bone or soft tissue. Even clean surgery needs to be covered by AMA in
diabetics, corticosteroid recipients and other immunocompromised subjects,
infants, elderly, malnourished and when there is extensive tissue handling/use
of electrocautery, etc.
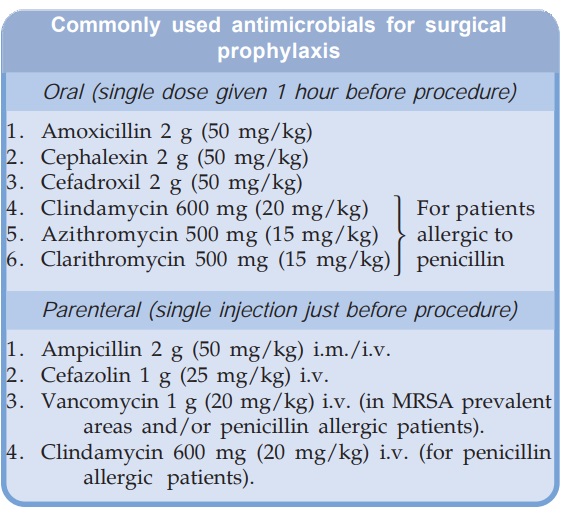
The selection of drug,
dose, timing and duration of prophylactic medication is crucial. It is important
that the antibiotic is not started prematurely and is not continued beyond the
time when bacteria have access to the surgical wound. Administration of the AMA
has to be so timed that peak blood levels occur when clot is forming in the
surgical wound, and it is present throughout the procedure. Thus, most of the
oral drugs are given 1 hour before incision, while i.v. administration just
before/after anaesthesia best ensures effective blood levels of the AMA during
surgery. Most AMAs do not penetrate the clot once it is formed and is older
than 3 hours. Thus, late and prolonged presence of the antibiotic in circulation
serves no purpose, but can foster resistant organisms. In case of prolonged
surgery, the AMA may be repeated i.v. during the procedure. Postoperative
administration of the AMA, especially after 4 hours of wound closure is
recommended only in case of contaminated and dirty surgery, in which case it
may be given for upto 5 days.
To be maximally
effective, a relatively high dose of the AMA is selected which yields peak
blood level several times higher than MIC for the likely pathogens. The drug or
combination of drugs is selected based on the knowledge of the organism most
commonly causing SSI in a given procedure. Local patterns of wound infection
(e.g. prevalence of MRSA) and sensitivities of the causative organisms should
guide the selection. The commonly employed AMAs for prophylaxis in case of
clean and clean-contaminated surgeries are listed in the box.
Dirty contaminated wounds (including road side accidents): The antimicrobial
regimens generally administered for 5 days in case of contaminated dirty wounds
are:
1. Cefazolin 1 g i.v. 8 hourly +
vancomycin 1 g i.v. 12 hourly
2. Cefoxitin 1 g i.v. 6 hourly/ceftizoxime
1 g i.v. 12 hourly.
3. Clindamycin 0.6 g i.v. 8 hourly +
Gentamicin 80 mg i.v. 8 hourly.
4. Ampicillin 2 g i.v. 6
hourly/vancomycin 1 g i.v. 12 hourly + Gentamicin 80 mg i.v. 8 hourly +
Metronidazole 0.5 g i.v. 8 hourly.
5. Amoxicillin 1 g + Clavulanate 0.2
g i.v. 12 hourly.
* All given for 5 days.
3. Prevention Of Infection In General
This is highly unsatisfactory in most cases and must
be condemned. Examples are:
·
Neonates, especially after prolonged or instrumental
delivery.
·
To prevent postpartum infections in the mother
after normal delivery.
·
Viral upper respiratory tract infections: to
prevent secondary bacterial invasion.
·
To prevent respiratory infections in unconscious
patients or in those on respirators.
Antimicrobial
prophylaxis in these situations may be hazardous—infection by resistant
organisms, fungal and other superinfections can occur, because it is not
possible to prevent all infections, at all times, in all individuals.
Related Topics
