The Netherlands
| Home | | Pharmacovigilance |Chapter: Pharmacovigilance: Other Databases in Europe for the Analytic Evaluation of Drug Effects
The Dutch system of health care is based on GPs who practice in the community but not in the hospital, refer-ring ambulatory patients to specialists for outpatient or inpatient care.
THE NETHERLANDS
GENERAL PRACTICE SYSTEM
The
Dutch system of health care is based on GPs who practice in the community but
not in the hospital, refer-ring ambulatory patients to specialists for
outpatient or inpatient care. Specialists report their findings to the GP, who
acts as a gatekeeper. Approximately 90% of the patients’ presenting problems
are addressed by the GP (van der Lei et
al., 1993; Leufkens and Urquhart, 2005) time staff physicians who are
specialists of various kinds provide hospital care. Medical care, including
prescription drugs, is paid for by various insurers, which provide a basic
service to all citizens. Patients can only be registered with one GP but are
free to change, which happens infrequently and nearly always because the
patient moves out of the area. When a patient trans-fers, so does the record.
More than 75% of the patients will visit their GP at least once per year (van
derLei et al., 1993). The high degree
of computerization of GPs has given rise to the birth of several GP networks;
most of them are connected to one of the seven University Centres. One of the
largest research-oriented GP databases is the IPCI database, which has been
created with the specific purpose to conduct phar-macoepidemiological studies
(van der Lei et al., 1993; Vlug et al., 1999).
INTEGRATED PRIMARY CARE INFORMATION
In
1992, the IPCI Project was started by the Depart-ment of Medical Informatics of
the Erasmus Univer-sity Medical School, initially in collaboration with
Intercontinental Medical Statistics (IMS). In 1998, IMS stepped out, and since
then the database was run independently by the department of Medical
Informat-ics in collaboration with the Pharmacoepidemiology Unit. Integrated
Primary Care Information is a longi-tudinal observational database that
contains data from computer-based patient records of a selected group of GPs
throughout the Netherlands that voluntarily chose to supply data to the
database (Vlug et al., 1999). General
practitioners only receive a minimal reim-bursement for their data and control
usage of their data, through the Steering Committee and through the possibility
to withdraw data for specific studies. The collaborating GPs are comparable to
other Dutch GPs regarding age and gender.
As
of January 2005, there are 120 practices belong-ing to more than 150 GPs that
have provided data to the database. The first practice was recruited into the
IPCI project in 1994. Practices have therefore been supply-ing data for varying
periods. The database contains information on more than 700 000 patients. This
is the cumulative amount of patients who have ever been part of the dynamic
cohort of registered patients. Turnover occurs as patients move and transfer to
new practices. The records of ‘transferred out’ patients remain on the database
and are available for retrospective study with the appropriate time. As of
December 2005, there were 400 000 active patients registered with the
collaborat-ing GPs, 49% was male and 57% was insured through the Sickfund, and
the mean age was 38 years. In 2006, the IPCI database is expected to grow to
cover a popu-lation of 1 million active subjects. This is achieved by extending
data retrieval to GPs with other GP informa-tion systems than the original
ELIAS system alone. Data are downloaded on a monthly basis, and the information
is sent to the gatekeeper who anonimizes all information before further access
is provided.
The
database contains anonymous patient iden-tifiers, demographics and eligibility
dates (date of birth, sex, patient identification, insurance, date of
registration and transferring out and date of death), notes (subjective and
assessment text), symptoms, signs, prescriptions, and indications for therapy,
phys-ical findings, referrals, hospitalizations and labora-tory values. All
data are directly entered into a computer during the consultation hour where it
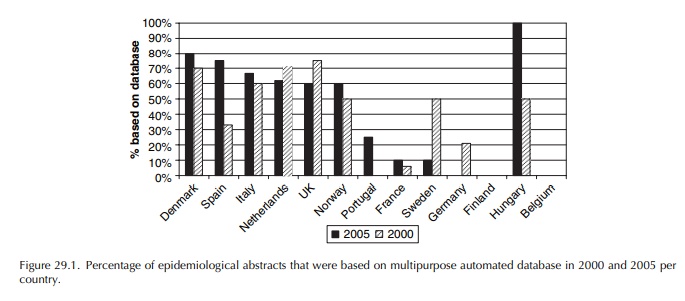
is stored (see Figure 29.1 for database structure). The International
Classification of Primary Care (ICPC) is the coding system for patient
complaints and diag-noses, but diagnoses and complaints can also be entered as
free text that is available as raw data (Lamberts and Wood, 1987). Prescription
data such as product name, quantity dispensed, dosage regi-mens, strength and
indication are entered into the computer to produce printed prescriptions (Vlug
et al., 1999). The National Database
of drugs, maintained by the Z-index, enables the coding of prescriptions,
according to the Anatomical Therapeutic Chemical (ATC) classification scheme
recommended by the WHO (de Smet, 1988).
Access to original medical records (discharge letters of hospitals) and administration of questionnaires to GPs is possible through the gatekeeper but only after approval of the IPCI Steering Committee. Data accu-mulated in the IPCI database have proven to be of high quality and suitable for epidemiological and pharma-coepidemiological research (Vlug et al., 1999). Data can be used for research purposes, but because of the privacy issues related to the presence of clinical notes access is possible only at the Erasmus Univer-sity Medical Centre and after approval of the Steering Committee.
The
database has been used for studies on disease occurrence (Eland et al., 2001, 2002; Verhamme et al., 2002; Straus et al., 2004a; van Soest et
al., 2005) and drug utilization
such as the change in prescriptions of terbinafine following a highly debated
press campaign (‘t Jong et al., 2004)
or appropri-ate prescribing in the elderly (van der Hooft et al., 2005); adherence and persistence with treatment ranging
from gastroprotection (Sturkenboom et al.,
2003a,b), antihypertensives, lipid lowering drugs, antidepressants and
respiratory drugs and the asso-ciation between adherence and treatment
outcomes; effectiveness of drugs and vaccinations (Voordouw et al., 2003, 2004; Dieleman et al., 2005); and last but not the least, a variety of adverse
drug reac-tions (Visser et al., 1996;
van der Linden et al., 1998, 1999; Straus
et al., 2004b, 2005). For a complete
updated list of publications, we refer to the website (www.ipci.nl).
Special
features of the database comprise the possi-bility to conduct randomized
database studies with naturalistic follow-up (Mosis, 2005a,b), pharmacoge-netic
studies and the possibility to return to patients and ask for additional
information, such as reasons for non-compliance, quality of life and blood
samples.
Related Topics
