Alternative Strategies for Antimicrobial Therapy
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Alternative Strategies For Antimicrobial Therapy
Most of us have no notion of what life would be like without antibiotics. Penicillin was discovered in 1928 and after a lengthy developmental period became available for clinical use in the 1940s.
ALTERNATIVE
STRATEGIES FOR ANTIMICROBIAL THERAPY
INTRODUCTION
Most of us have no notion of what life
would be like without antibiotics. Penicillin was discovered in 1928 and after
a lengthy developmental period became available for clinical use in the 1940s.
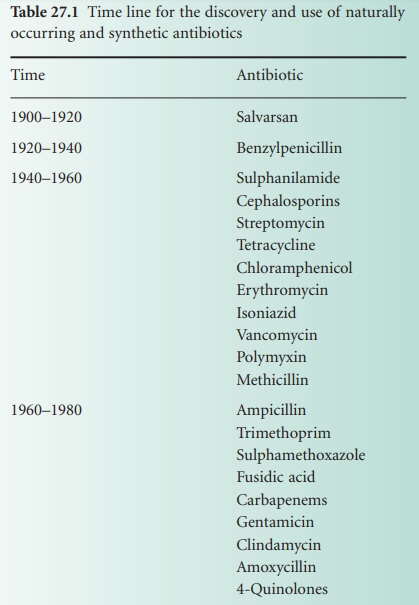
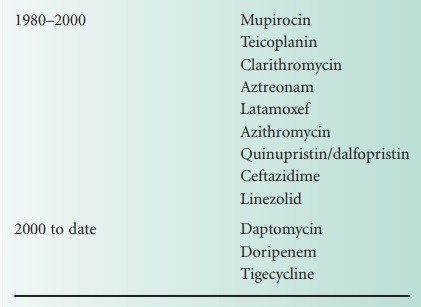
Then followed what is often referred to as the golden era of antibiotic
discovery which brought us the cephalosporins, the tetracyclines, the
macrolides, the aminoglycosides, the 4-quinolones, etc. (Table 27.1).
It is interesting to note that the impact of antibiotic discovery was
sufficient to halt the development of virtually all other antimicrobial
therapies being pursued at that time. The fact that Alexander Fleming in the
early years had flagged up the probability of resistance development in
bacterial pathogens was largely ignored because of the constant stream of new
agents on to the market. There is anecdotal evidence that in 1967 the US
Surgeon General stated ‘… it is time to close the book on infectious disease,
declare the war against pestilence won…’. Whether or not he actually said this
is debatable, but it represented a widely held view at the time that the stream
of antibiotic discovery would never dry up. However, we now know that is
precisely what has happened.
At present we are faced with two major
issues—we have seen an inexorable rise in the incidence of antibiotic
resistance among the most important bacterial pathogens, while at the same time
the development of novel antibacterial antibiotics has all but stopped. Some
clinical isolates from species such as Pseudomonas aeruginosa,
Acinetobacter baumannii, Enterococcus faecium and Mycobacterium tuberculosis are resistant to
virtually every antibiotic we have at our disposal. It is not appropriate here
to discuss the issue of antibiotic resistance, other than to say it is an
almost inevitable event occurring as a consequence of the bacterial cell’s
remarkable adaptability to environmental change. Without this ability to adapt
to their environment bacteria would not still be thriving 3.5 billion years
after first emerging on to what was at that time an extremely hostile earth.
Suffice it to say there is very little we can do to stop this process.
The second issue of antibiotic discovery and development is, of course,
under our control. We have the scientific ingenuity to devise novel approaches
to circumvent the resistance mechanisms put in place by these bacteria. Unfortunately,
the driving force behind drug discovery is not based on altruism but has a
financial imperative. The cost of bringing a new chemical entity to the market
has been estimated as $800 million or more, while the process of development
takes about 8 years. Antibiotics simply do not generate sufficient revenue to
justify this initial outlay of time and cost, and not surprisingly the focus
for the large pharmaceutical companies has switched to those medicines which
patients will take long-term such as statins, antidepressants and
antihypertensives. The market for antiviral agents, particularly those to treat
HIV/AIDS, remains buoyant simply because the patients will be taking the
medicines for the remainder of their lives.
All this poses the question, ‘How in the near future will clinicians be
able to treat patients with infections caused by multiresistant bacterial
pathogens?’ In reality this is a question which is relevant today but will only
become more pressing in the future. Some respected authorities in the field
have already expressed the view that we are on the verge of entering a
postantibiotic era.
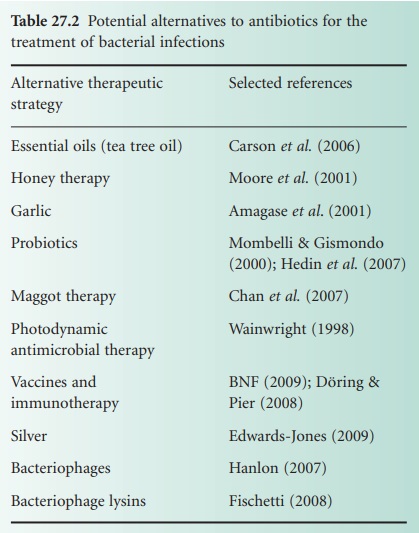
This article examines a range of alternative
therapeutic strategies available for the management of infectious disease (Table 27.2). As we will see, a
number of the techniques to be described have a very long history, some of them
going back many centuries. Some of these have very little chance of ever moving
from the fringes of medicine, some may have the potential to be useful but in
reality suffer from the same developmental issues as conventional antibiotics,
some are niche approaches which may find relevance in specific clinical areas,
while a few may offer a realistic alternative, or at least an adjunct, to
antibiotics.