The Respiratory Muscles
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Respiratory System
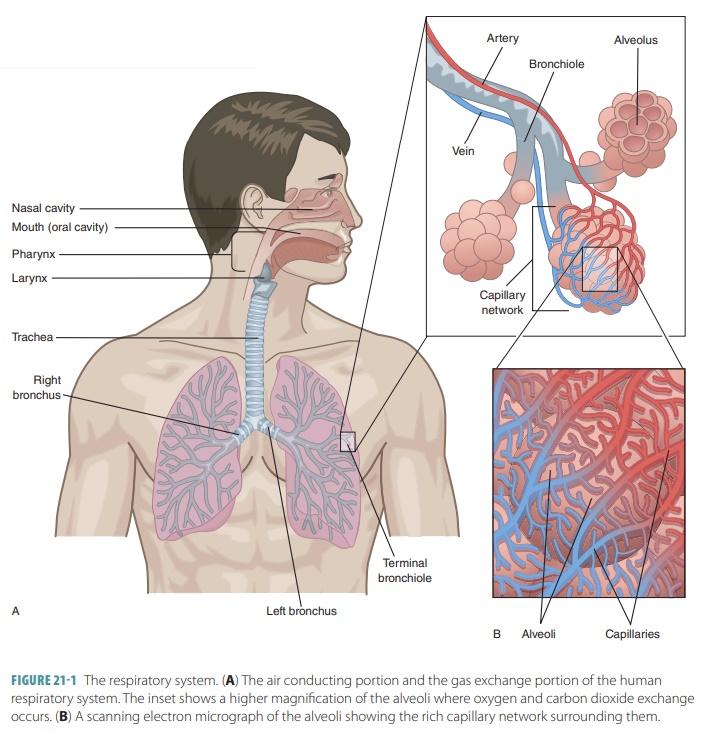
As the diaphragm contracts, the external or inspiratory intercostal muscles between the ribs are stimulated to contract.
Organization of the Respiratory System
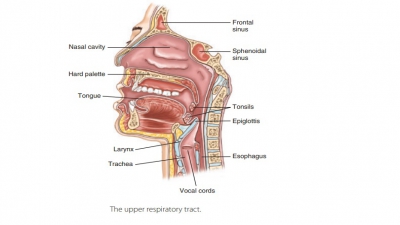
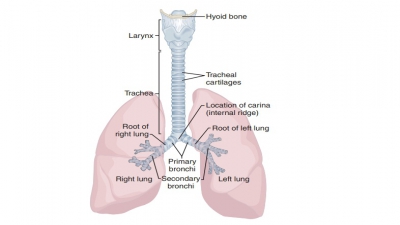
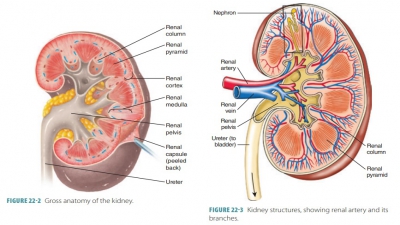
The upper respiratory tract includes the nose, nasal cavity, paranasal sinuses, and pharynx. The lowerrespiratory tract includes the larynx, trachea, and lungs. The lungs contain the bronchi, bronchioles, and alveoli. FIGURE 21-1 shows the structures of the respiratory system.
The
Respiratory Muscles
As the diaphragm contracts, the external or inspiratory intercostal muscles between
the ribs are stimulated to contract. The ribs raise and the sternum elevates,
enlarging the thoracic cavity further. The lungs expand in response to these
movements as well as those of the pleural membranes. When the external
intercostal muscles move the thoracic wall upward and outward, the parietal
pleura also moves as does the visceral pleura. The lungs then expand in all
directions.
Expiration occurs because of the elastic recoil of tissues
and surface tension. As the diaphragm low-ers, it compresses the abdominal
organs below it. The elastic tissues cause the lungs and thoracic cage to
return to their original shapes, and the abdominal organs move back into their
previous shapes to push the diaphragm upward. Surface tension decreases the
diameters of the alveoli, increasing alveolar air pressure. Air inside the
lungs is forced out, meaning that normal resting expiration is a passive
process. If more forceful exhalation is required, the posterior internal or expiratory intercostal muscles
contract. This pulls the ribs and sternum downward and inward to increase the
pressure in the lungs. The abdominal wall muscles squeeze the abdominal organs
inward, forcing the diaphragm even higher against the lungs. Accessory respiratory muscles are
activated when there is a need for
greatly increased respiratory depth and frequency. The accessory respiratory
muscles include the internal intercostal,
sternocleidomastoid, serratus anterior,
pectoralis minor, scalene, transverse thoracis and abdominis, external and
internal oblique, and rec-tus
abdominis muscles. The processes of expiration and inspiration are shown in FIGURE 21-8A and B.
Muscles Used in Inhalation
The active process of inhalation involves one or more of
these three actions:
■■ Diaphragm
contraction: This flattens the thoracic cavity floor to increase its
volume; air is drawn into the lungs. About 75% of air movement in normal
at-rest breathing results from this contraction.
■■ External intercostal muscle contraction: This raises the ribs, contributing about 25% of air volume in the lungs at rest.
■■ Accessory
muscle contraction: This assists the exter-nal intercostal muscles in
elevation of the ribs; the speed and mount of rib movement is increased.
Muscles Used in Expiration
Based on the level of respiratory activity, expiration
(exhalation) is classified as passive
or active. When it is active, one or
both of the following actions occurs:
■■The ribs are depressed by the
internal intercostal and transversus thoracic muscles. This means that the
width and depth of the thoracic cavity is reduced.
■■ The abdominal muscles help the
internal intercostal muscles by compressing the abdomen, which forces the
diaphragm upward. The abdominal muscles include the external oblique, internal
oblique, transversus abdominis, and rectus abdominis.
Modes of Breathing
The volume of air required to be move in or out of the
respiratory system influences different combinations of respiratory muscle
actions. Respiratory movements are usually classified as either quiet breathing or forced breathing. These
classifications are made based on pat-terns of muscle activity within a single
respiratory cycle.
Quiet Breathing
Quiet breathing is also known as eupnea. In this type of breathing, muscular contractions are
required for inhalation, while exhalation is done passively. Inha-lation
usually includes contraction of the diaphragm and external internal intercostal
muscles. There are variations in the actions of these muscles:
■■ Deep
(diaphragmatic) breathing: Diaphragm contrac tion provides the required
thoracic volume change,with air drawn into the lungs as the diaphragm
contracts. When it relaxes, air is passively exhaled.
■■ Shallow
(costal) breathing: The rib cages changes shape, altering thoracic volume.
Contractions of the external intercostal muscles raise the ribs, enlarge the
thoracic cavity, and allow inhalation to occur. When these muscles relax,
passive exhalation occurs.
The elastic lung fibers are stretched when the lungs expand
during quiet breathing. Rib cage elevation stretches opposing skeletal muscles
as well as elastic fibers in the body walls’ connective tissues. When mus-cles
of inhalation relax, there is recoiling of the elastic fibers. The diaphragm,
rib cage, or both return to their original positions. This is known aselastic rebound.
Diaphragmatic breathing is used during minimal activity
levels. When more air volume is required, the inspiratory movements increase,
along with the actions of rib movement. Costal breathing, even while resting,
is able to be the dominant form when movements of the diaphragm are restricted,
such as by fluids, masses, or abdominal pressure. A good example is during
pregnancy, when a woman uses costal breathing on an increased basis as the
enlargement of her uterus forces the abdominal organs against the diaphragm.
Forced Breathing
Forced breathing is also called hyperpnea. It involves active movements of inspiration and
expiration. The accessory muscles assist with inhalation. The inter-nal
intercostal muscles contract during exhalation. When hyperpnea is at maximum
level, the abdominal muscles assist in exhalation. When they contract, the
contents of the abdomen are compressed and pushed up against the diaphragm.
This reduces the thoracic cavity volume even further.
Pressure Relationships in the Thoracic Cavity
The force that moves air into the lungs is atmo-spheric
pressure, and respiratory pressures are always expressed in relation to this
pressure. Atmospheric pressure is defined as the pressure exerted by the gases,
which comprise the air that surrounds
us. At sea level, normal air pressure is equal to 760 mm Hg. It is exerted on
every surface in contact with the air. The pressure on the inside of the lungs
and alveoli is almost equal to outside air pressure. Atmospheric pressure may
also be expressed in atmospheric units, which means that 760 mm Hg equals 1
atmospheric unit.
A region of the world is lower than atmospheric pressure when there is a negative respiratory pres-sure.
For example, a respiratory pressure of –2 mm Hg means the pressure is lower
than atmospheric pres-sure by 2 mm Hg. So, 760 mm Hg minus 2 mm Hg leaves 758
mm Hg, which is described as the absolute
pressure of
the given region. A zero respiratory pressure is equal to atmospheric pressure. A positive
respiratory pressure is higher than atmospheric pressure.
Intrapulmonary
pressure is also known asintra-alveolar
pressure, abbreviated as “Ppul,” and defined as the pressure inside the alveoli. Ppul
increases and decreases during normal breathing but always becomes equalized
with atmospheric pressure eventually. The pressure inside the pleural cavity is
known as intrapleu-ral pressure,
abbreviated as “Pip,” and also increases and decreases during normal breathing. However, Pip is
always approximately 4 mm Hg lower than Ppul. It is, therefore,
described as always negative to the Ppul.
This occurs because there are opposing forces in the thorax.
Two forces pull the visceral pleura of the lungs away from the parietal pleura
of the wall of the thorax, causing the lungs to collapse—the natural tendency
of the lungs to recoil and the surface tension of the alveolar fluid. Because
the lungs are highly elastic, they always form the smallest size they possibly
can form. The mol-ecules of the fluid that lines the alveoli are attracted to
each other. This causes surface tension, which continu-ally draws the alveoli
to their smallest possible dimen-sions. The natural elasticity of the chest
wall opposes these lung-collapsing forces. The forces of the chest wall pull
the thorax outward, enlarging the lungs.
To have a negative Pip, the amount of pleural
fluid in the pleural cavity needs to remain as little as pos-sible. On a
continuous basis, pleural fluid is pumped out of the pleural cavity, entering
the lymphatics. Oth-erwise, it would accumulate in the intrapleural space and
produce a positive pressure in the pleural cavity. The negative pressure in the
intrapleural space and the snug joining of the lungs to the wall of the thorax
are extremely critical. If a condition equalizes Pip with either
intrapulmonary or atmospheric pressure, imme-diate lung collapse occurs. The
difference between the intrapulmonary and Pips is called the transpulmonary pressure. This pressure keeps the air spaces in the lungs open, keeping them from collapsing.
Airway Resistance
Friction is the primary nonelastic source of resistance to
gas flow. Also referred to as “drag,” it occurs in the respiratory passageways.
Gas flow is related to pressure and resistance. Equivalent factors determine
gas flow in the respiratory system and blood flow in the cardio-vascular
system. Usually, tiny differences in pressure produce significant changes in
gas flow volume. During normal, quiet breathing, the average pressure gradient
is 2 mm Hg or less. This small amount is able to move 500 mL of air with each
breath in and out of the lungs!
Alveolar Surface Tension
Surface
tension is a state of tension at a liquid’s surface
that is produced by unequal attraction. At the boundary of a gas and a liquid,
the liquid molecules are attracted to each other more strongly than they are
attracted to the gas molecules. Surface tension pulls liquid molecules closer
together. It lessens their contact with the gas molecules because they are not
similar. Surface tension also resists forces that tend to increase the liquid’s
surface area.
H2O is an example of a liquid with very high
surface tension. It is made up of highly polar molecules. H2O makes
up a major percentage of the liquid film coating the walls of the alveoli. As a
result, it helps to reduce the alveoli to their smallest possible size.
However, if this film was only made of H2O, the alveoli would
collapse between every breath taken. Why does it not collapse?
Surfactant
is a mix of lipids and proteins that resembles a detergent in its effects. It is
produced by type II alveolar cells. Surfactant makes H2O molecules
become less cohesive. This reduces the surface ten-sion of the alveolar fluid.
As a result, lower amounts of energy are needed to expand the lungs and keep
the alveoli from collapsing. The type II alveolar cells are stimulated to
secrete more surfactant by breaths that are deeper than normal.
Respiratory Volumes
There are four distinct respiratory volumes that can be measured by using spirometry, which is also known as pulmonary function testing. Spirometry
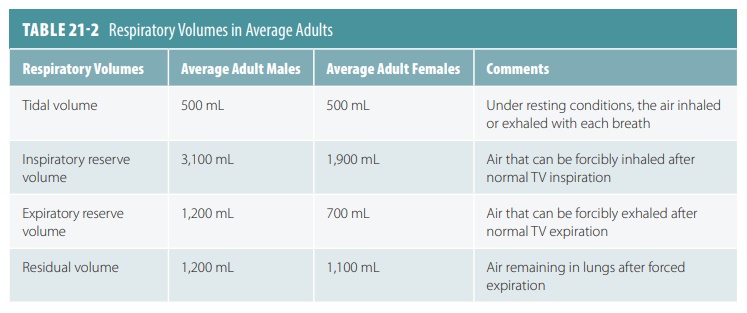
is used to measure the functional capacity of the lungs (FIGURE 21-9). TABLE 21-2 shows average values of respi-ratory volumes for men and
women of normal weight at about 21 years of age. As discussed earlier, about
500 mL of air move in and out of the lungs with each breath during normal,
quiet breathing. This is known astidal volume (TV). However, between 2,100
and 3,200 mL of
air can be inspired forcibly beyond the TV. This is known as
the inspiratory reserve volume (IRV).
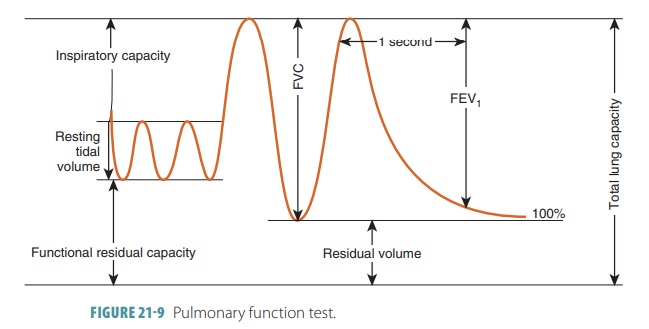
The amount of air that can be expelled from the lungs after
a normal TV expiration is between 1,000 and 1,200 mL. This is known as the expiratory reserve volume (ERV).
However, after the most strenuous
expiration of air, there are still about 1,200 mL remaining in the lungs.
Called the residual
volume,
it helps to prevent lung collapse and keep the alveoli open, which is also referred to as being
patent.
1. During inspiration, explain how Ppul decreases.
2. Explain airway resistance and the factors involved.
3. Describe how surfactant keeps the alveoli from collapsing.
4. What is the role of surfactant in the alveoli?
5. Differentiate respiratory volumes from respiratory capacities.
Respiratory Capacities
Respiratory
capacities as well as respiratory volumes are useful for diagnosing problems with
pulmonary ventilation. On average, adult females have smaller bodies and lung
volumes than do adult males, which is why there are gender-related differences
regarding respiratory volumes and capacities (TABLE 21-3).
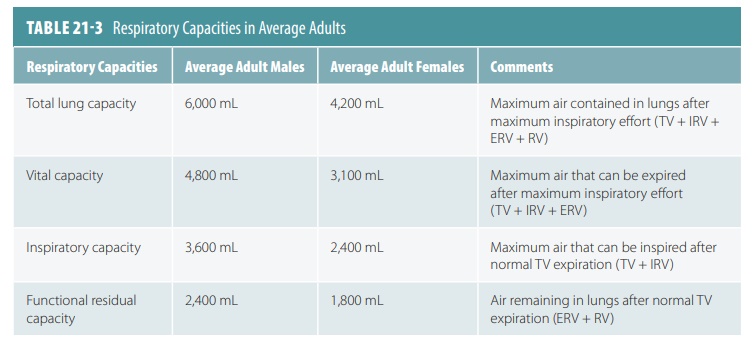
Respiratory capacities include inspiratory, func-tional
residual, vital, and total lung capacities. Two or more lung volumes always
make up the respi-ratory capacities (FIGURE 21-10 ). The inspiratory capacity is the total air that
can be inspired after one normal TV expiration. Therefore, TV plus IRV equals
inspiratory capacity.
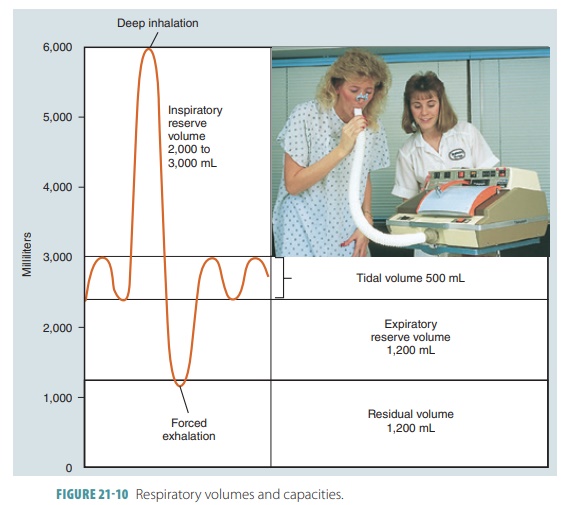
Functional residual capacity (FRC) is the air that remains in the lungs after one normal TV expira-tion. Therefore, residual volume plus ERV equals FRC. Vital capacity (VC) is the total amount of exchange-able air and is made up of the total volume, IRV, and ERV. Total lung capacity (TLC) is the total of all lung volumes added together.
Dead Space
A certain amount of inspired air does not contrib-ute to
alveolar gas exchange but fills the conducting respiratory passageways. Anatomic dead space is made up of the
volume of these conducting conduits. The dead space is approximately 150 mL.
For example, only 350 mL of air are used in alveolar ventilation out of a TV of
500 mL. In conditions of alveolar collapse or mucous obstruction, gas exchange
may stop. Then, the alveolar dead space
is added to the anatomic dead space, comprising a volume that is not used,
known as the total dead space.
Testing Pulmonary Function
Originally, a spirometer was used
to test pulmo-nary function. Today, a small electronic measuring device is used
instead, into which the patient blows air. Electronic spirometry is used for
evaluating lost respiratory function and for studying respiratory dis-ease
progression. Although not diagnostic, it can dis-tinguish between obstructive and restrictive diseases of the pulmonary region. Obstructive pulmonary
diseases such as chronic bronchitis involve increased airway resistance. The
lungs hyperinflate, increasing TLC, FRC, and residual volume. Restrictive
diseases involve a reduction in TLC. Because lung expansion is limited, there
are decreases in VC, TLC, FRC, and residual volume.
The rate at which gas moves in and out of the lungs is
expressed in forced vital capacity
(FVC) and forced expiratory volume (FEV). FVC measures how much gas is expelled
after taking a deep breath and forcefully, maximally, and rapidly exhaling. FEV
determines how much air is expelled during certain time intervals of the FVC
test. FEV1 is the volume
exhaled during the first second. Healthy people can exhale approximately 80% of
their FVC in one second. Obstructive pulmo-nary diseases cause an individual to
be unable to exhale anywhere near this percentage. In restrictive diseases,
even though there is reduced FVC, the patient can exhale 80% or higher in one
second.
1. Explain how TLC is calculated.
2. Describe the importance of surfactant.
3. Explain the diaphragm’s function in respiration.
4. What is the TLC?
Alveolar Ventilation
The total amount of gas flowing into or out of the
respiratory tract in one minute is called the minute ventilation.
In a healthy individual during normal, quiet breathing, this is
approximately 500 mL per breath. At 12 breaths per minute, this is about 6 L of
air. The minute ventilation may increase to 200 L/min during vigorous exercise.
These values help to assess respiratory efficiency.
A better indicator is the alveolar ventilation rate (AVR) because it includes the air in the dead space. It measures the flow of gases into and
out of the alveoli during a certain interval of time. The AVR is calculated by
multiplying the frequency of breaths per minute by the TV minus the dead space,
both in milliliters of air per breath. The AVR is based on millimeters of air
per minute.