Skin
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Support and Movement: Integumentary System
1. List and discuss the five layers of the epidermis. 2. Explain melanin, melanocytes, and melanosomes. 3.Which layer of the epidermis is vascular? 4. What are the functions of the subcutaneous layer
Skin
The skin is also known as the integument. This is
where the name integumentary system
is derived. The skin varies in thickness between 1.5 and 4 mm, depending on
which part of the body it covers. The general functions of the skin are:
■■ Protection of the underlying organs and tissues against abrasion, chemicals, fluid loss, and impact
■■ Detection of stimuli (pain, pressure, temperature, and touch) and relay of this information to the nervous system
■■ Maintenance of normal body temperature, as needed, via insulation or
evaporative cooling
■■ Melanin production, to protect underlying tissue from ultraviolet (UV)
radiation.
■■ Keratin production, to serve as a water repellant and to protect
against abrasion
■■ Vitamin D3 synthesis; this steroid is converted to calcitriol, a hormone vital for normal calcium metabolism
■■ Lipid storage, in the adipocytes of the dermis and in the adipose
tissue of the subcutaneous layer
■■ Excretion of organic wastes, salts, and water via the integumentary glands
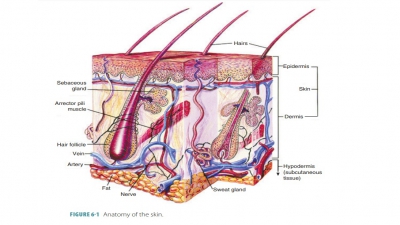
The two main layers of skin are
the epidermis and dermis. The epidermis, the outer layer, is made up of keratinized stratified squamous
epithelium (FIGURE 6-1). It is also called the superficial
epithe-lium. It has four primary cell types and four or five layers, depending on body location
(four layers in most body areas and five layers on the palms, fin-gertips, and
soles of the feet). Unlike the dermis, the epidermis is not vascularized.
Nutrients must dif-fuse through dermal blood vessels and tissue fluid to reach
the epidermis. The dermis, the inner layer, is much thicker than the epidermis and consists of
papillary and reticular regions. The papillary region contains fine elastic
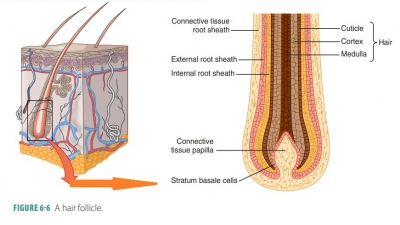
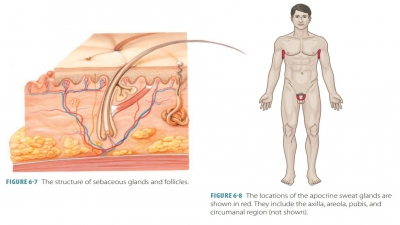
fibers and dermal papillae. The reticular region is composed of connective
tissue containing collagen, elastic fibers, fat tissue, hair fol-licles,
nerves, sebaceous (oil) glands, and the ducts of sweat glands. The epidermis is
connected to the dermis by a basement membrane.
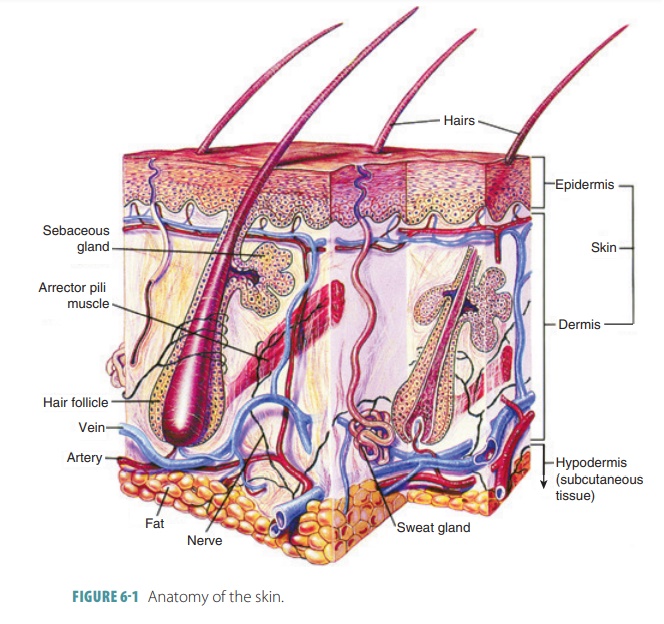
Loose connective tissue below the dermis binds the skin to the organs underneath. This tissue, which is pre-dominantly adipose (fatty), forms the subcutaneous layer, also known as the hypodermis or superficial fascia. It is deep below the dermis and not actually part of the skin. This adipose tissue insulates the body, conserving inner heat and helping to keep excessive heat from out-side the body from entering. The major blood vessels that supply the skin and adipose tissue are containe within the subcutaneous layer. The hypodermis is loose enough that the skin slides with ease over its underlying structures. It also acts as a shock absorber and becomes much thicker when weight is gained. This tissue first accumulates in the anterior abdomen in males and in the thighs and breasts in females. The hypodermis lends its name to the term “hypodermic,” which is where sub-cutaneous injections are made via hypodermic needles.
Epidermis
The epidermis is the outermost
layer of the skin and is composed of stratified squamous epithelium. The
epidermis does not contain blood vessels, although its deepest layer, the
stratum basale, receives blood via the dermal blood vessels. Epidermal cells
require diffusion of oxygen and nutrients from the capillaries within the
dermis. Cells that have a higher metabolic demand are located closer to the
basement mem-brane. Cells in this layer of the epidermis divide and grow,
moving toward the skin surface and away from the dermis below. As they move
upward, they receive fewer nutrients and eventually die. Older cells are called
keratinocytes, which harden with age in the process known as keratinization. Keratin protein fills the cytoplasm of these skin
cells, which collectively form a layer called the stratum corneum. Dead skin cells in this layer are eventually shed
from the body.
Epidermis Layers
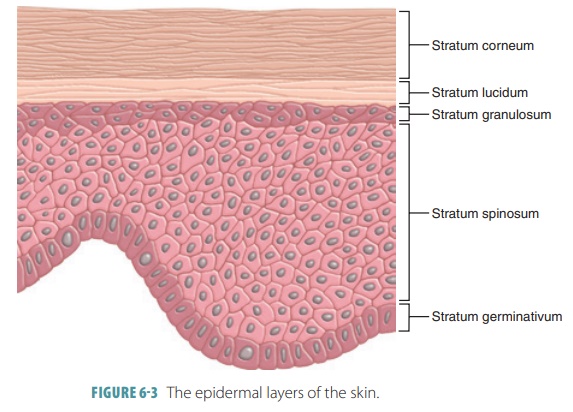
There are basically five layers
of the epidermis: stratum germinativum (stratum basale), stratum spi-nosum,
stratum granulosum, stratum lucidum, and stratum corneum. Most of the body
surface is covered by thin skin,
consisting of four layers of keratinocytes that total only 0.08 mm in
thickness. Areas of thick skin (the
palms and soles) contain a fifth layer, the stratum lucidum, and the stratum
corneum in these areas is much thicker. Therefore, on the palms and soles, the
epidermal layers total about 0.5 mm in thickness. The five individual layers
are explained as:
■■ The stratum
germinativum (“germinative” or “basal layer”)
is the innermost epidermal layer and is also known as the stratum basale (basal
layer). It is interlocked with the underlying dermis via hemidesmosomes, which are tiny pin-like structures. This layer
forms the epidermal ridges, extending into the dermis, which are adjacent to
dermal projections (dermal papillae). The attach-ment of the stratum basale to
the dermis is along a wavy borderline. Epidermal ridges are import-ant because
the strength of the attachment of the layer is proportional to the surface area
of the basal lamina. Ridge shapes are genetically deter-mined, and the pattern
of epidermal ridges does not change during the life span of an individual (FIGURE 6- 2).

The ridge patterns on
the tip of each finger are instrumental in the forming of finger-prints. Each
person’s fingerprints are unique, including those of identical twins. As a
result, fingerprints are commonly used in criminal cases to identify individuals.
Large basal (germinative) cells dominate the stratum germinativum. Stem cells
are usually in single rows, with divisions that replace superficial
keratinocytes that are lost or shed on the epithelial surface. When a stem cell
divides into daughter cells, they are pushed from the stratum germinativum
upward into the next layer, the stratum spinosum. There are many mitotic cell
nuclei in this layer, reflecting rapid cell division. Approximately, 10% to 25%
of these cells are melanocytes that reach into the stratum spinosum. The ridges
on the palms and soles also increase the surface area of the skin and help us
to grip objects due to the increased friction. In areas where the skin surface
does not have hair, there are specialized epithelial cells known as Merkel or
tactile cells. They are sensitive to touch, releasing chemicals that stimulate
sensory nerve endings when they are compressed. The brownish color of the skin
comes from melanocytes, distributed in the stratum germinativum. They have cell
processes that extend into the more superficial layers.
■■ The stratum spinosum (“spinous” or “prickle cell layer”) is
made up of 8–10 layers of keratinocytes that are bound together by desmosomes.
It contains cells that look like tiny pin cushions, because of exposure to
chemicals that caused the keratinocyte cytoplasm to shrink slightly. However,
the desmosomes and elements of the cytoskeleton remained intact. Some entering
cells from the stratum basale continue dividing, which increases the thickness
of the epithelium. Additionally, this layer contains Langerhans cells, also
known as dendritic cells, which stimulate immune defenses against
microorganisms and superficial skin cancers.
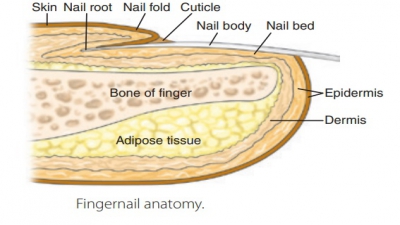
■■ The stratum granulosum (“granular layer”) is the third layer
and consists of only three to six layers of keratinocytes. Cells in this layer
have mostly stopped dividing and begin to make the proteins keratin and
keratohyalin. Keratin is tough and fibrous, making up hairs and nails.
Developing keratin fibers become flatter and thinner, as their membranes
thicken and lose permeability. Keratohyalin forms cytoplasmic granules that
dehydrate cells and aggregate and cross-link keratin fibers. The cells die as
the nuclei and other organelles disintegrate. Continued dehydration causes this
layer to become extremely interlocked. Nutrients are brought via capillaries in
the dermis. However, above this layer, the cells are too distant from the
dermal capillaries and glycol lipids coating them keep nutrients from being
supplied, hence their normal death.The stratum lucidum (“clear layer”) is the
fourth region, which is only found on the palms of the hands and soles of the
feet, with a glassy or clear appearance. Therefore, the overall skin of the
palms and soles is thicker than on other parts of the body. In this layer, the
cells are flattened and densely packed, have few organelles, and are filled
with keratin. The stratum lucidum is microscopically viewed only in thick skin,
appearing as a thin translucent band above the stratum granulosum. It consists
only of two or three rows of flat and dead keratinocytes that have indistinct
boundaries.
■■ The stratum
corneum (“horny layer”) makes up the surface of the skin and contains 15–30
layers of keratinized cells that are protective and filled with keratin, they
are the most numerous epidermal cells. The process of keratinization is also
known as cornification. It occurs on all exposed body surfaces, except the
anterior eye surfaces.The dead cells of the stratum corneum are tightly
interconnected by desmosomes. Because of this interconnection, keratinized
cells of this layer are shed in large sheets rather than individually. Cells
move from the stratum germinativum to the stratum corneum in 7–30 days,
remaining in the stratum corneum for about two weeks before being washed away
or naturally shed. The dryness of the stratum corneum reduces the amount of
potential microbial growth, and this layer is coated with lipid secretions from
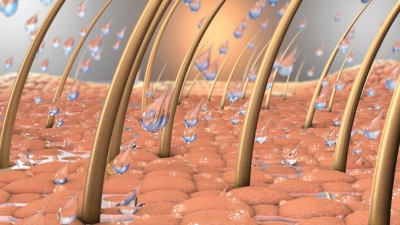
the sebaceous glands.This layer is water resistant but not waterproof. Water
from the interstitial fluids eventually penetrates to the surface. About 500 mL
of water is lost from this layer via evaporation every day in a process known
as insensible perspiration. This differs from sensible perspiration, which is
produced by merocrine sweat glands. The rate of insensible perspiration may be
increased when the epidermis is damaged and sometimes can be dangerous, such as
when severe burns excessively damage the epidermis. Oppositely, being immersed
in fresh (hypotonic) water for a long time causes the epidermal cells to swell
up to four times their normal volume. This is most noticeable on the palms and
soles. Immersion in ocean (hypertonic) watercauses water to leave the epidermal
cells, eventually resulting in dehydration. FIGURE 6-3 shows how healthy skin
balances the production of epidermal cells with the loss of dead cells. The
stratum corneum makes up nearly three-fourths of the total epidermal thickness.
Keratin protects it against abrasion and glycolipids cause its water
resistance. Approximately, 50,000 dead cells are shed from this layer every
minute. In an average lifetime, you will lose 40 pounds of these dead skin
cells.
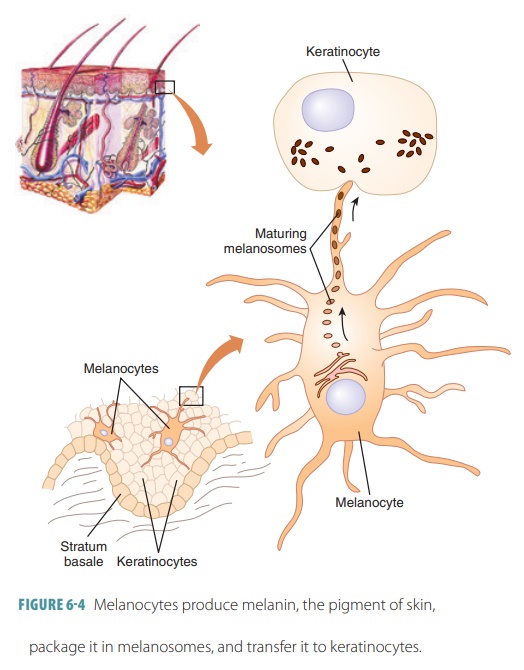
Epidermal Cells
The epidermis protects the
underlying tissues against the effects of harmful chemicals, excess water loss,
mechanical injury, and pathogenic microorganisms. Layers of pigment in the
epidermis help protect both epidermal and dermal tissues. Melanin is a
brown, yellow-brown, or black pigment produced by spider-shaped melanocytes located
in the stratum germinativum, either between or deeply rooted in the epithelial
cells (FIGURE 6-4). It is made of tyrosine amino acids and has two forms that range in
color (from red-yellow to brown-black). Synthesis of mela-nin is based on an
enzyme called tyrosinase. Melanin accumulates in granules that are bound to membranes called melanosomes. Lysosomes eventually break
down melanosomes, meaning that melanin pigment is found only in the deeper layers of the
epidermis, regardless of race, all human beings have about the same number of
melanocytes. Motor proteins move down actin filaments to reach the ends of each
mela-nocyte’s processes. Then, they move to nearby kerat-inocytes, accumulating
on the superficial side of the keratinocyte nucleus. Normal exposure of the
skin to sunlight causes the keratinocytes to secrete chemi-cals that stimulate
the melanocytes. Melanin absorbs UV
radiation from sunlight, protecting the epidermis and dermis from its harmful effects. It builds up from sun
exposure, absorbing rays, dissipating this energy as heat, and protecting DNA
of viable skin cells from UV radiation. However, sunlight contains extremely
significant amounts of UV radiation. Although small amounts of UV radiation are
beneficial because they stimulate the epidermal production of a compound
required for calcium ion homeostasis (the produc-tion of vitamin D), larger
amounts damage DNA. This causes mutations, promoting the development of cancer.
UV radiation can also produce burns. When severe, they can damage the epidermis
and the dermis.
Keratinocytes produce keratin, which is the fibrous
protein that aids the epidermis in protecting the body. Most epidermal
cells are keratinocytes, which arise in the stratum basale. Upon reaching the
skin surface, they are already dead. At this time, they have a scale-like
appearance and are basically plasma membranes filled with keratin. Every day, millions
of dead kera-tinocytes rub off. Therefore, the epidermis is totally replaced
every 25–45 days.
Star-shaped dendritic cells or Langerhans cells from the bone marrow
eventually move to the epider-mis. They consume foreign substances and play a
key role in activating the immune system. Tactile
cells or Merkel cells are located at the epidermal–dermal junction. They
have spiked shapes and combine with disc-like sensory nerve endings to form tactile discs, which are receptors for
the sense of touch.
Differences in skin color are
based on the amount of melanin produced and how it is distributed through-out
the skin. Skin color is based on a person’s genetics, which regulates the
amount of melanin produced by the melanocytes. Other factors that affect skin color
include sunlight, UV light, and X-rays. Dermal blood vessel also affects the
color of the skin. Well-oxygenated blood makes light-skinned people appear
pinker, whereas poorly oxygenated blood makes them appear bluer, as in the
condition known as cyanosis. Diet
also affects skin color, as do biochemical imbalances. For example, the buildup
of the substance known as bili-rubin makes
the skin appear yellowish, as in the con-dition called jaundice.
Also contributing to skin color
are the pigments carotene and hemoglobin. Carotene is a yellow to orange pigment that primarily
accumulates in the stratum corneum and the hypodermic fatty tissue. It is also
found in plant products such as carrots and other orange-colored vegetables.
The color of carotene is most easily seen in the palms and soles, especially in
lighter skinned individuals, where the stratum cor-neum is present in thicker
cellular levels. It intensi-fies in the body when large amounts of foods rich
in carotene are consumed. Carotene can be converted to vitamin A (essential for
normal vision), which aids in the health of the epidermis. Carotene, along with
variations in melanin, contributes to the skin color of people from certain
Asian countries. Hemoglobin is the
red pigment inside red blood cells. As it circulates throughout the dermal
capillaries, it gives off a pink color that is easily seen in people with
fairer skin.
1. List and discuss the five layers of the epidermis.
2. Explain melanin, melanocytes, and melanosomes.
3.Which layer of the epidermis is vascular?
4. What are the functions of the subcutaneous layer