Life Cycle of Plasmodia (Malarial causative)
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Protozoa
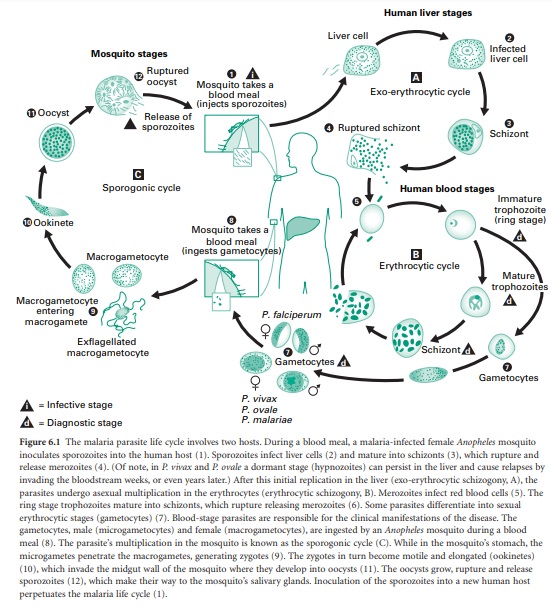
Plasmodia have a complex life cycle involving a number of life cycle stages and two hosts. The human infective stage comprises the sporozoites ( c.1–7 μm), which are produced by sexual reproduction in the midgut of the mosquito (vector) and migrate to its salivary gland.
LIFE CYCLE OF PLASMODIA (MALARIAL CAUSATIVE)
Plasmodia have a complex
life cycle (Figure 6.1) involving a number of life cycle stages and two hosts.
The human infective stage comprises the sporozoites ( c.1–7 μm), which are produced
by sexual reproduction in the midgut of the mosquito (vector) and migrate to
its salivary gland. When an infected Anopheles
mosquito bites a human, sporozoites are injected into the bloodstream and are
thought to enter liver parenchymal cells within 30 minutes of inoculation. In
these cells the parasite differentiates into a spherical, multinucleate
schizont which may contain 2000–40 000 uninucleate merozoites. This process of
growth and development is termed exoerythrocytic
schizogony. This exoerythrocytic phase usually takes between 5 and 21 days, depending on the species of Plasmodium; however, in P. vivax and P. ovale the maturation of schizonts may be delayed for up to 1–2
years. These ‘quiescent’ parasites are called hypnozoites. Clinical illness is caused by the erythrocytic stage
of the parasite life cycle; no disease is associated with sporozoites, the
developing liver stage of the parasite, the merozoites released from the liver,
or gametocytes.
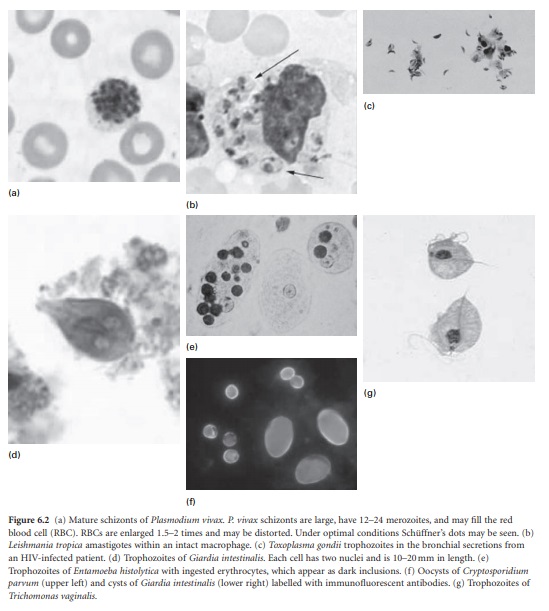
The common symptoms of
malaria are due to the rupture of erythrocytes when erythrocytic schizonts
mature (Figure 6.2a). This release of parasite material triggers a host immune
response, which in turn induces the formation of inflammatory cytokines,
reactive oxygen intermediates and other cellular products. These proinflammatory
molecules play a prominent role in pathogenesis, and are probably responsible
for the fever, chills, sweats, weakness and other systemic symptoms associated
with malaria. In P. falciparum
malaria, infected erythrocytes adhere to the endothelium of capillaries and
postcapillary venules, leading to obstruction of the microcirculation and
localized anoxia. The pathogenesis of anaemia appears to involve haemolysis or
phagocytosis of parasitized erythrocytes and ineffective erythropoiesis.
Related Topics
