Entamoeba histolytica - Intestinal Parasites
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Protozoa
Entamoeba histolytica is the causative agent of amoebic dysentery, another infection transmitted via the faecal– oral route. The severity of this and related pathologies caused by this organism can vary from diarrhoea associated with the intestinal infection to extraintestinal amoebiasis producing hepatic and often lung infection.
Entamoeba histolytica
Entamoeba histolytica is the causative agent of amoebic dysentery, another infection transmitted
via the faecal– oral route. The severity of this and related pathologies caused
by this organism can vary from diarrhoea associated with the intestinal
infection to extraintestinal amoebiasis producing hepatic and often lung
infection. The prevalence of amoebiasis in developing countries reflects the
lack of adequate sanitary systems. It had long been known that most infections
associated with E. histolytica are
asymptomatic or exhibit minimal symptomology, but in the late 1980s a separate,
but morphologically and biochemically similar species, E. dispar, was identified. This organism exhibits limited
pathogenicity and in many cases produces no symptoms but is commonly
misidentified as E. histolytica. This
species is the most likely cause of ‘asymptomatic Entamoeba infection’.
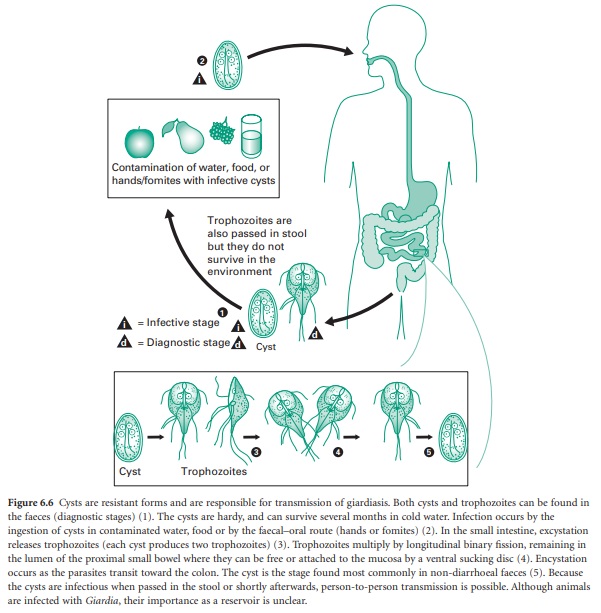
E. histolytica has a relatively simple life cycle and, like Giardia , exhibits only two
morphological forms: the trophozoite and cyst stages. Trophozoites (Figure
6.2e) vary in size from 10 to 60 μm and are actively motile. The cyst is spherical, 10–20 μm in diameter, with a thin transparent wall.
Fully mature cysts contain four nuclei.
Symptoms of amoebic
dysentery are associated with mucosal invasion and ulceration. Mucosal erosion
causes diarrhoea, the severity of which increases with the level of invasion
and colonization. Symptoms can also be affected by the site of the infection.
Peritonitis as a result of perforation has been reported in connection with
severe amoebic infection. Extraintestinal amoebiasis is usually associated with
liver infection, causing abscesses and/or enlargement. The abscess appears as a
slowly enlarging liver mass and will cause noticeable pain. Jaundice may also
occur due to blockage of the bile. Pleural, pulmonary, and pericardial
infection results from metastatic spread from the liver, but can also manifest
in other parts of the viscera or give rise to a brain abscess. However, these
complications are uncommon.
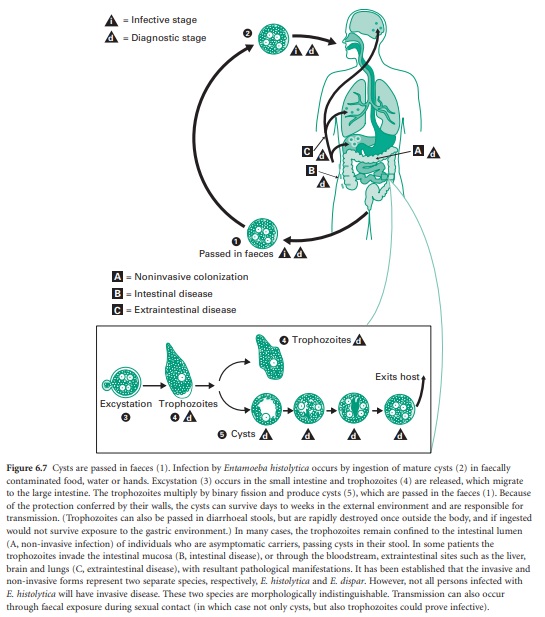
The life cycle of E. histolytica (Figure 6.7) is simple,
but the ability of trophozoites to infect sites other than the intestine make
it more complex than that of Giardia.
Infection is initiated by ingestion of mature cysts, and again, excystation
occurs during transit through the gut. After this, trophozoites rapidly divide
by simple fission to produce four amoebic cells which undergo a second division;
thus each cyst yields eight trophozoites. Survival outside the host depends on
the resistant cyst form.
The pathology of the
disease is only partially understood. The process of tissue invasion has been
well studied and involves binding and killing of the host cells by specific
adhesin molecules and the action of a poreforming protein, amoebapore. The
initial superficial ulcer may deepen into the submucosa and become chronic.
Spread may occur by direct extension, by undermining of the surrounding mucosa
until it sloughs, or by penetration that can lead to perforation. If the
trophozoites gain access to the vascular or lymphatic circulation, metastases may
occur first to the liver and then by direct extension or further metastasis to
other organs, including the brain.
Related Topics
