Antihistamines
| Home | | Medicinal Chemistry |Chapter: Medicinal Chemistry : Antihistamines
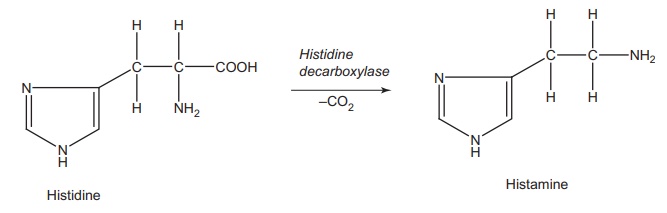
Histamine, [2-(imidazol-4-y1) ethylamine], which is biosynthesized by decarboxylation of the basic amino acid histidine, is found in all organs and tissues of the human body.
Antihistamines
INTRODUCTION
Histamine,
[2-(imidazol-4-y1) ethylamine], which is biosynthesized by decarboxylation of
the basic amino acid histidine, is found in all organs and tissues of the human
body.
The
histamine is stored in the secretory granules of mast cells (pH 5.5) as
positively charged and ionically complexed with negatively charged acidic group
on other seceretory granules, which constitutes heparin. The principal target
cells of immediate hypersensitivity reactions are mast cells and basophils to
generate IgE antibodies that binds to FC€ receptor on the granule surface. This
leads to transmembrane activation of tyrosine protein kinase, which
phosphorylates and activates the phospolipase. The phosphotidyl inositol
biphosphate is converted into inositol triphosphate, which triggers the
intracellular release of calcium ion. The calcium ion causes exocytic release of
histamine with the transfer of Na+ ion from extracellular space. The released
histamine targets the histaminergic receptors (H1, H2,
and H3) to elicit the actions.
Histamine is
an important chemical messenger, communicating information from one cell to another,
and is involved in a variety of complex biological actions. It is mainly stored
in an inactive bound form, from which it is released as a result of an
antigen–antibody reaction, initiated by different stimuli, such as venoms, toxins, proteolytic enzyme,
detergents, food materials, and numerous chemicals. Systemically, histamine
contracts smooth muscles of the lungs and the gastrointestinal system and cause
vasodialation, low blood pressure, and increases the heart rate. It also causes
symptoms such as itching, sneezing, watery eye, and running nose.
Histamine
exerts its biological function by interacting with at least three distinctly
specific receptors H1,
H2, and H3. Historically, the term antihistamine has been
used to describe a drug that acts on H1 and H2 receptors.
An antihistaminic agent should ideally prevent the production or release of
these autocoids by inhibiting the response of sensitized mast cells and
basophils to specific antigens.
1.
Antihistamines
are drugs that competitively blocks the H1 receptors.
2.
Antihistamines
antagonize the stimulant action of histamine on the smooth muscles of gastro
intestinal tract (GIT), uterus, and blood vessels, and inhibit histamine
augmented salivary secretion.
3.
H1-receptor
antagonists have been used clinically to treat various allergic disorders, such
as seasonal or perennial allergic rhinitis and chronic urticaria.
Release and Function of Endogenous Histamine
Histamine is
released because of the interaction of an antigen with IgE antibodies on the
mast cell surface and plays a central role in immediate hypersensitive
reactions (Fig. 1.1).
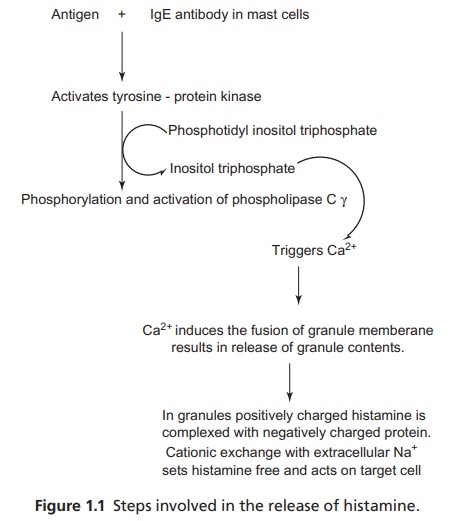
The release of histamine, in addition to the stimulation of IgE receptors, also activates the phospholipase A2, leading to the production of host mediators, including platelet activating factors and metabolites of arachidonic acid. Leukotriene D4 is also generated, which is a potent constrictor of smooth muscles. This mediates the constriction of bronchi.
Histamine and Gastric Acid Secretion
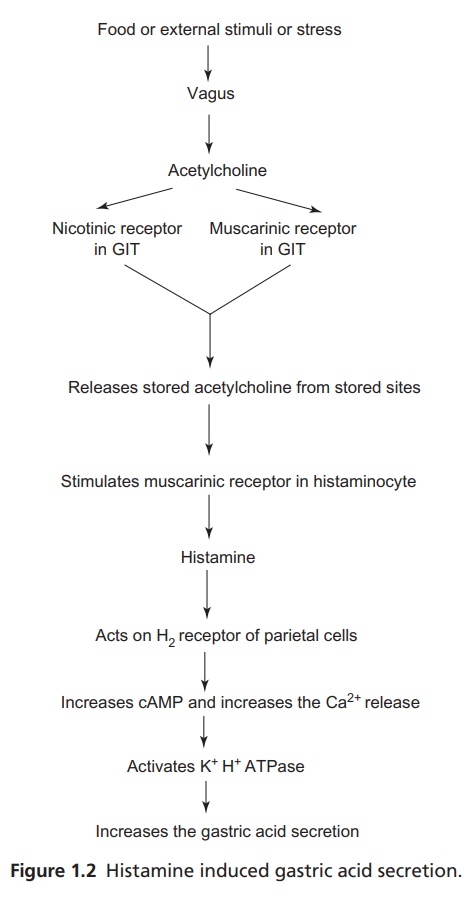
Histamine is
a powerful gastric acid secretagogue and evokes a copious secretion of acid
from the parietal cells by acting on the H2 receptors. The output of
pepsin and intrinsic factors are also increased. However, the secretion of acid
is evoked by the stimulation of vagus nerve and by the enteric hormone gastrin.
The mechanism operating at the gastric parietal cells is through H+
K+ ATPase (proton pump), which secretes H+ ions in the
apical canaliculi of parietal cells and also which can be activated by
histamine (Fig. 1.2).
The
therapeutically available antagonists of histamine receptors are used as
antiallergic drugs by targeting H1 receptors and as antiulcers by
targeting H2 receptors.
Mode of Action of Antihistamines
After the
release of histamine by the mast cells, it binds with histaminergic receptors
(H1, H2, and H3) to elicit a series of events
that mediates the characteristic responses through second messenger systems.
The histaminergic receptors are G-protein coupled type. H1 receptors
are coupled to phospholipase-C and their activation leads to the formation of
inositol phosphate (Ip3) and diacylglycerol (DAG), respectively,
from phospholipids in cell membrane. Ip3 causes rapid release of Ca2+
from endoplasmic reticulum. DAG activates the protein kinase C. Altogether the
turnover of Ca2+ and protein kinase-C activates Ca2+/calmodulin
dependent protein kinase and phospholipase A2. The antihistaminergic
(H1-antagonist) binds to the H1 receptors and decreases
the production of phospholipase-C and their activation to form IP3
and DAG thereby blocks the characteristic response of histamine.
Histamine on
H2 receptors produces cAMP-dependent protein kinase (Cyclic adenosine monophosphate (cAMP), also known as cyclic AMP or
3’-5’-cyclic adenosine monophosphate) to elicit a response in the GIT. The H2
antagonist reversibly binds the H2 receptors and reduces the cAMP
formation, which is responsible for the activation of proton pump and,
subsequently, reduces the gastric acid formation in the GIT.
H3
receptors are also G-protein coupled receptors, unlike H1 and H2,
and they produce a decreased Ca2+ influx. H3 receptors
function as feedback inhibitors for histamine and other neurotransmitters by
decreasing the calcium influx into the cells in the central nervous system
(CNS), and in the GIT, they reduce the secretion of gastrin and down-regulates
histamine through auto-regulatory effects. Blocking H3 receptors antagonize
these effects, but the clinical extendibility is narrow for H3.
Related Topics
