Anatomy of the Female Reproductive System
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Reproductive System
Anatomy and Structure of the Female Reproductive System - Ovaries; Female Duct System: Uterine Tubes, Uterus, Uterine Supporting Structures, Layers of the Uterine Wall, Vagina ; External Genitalia ; Mammary Glands
Anatomy
of the Female Reproductive System
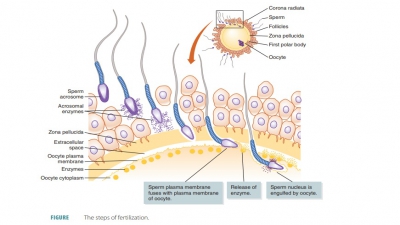
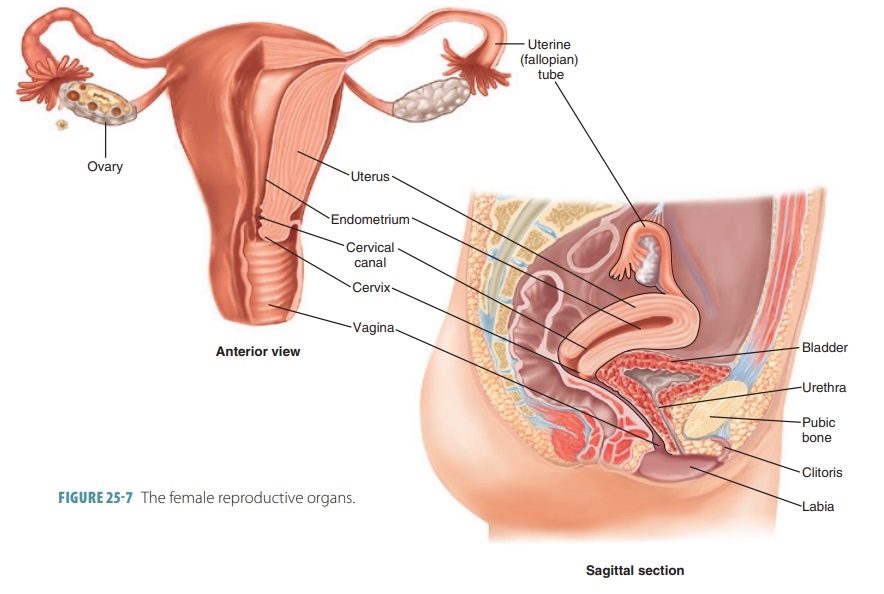
The anatomy of the female reproductive system is highly
complex in comparison with that of the male and the female reproductive and
urinary tracts are totally separated. The female reproductive organs pro-duce
and maintain the egg cells or oocytes, which are the female sex cells. The
organs also transport them to the site of fertilization, provide a strong
environ-ment for the developing fetus, give birth to a fetus, and produce
female sex hormones. The principal organs of the female reproductive system,
besides the ovaries, are the uterine tubes, uterus, vagina, and the compo-nents
of the external genitalia. The
primary sex organs or gonads are the
two ovaries, which reproduce female sex cells and sex hormones. The accessory
sex organs are the internal and external reproductive organs (FIGURE 25-7). As in males, a variety of
accessory glands releases secretions into the female reproductive tract. The
female internal genitalia are primarily located in the pelvic cavity, and
include the ovaries and duct sys-tem. The accessory ducts include the uterine
tubes, uterus, and vagina.
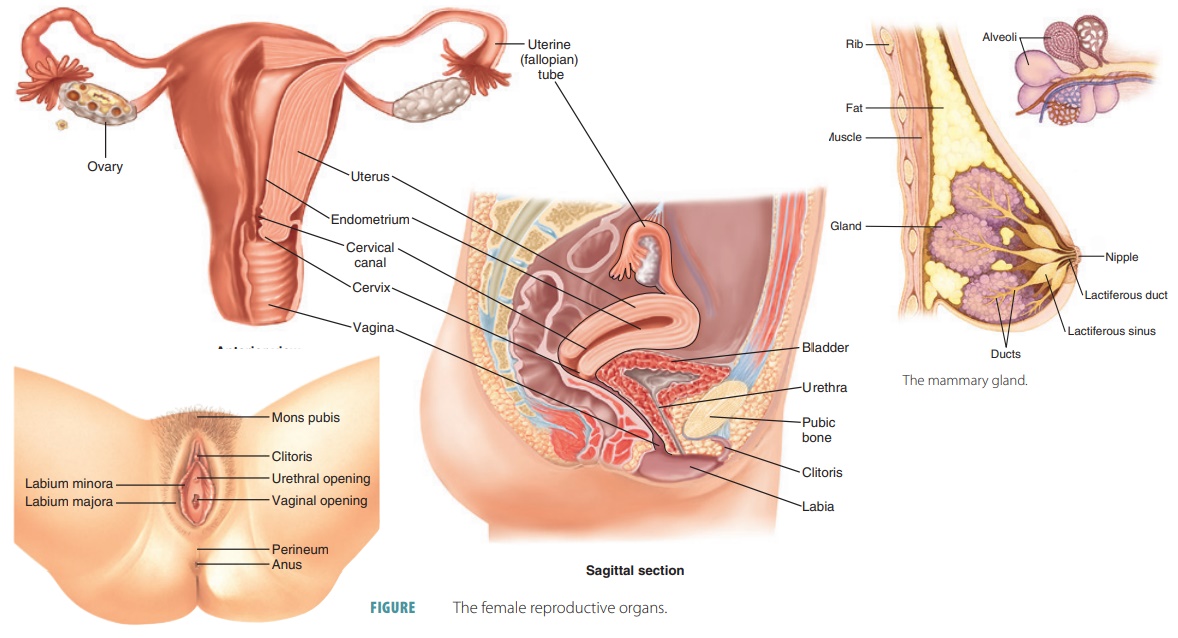
Ovaries
The female gonads or ovaries are oval-shaped, solid structures about 3.5 cm long, 2 cm
wide, and 1-cm thick. They lie in shallow depressions in the lateral pelvic
cavity wall on either side of the uterus. The ova-ries are suspended by several
ligaments in the perito-neal cavity, where the iliac blood vessels split into a
“fork.” Each ovary is anchored medially to the uterus by an ovarian ligament and laterally to the pelvic wall by
the suspensory ligament. Also, a mesovarium
suspends each ovary in between these points. The mesovarium and suspensory ligament are part of a
broad ligament,
which folds over the uterus to sup-port the uterus, uterine tubes, and vagina.
The ovarian ligaments are enclosed by the broad ligament.
The ovarian
arteries serve the ovaries and are branches of the abdominal aorta.
The ovaries are also served by the ovarian branch of the uterine arteries. To
reach the ovaries, the ovarian blood vessels must travel through the mesovaria
and suspensory ligaments.
Each ovary is externally surrounded by a fibrous tunica albuginea. This structure is then
covered by a
cuboidal epithelial cell layer that is known as the germinal epithelium. This epithelium is a continua-tion of the
peritoneum. Each ovary additionally has an outer cortex enclosing the
developing gametes. An inner medulla contains the primary blood vessels and
nerves. However, the relative area of each region is not well defined.
Many small structures called ovarian follicles resemble sacs and are embedded in
the cortex of each ovary, which is highly vascular and made of connective
tissue. One oocyte is found in each folli-cle, encased in a variety of cells.
If only a single layer is present, these are called follicle cells, but if more than one layer is
present, they are called granulosa cells (FIGURE
25-8).
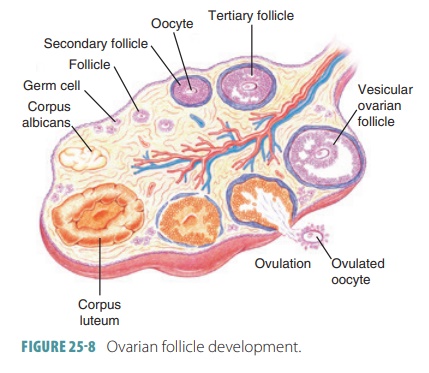
In women of childbearing age, one ripening fol-licle ejects
its oocyte from an ovary every month in a process called ovulation. The ruptured follicle then changes its appearance,
becoming a glandular struc-ture, the corpus
luteum. This structure soon degener-ates. The surfaces of the ovaries show
pits and scars in older women because they have released many oocytes over a
lifetime.
Ovarian tissues consist of an inner medulla and an outer
cortex. The medulla is made up of loose connective tissue with many blood and
lymphatic vessels as well as nerve fibers. The cortex has more compact tissue
with a granular appearance because of masses of ovarian follicles. The ovary’s
free surface is covered with cuboidal epithelium above a layer of dense
connective tissue. The almond-shaped ovaries perform three main functions:
production of imma-ture female gametes called oocytes; secretion of female sex hormones, including estrogens and
progestins; and secretion of inhibin, which is involved in the feed-back
control of pituitary FSH production. The most common form of estrogen is estradiol, followed by estrone and estriol.
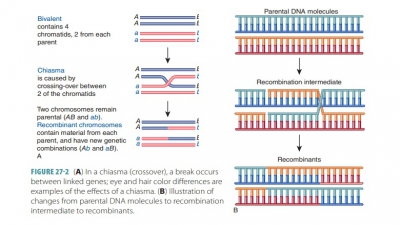
Before birth, a female fetus develops small cell groups in
the outer ovarian cortex that form several million primordial follicles. Each
follicle consists of a primary oocyte surrounded by follicular cells. The
primary oocytes begin to undergo meiosis early in development, but then the
process stops and does not restart until puberty. No new primordial fol-licles
form after the initial ones form, and oocytes degenerate. Although several
million oocytes form in the female embryo, only about 1 million remain at
birth, with only 400,000 left at puberty. The ovary releases less than 400–500
oocytes during a female’s reproductive life.
Female Duct System
The female duct system has no or very little contact with
the ovaries. The female reproductive system includes accessory structures,
including two uterine tubes, a uterus, and a vagina.
Uterine Tubes
The uterine
tubes, also called the fallopian tubes or oviducts, receive the ovulated oocytes from the ovaries and are
each about 10 cm (4 inches) long. The uterine tubes are the sites where
fertilization usually occurs. Each uterine tube empties into the superolateral
area of the uterus via a constricted isthmus. As it curves around the ovary, each uter-ine
tube’s distal end expands to form an ampulla.
Near the ovaries, each tube expands into a funnel shaped infundibulum that partially encircles the
ovary. Finger-like fimbriae surround
its margin with one of the larger extensions connecting with the ovary.
The epithelium lining the uterine tube is com-posed of
ciliated columnar epithelial cells, with scattered mucin-secreting cells. The
mucosa is sur-rounded by concentric smooth muscle layers. The transport of
oocytes involves a combination of cil-iary movement and peristaltic
contractions in the uterine tube walls. Nonciliated mucosal cells have dense
microvilli and produce secretions that keep oocytes as well as any present
sperm nourished and moist. The uterine tubes are externally covered by
peritoneum, supported by a short mesentery called the mesosalpinx. This structure is actually part of
the broad ligament.
Uterus
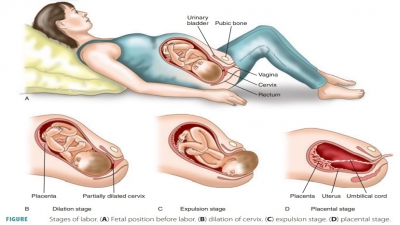
If the secondary oocyte is fertilized to become a zygote,
the uterus receives
the developing embryo, sustaining its development. The uterus is hollow and
muscular, shaped slightly like an inverted pear. Its size changes during
pregnancy, from about 7.5 cm by 5 cm by 2.5 cm to much larger, able to hold the
developing baby up until birth. At this point, it weighs 30–40 g. The uterus is
located in the anterior pelvic cavity, superior to the vagina, usually bending
over the urinary bladder. The uterine body is also called the corpus, the largest portion of the
uterus. The fundus is the
rounded portion of the corpus and is superior to the attachment of the uterine
tubes. It ends at the constriction known as the isth-mus. The cervix is the
inferior portion of the uterus, extending
from the isthmus to the vagina. The cervix surrounds the cervical orifice,
where the uterus opens to the vagina. The uterine wall is thick, with three
layers.
The cervical
canal communicates with the vagina through the external os and also with the uterine
body cavity through the internal os.
Cervical glands exist in the mucosa of the cervical canal and secrete mucus
that fills the cervical canal and also covers the external os. This is believed
to block bac-teria from spreading into the uterus from the vagina. In most
times during the uterine cycle, this cervical mucus blocks sperm entry.
However, it allows sperm to pass through at the midpoint of the cycle, which is
when it becomes less viscous.
Uterine Supporting Structures
Additional supports of the uterus include the mesome-trium, laterally, and other
ligaments. The cardinal lig-aments, also called lateral
cervical ligaments, extend from the cervix and superior vagina to the
lateral pelvic walls more inferiorly than the mesometrium. Two uterosacral ligaments secure the uterus to
the sacrum, posteriorly. Fibrous round
ligaments bind the uterus to the anterior body wall. They
pass through the inguinal canals, anchoring in the labia majora’s subcutaneous
tissue. Collectively, these ligaments allow the uterus to be quite movable,
accommodating filling and emptying of the bladder and rectum.
Layers of the Uterine Wall
The three layers of the wall of the uterus are the perimetrium, myometrium, and endometrium. The perimetrium is the outer, incomplete, serous
layer. The myometrium is the thick middle layer. It is made of interlaced
smooth muscle bundles and contracts rhythmically during childbirth, expelling
the baby from the uterus.
The endometrium is the mucosal lining, made of simple
columnar epithelium above an underlying, thick lamina propria. Fertilization
causes the embryo to implant into the endometrium for the entire preg-nancy.
There are two chief layers or strata
in the endometrium. The functional layer is the stratum functionalis,
which changes based on ovarian hor-mone levels in the blood. This layer is shed
during menstruation, about every 28 days. The basal layer is the stratum basalis, which is thinner. It
forms a new stratum functionalis after menstruation. This layer does not
respond to ovarian hormones. Many uterine glands in the endometrium change
lengthwise, along with the endometrial thickness changes that occur.
The cyclic changes of the uterine endometrium are linked to
its vascular supply. From the internal iliacs of the pelvis arise the uterine arteries. They ascend along the sides of the
uterus, branching into the uterine wall. The branches split into several arcuate arteries inside the myometrium. These
arteries continue as radial arteries into the endometrium.
Here, straight arteries supply
the stratum basalis, whereas spiral,
coiled arter-ies supply the stratum functionalis. The spiral arteries degenerate and regenerate continuously.
When they spasm, these actions cause the functionalis layer to be shed during
the menstrual cycle. In the endometrium, the veins have thin walls. They form
an extensive net-work with small amounts of sinusoidal enlargements.
Painful menstruation is known as dysmenorrhea. It may be caused by inflammation of the uterus,
myo-metrial contractions commonly known as cramps,
or conditions that involve nearby pelvic structures.
Vagina
The vagina is a
thin-walled fibromuscular tube, about 8–10 cm (3–4 inches) in length, extending
from the cervix to the outside of the body. It conveys uterine secretions,
receives the erect penis during intercourse, and provides the open channel for
offspring. The vagina extends up and back into the pelvic cavity and lies
posterior to the urinary bladder and urethra but anterior to the rectum. The
urethra is parallel to the course of the vagina anteriorly. The vagina is
attached to these other structures by connective tissues.
The hymen is a thin
membrane of connective tis-sue and epithelium that partially covers the vaginal orifice in females who have not had sexual inter-course.
It has a central opening that allows uterine and vaginal secretions to pass to
the outside of the body. The hymen is extremely vascular and may bleed when it
stretches or ruptures during initial sexual inter-course. It can also be
ruptured by insertion of tam-pons, sports activities, or pelvic examinations.
In rare cases, it is tougher than normal and requires a surgical procedure for
normal intercourse to occur.
The three major functions of the vagina are to serve as a
passageway for the elimination of menstrual flu-ids, to receive the penis
during sexual intercourse, and to hold the spermatozoa before their passage
into the uterus. The vagina forms the interior portion of the birth canal, through which the fetus passes during delivery.
The vaginal wall has three layers:
■■ Inner
mucosal layer (mucosa): Stratified squamous epithelium with no mucous
glands. Dendritic cells act as antigen-presenting cells. They may be the route
of HIV transmission from an infected male. This layer has no glands but is
lubricated by the cervical mucous glands. It also has a mucosal transudate that
leaks from the vaginal walls. Large amounts of glycogen are released by its
epithelia, which are metabolized anaerobically by bacteria to form lactic acid.
Therefore, the pH is very acidic, which helps to fight infections but is
harmful to sperm. Because this fluid is alkaline instead of acidic in
adolescent girls, they are predisposed to STIs if they are sexually active.
■■ Middle
muscular layer (muscularis): Mostly smooth muscle fibers; helps to close
the vaginal opening.
■■ Outer
fibrous layer (adventitia): Dense connective tissue and elastic fibers.
The vaginal fornix is a recess produced at the upper end of the vaginal canal, which loosely surrounds the cervix. The posterior fornix is much deeper than the lateral and anterior fornices. The lumen of the vagina is basically small, and its posterior and anterior walls touch each other, except where the cervix keeps it open. During sexual intercourse and childbirth, the vagina can stretch considerably. However, ischial spines and the sacrospinous ligaments limit its lateral distention. When various microorganisms cause inflammation and infection of the vagina, it is known as vaginitis.
1. Describe the internal genitalia of females.
2. Explain the roles of the ovaries.
3. Describe the three layers of the uterine wall.
4. Name the suspensory ligaments that support the uterus and
hold it in place.
5. Describe normal and abnormal locations where fertilization
may occur.
External Genitalia
The external accessory organs of the female reproduc-tive
system include the mons
pubis, labia majora, labia minora, clitoris, and vestibular
glands (FIGURE 25-9).They
surround the openings of the urethra and vagina, composing the vulva or pudendum. The mons pubis is a rounded area made of
fatty tissue that overlies the pubic symphysis. This area becomes covered with
pubic hair after puberty.
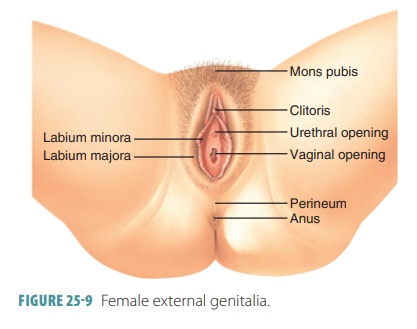
The labia
majora enclose and protect the other external reproductive organs.
They are made up of rounded folds of adipose tissue and thin smooth mus-cle
covered by skin and hair. They lie close together, with a cleft that includes
the urethral and vaginal openings separating the labia longitudinally. The
labia majora are analogous to the male scrotum and enclose the labia minora.
The labia
minora are flattened, hairless longitudi-nal folds composed of
connective tissue. They contain the external openings of the urethra and
vagina. They have a rich blood supply, and therefore a pinkish appear-ance.
They merge posteriorly with the labia majora to form a ridge called the fourchette. Anteriorly, they converge to form
the hood-like covering of the clitoris.
The clitoris projects
from the anterior end of the vulva between the labia minora. It is usually
about 2 cm in length and 0.5 cm in diameter. It corresponds to the penis in
males, with a similar structure. It is made up of two columns of erectile
tissue called the corpora cavernosa and forms a glans at its
anterior end that has many sensory
nerve fibers. The exposed portion is called the glans of the clitoris and the hooded fold is called the prepuce of the clitoris. The clitoris
has a rich innervation of sensory
nerve endings and swells with blood, becom-ing erect during tactile stimulation
and sexual arousal.
The labia minora encloses the vestibule, into which the vagina opens posteriorly. The urethra opens
into the vestibule in the midline, about 2.5 cm posterior to the glans of the
clitoris. One pea-sized vestibular
gland lies on each side of the vaginal opening, which is similar
to the bulbourethral glands of males. They release mucus into the vestibule,
moist-ening and lubricating it for intercourse. Under the vestibule’s mucosa,
on either side, is a mass of vascular erectile tissue called the vestibular bulb. These bulbs are similar to the
single penile bulb and corpus spon-giosum in males. They engorge with blood
during sex-ual stimulation, helping the vagina to grip the penis and causing
the urethral orifice to shut. This prevents semen and bacteria from moving
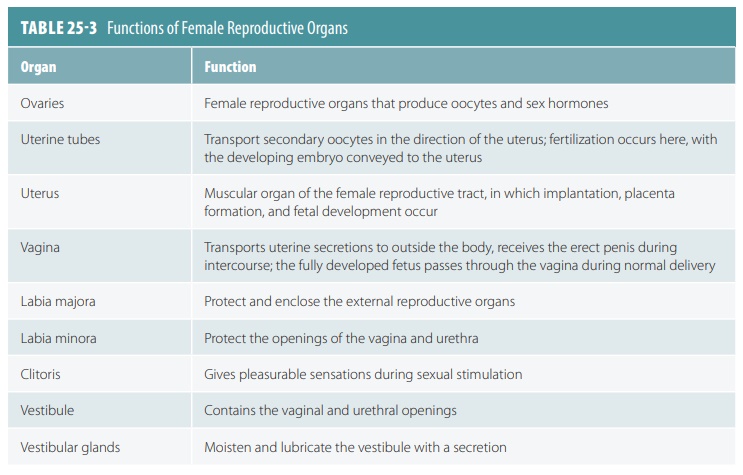
superiorly into the bladder as intercourse occurs. TABLE 25-3 summarizes the functions of the female reproductive organs.
Mammary Glands
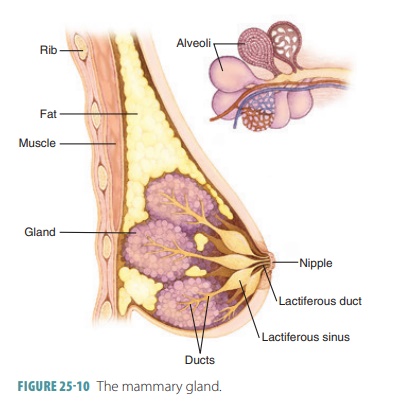
The mammary
glands are specialized to secrete milk after pregnancy. They are
located in the subcutane-ous tissue of the anterior thorax within the breasts.
The breasts are above the pectoralis major muscles, extending from the second
to the sixth ribs, from the sternum to the axillae. They lie within the
superficial fascia, also known as the hypodermis.
The subcutane-ous tissue of a pectoral
fat pad, which is deep to the skin of the chest, contains each mammary
gland.
Just below the center of each breast is an areola, which is a ring of pigmented skin. The areola is slightly
bumpy because of large sebaceous glands and produces sebum to reduce cracking
and chapping of the nipple, which is
located near the tip of each breast within the areola surrounding it (FIGURE 25-10). Smooth muscle fibers in the
areola and nipple are controlled by the autonomic nervous system. This can
cause the nipple to become erect when it is stimulated by touch or cold
temperatures. Although present in males, the mam-mary glands have no function.
Each mammary gland is a modified sweat gland made up of
15–25 lobes that contain alveolar glands and an alveolar duct, which leads to a
lactiferous duct. This leads to the nipple. The lobes are separated by dense
adipose and connective tissues. Dense suspensory ligaments
extend inward to help support the weight of the breast. Lobules are smaller units inside the lobes. They contain glandular alveoli, which produce milk during
lactation. Milk is passed from these compound alveolar glands into lactiferous ducts, which open to the
outside of the nipple. Each duct, just below the are-ola, has a dilated lactiferous sinus, where milk
accumu-lates during nursing. As female children reach puberty, their mammary
glands develop because of ovarian hormones. The alveolar glands and ducts
enlarge. Fatty tissue deposits around and within the breasts.
1. Describe the structures of the external genitalia.
2. Explain the components of the mammary glands.
3. Identify
risk factors for breast cancer.