Antipsychotic Drugs
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs Used In Mental Illness: Antipsychotic And Antimanic Drugs
These are drugs having a salutary therapeutic effect in psychoses.
ANTIPSYCHOTIC DRUGS
(Neuroleptics)
These are drugs having
a salutary therapeutic effect in psychoses.
Classification
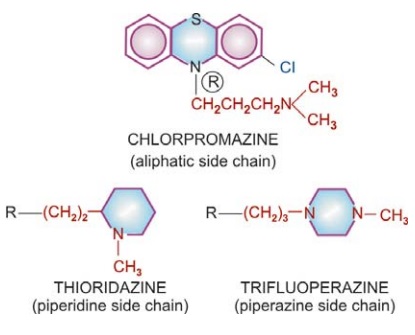
1. Phenothiazines
Aliphatic side chain: Chlorpromazine,Triflupromazine
Piperidine side chain: Thioridazine
Piperazine side chain: Trifluoperazine,
Fluphenazine
2. Butyrophenones
Haloperidol
Trifluperidol
Penfluridol
3.Thioxanthenes
Flupenthixol
4.Other heterocyclics
Pimozide
Loxapine
5.Atypical antipsychotics
Clozapine
Risperidone
Olanzapine
Quetiapine
Aripiprazole
Ziprasidone
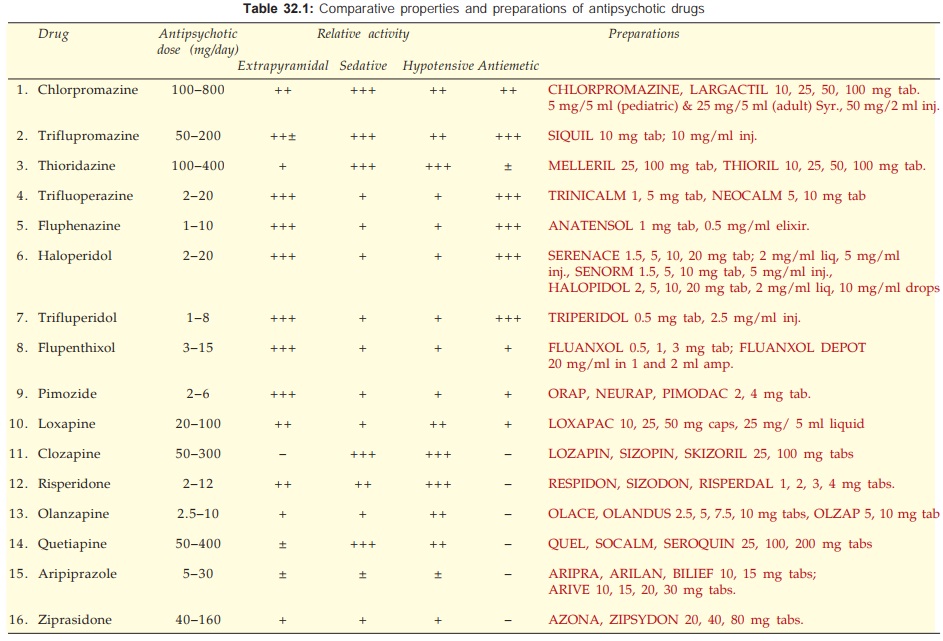
Many more drugs have been marketed in other countries but do not
deserve special mention. Pharmacology of chlorpromazine (CPZ) is described as
prototype; others only as they differ from it. Their comparative features are presented
in Table 32.1.
Pharmacological Actions
1. CNS
Effects differ in normal
and psychotic individuals.
In normal individuals CPZ produces
indifference to surroundings,
paucity of thought, psychomotor slowing, emotional quietening, reduction in
initiative and tendency to go off to sleep from which the subject is easily arousable.
Spontaneous movements are minimized but slurring of speech, ataxia or motor
incoordination does not occur. This has been referred to as the ‘neuroleptic
syndrome’ and is quite different from the sedative action of barbiturates and
other similar drugs. The effects are appreciated as ‘neutral’ or ‘unpleasant’
by most normal individuals.
In a psychotic CPZ reduces irrational
behaviour, agitation and aggressiveness and controls psychotic symptomatology.
Disturbed thought and behaviour are gradually normalized, anxiety is relieved.
Hyperactivity, hallucinations and delusions are suppressed.
All phenothiazines,
thioxanthenes and butyrophenones have the same antipsychotic efficacy, but
potency differs in terms of equieffective doses. The aliphatic and piperidine side
chain phenothiazines (CPZ, triflupromazine, thioridazine) have low potency,
produce more sedation and cause greater potentiation of hypnotics, opioids,
etc. The sedative effect is produced promptly, while antipsychotic effect takes
weeks to develop. Moreover, tolerance develops to the sedative but not to the
antipsychotic effect. Thus, the two appear to be independent actions.
Performance and
intelligence are relatively unaffected, but vigilance is impaired. Extrapyramidal
motor disturbances (see adverse
effects) are intimately linked to the antipsychotic effect, but are more
prominent in the high potency compounds and least in thioridazine, clozapine
and other atypical antipsychotics. A predominance of lower frequency waves
occurs in EEG and arousal response is dampened. However, no consistent effect
on sleep architecture has been noted. The disturbed sleep pattern in a
psychotic is normalized.
Chlorpromazine lowers
seizure threshold and can precipitate fits in untreated epileptics. The piperazine
side chain compounds have a lower propensity for this action. Temperature
control is knocked off at relatively higher doses rendering the individual
poikilothermic—body temperature falls if surroundings are cold. The medullary
respiratory and other vital centres are not affected, except at very high
doses. It is very difficult to produce coma with these drugs. Neuroleptics,
except thioridazine, have potent antiemetic action exerted through the CTZ. However,
they are ineffective in motion sickness.
In animals, neuroleptics
selectively inhibit ‘conditioned avoidance response’ (CAR) without
blocking the unconditioned response to a noxious stimulus. This action has
shown good correlation with the antipsychotic potency of different compounds, though
it may be based on a different facet of action. In animals, a state of rigidity
and immobility (catalepsy) is produced which resembles the bradykinesia seen
clinically.
Mechanism Of Action
All antipsychotics
(except clozapinelike
atypical) have potent dopamine D2 receptor blocking action; antipsychotic
potency has shown good correlation with their capacity to bind to D2 receptor.
Phenothiazines and thioxanthenes also block D1, D3 and D4 receptors, but there
is no correlation with antipsychotic potency. Blockade of dopaminergic
projections to the temporal and prefrontal areas constituting the ‘limbic
system’ and in mesocortical areas is probably responsible for the antipsychotic
action. This along with the observation that drugs which increase DA activity
(amphetamines, levodopa, bromocriptine) induce or exacerbate schizophrenia has
given rise to the ‘Dopamine theory of
Schizophrenia’ envisaging DA overactivity in limbic area to be responsible
for the condition. As an adaptive change to blockade of D2 receptors, the firing
of DA neurones and DA turnover increases initially. However, over a period of
time this subsides and gives way to diminished activity, especially in the
basal ganglia—corresponds to emergence of parkinsonian side effect. Tolerance
to DA turnover enhancing effect of antipsychotics is not prominent in the
limbic area—may account for the continued antipsychotic effect.
The above model fails
to explain the antipsychotic activity of clozapine and other atypical
antipsychotics which have weak D2 blocking action. However, they have
significant 5HT2 and α1 blocking action, and
some are relatively selective for D4 receptors. Thus, antipsychotic property
may depend on a specific profile of action of the drugs on several
neurotransmitter receptors. Recent positron emission tomography (PET) studies of
D2 and other receptor
occupancy in brains of
antipsychotic treated patients have strengthened this concept.
Dopaminergic blockade
in the basal ganglia appears to cause the extrapyramidal symptoms, while that
in CTZ is responsible for antiemetic action.
2. ANS
Neuroleptics have
varying degrees of α adrenergic blocking
activity which may be graded as:
CPZ = triflupromazine
> thioridazine > clozapine > fluphenazine > haloperidol >
trifluoperazine > pimozide, i.e. more potent compounds have lesser α blocking activity.
Anticholinergic
property of neuroleptics is weak and may be graded as:
thioridazine > CPZ
> triflupromazine > trifluoperazine = haloperidol.
The phenothiazines
have weak H1antihistaminic and anti5HT actions as well.
3. Local Anaesthetic
Chlorpromazine is as potent a local anaesthetic as procaine.
However, it is not used for this purpose because of its irritant action. Others
have weaker membrane stabilizing action.
4. CVS
Neuroleptics produce
hypotension (primarily postural) by a central as well as peripheral action on
sympathetic tone. The hypotensive action is more marked after parenteral
administration and roughly parallels the α adrenergic blocking
potency. Hypotension is not prominent in psychotic patients, but is accentuated
by hypovolemia. Partial tolerance develops after chronic use. Reflex
tachycardia accompanies hypotension.
High doses of CPZ
directly depress the heart and produce ECG changes (QT prolongation and
suppression of T wave). CPZ exerts some antiarrhythmic action, probably due to
membrane stabilization. Arrhythmia may occur in overdose, especially with thioridazine.
5. Skeletal
Muscle
Neuroleptics have no effect on muscle fibres or neuromuscular transmission. They reduce certain types of spasticity: the site of action being in the basal ganglia or medulla oblongata. Spinal reflexes are not affected.
6. Endocrine
Neuroleptics
consistently increase prolactin release by blocking the inhibitory action of DA
on pituitary lactotropes. This may result in galactorrhoea and gynaecomastia.
They reduce gonadotropin secretion, but amenorrhoea and
infertility occur only occasionally. ACTH release in response to stress is
diminished—corticosteroid levels fail to increase under such circumstances.
Release of GH is also reduced but this is not sufficient to cause growth
retardation in children or to be beneficial in acromegaly. Decreased release of
ADH may result in an increase in urine volume. A direct action on kidney
tubules may add to it, but Na+ excretion is not affected.
Tolerance And Dependence
Tolerance to the sedative and hypotensive actions develops
within days or weeks, but maintenance doses in most psychotics remain fairly
unchanged over years, despite increased DA turnover in the brain. The
antipsychotic, extrapyramidal and other actions based on DA antagonism do not
display tolerance.
Neuroleptics are hedonically (pleasurably) bland drugs. Physical
dependence is probably absent, though some manifestations on discontinuation
have been considered withdrawal phenomena. No drug seeking behaviour is
exhibited.
Pharmacokinetics
Oral absorption of CPZ is somewhat unpredictable and
bioavailability is low. More consistent effects are produced after i.m. or i.v.
administration. It is highly bound to plasma as well as tissue proteins—brain
concentration is higher than plasma concentration. Volume of distribution,
therefore, is large (20 L/kg). It is metabolized in liver, mainly by CYP 2D6
into a number of metabolites.
The acute effects of a
single dose generally last for 6–8 hours. The elimination t½ is variable, but
mostly is in the range of 18–30 hours. The drug cumulates on chronic
administration and it is possible to give the total maintenance dose once a
day. Some metabolites are probably active. The intensity of antipsychotic
action is poorly correlated with plasma concentration. Nevertheless,
therapeutic effect may be seen at 30–200 ng/ ml. The metabolites are excreted
in urine and bile for months after discontinuing the drug.
The broad features of
pharmacokinetics of other neuroleptics are similar.
Distinctive Features Of Neuroleptics
Antipsychotic drugs differ in potency and in their propensity to produce different effects. This is summarized in a comparative manner in Table 32.1.
Triflupromazine
An aliphatic side chain phenothiazine, somewhat more potent than CPZ.
Used mainly as antiemetic; it frequently produces acute muscle dystonias in
children; especially when injected.
Thioridazine
A low potency
phenothiazine having marked central
anticholinergic action. Incidence of extrapyramidal side effects is very low.
Cardiac arrhythmias and interference with male sexual function are more common.
Risk of eye damage limits long-term use.
Trifluoperazine,
Fluphenazine
These are high potency piperazine side chain phenothiazines.
They have minimum autonomic actions. Hypotension, sedation and lowering of
seizure threshold are not significant. They are less likely to cause jaundice
and hypersensitivity reactions. However, extrapyramidal side effects are
marked.
Fluphenazine decanoate
can be given as a depot i.m. injection every 2–4 weeks.
ANATENSOL DECANOATE,
PROLINATE 25 mg/ml inj.
Haloperidol
It is a potent antipsychotic with pharmacological
profile resembling that of piperazine substituted phenothiazines. It produces few
autonomic effects, is less epileptogenic, does not cause weight gain, jaundice
is rare. It is the preferred drug for acute schizophrenia, Huntington’s disease
and Gilles de la Tourette’s syndrome. Elimination t½ averages 24 hours.
Trifluperidol
It is similar to but slightly more potent than
haloperidol.
Penfluridol
An exceptionally long
acting neuroleptic,
recommended for chronic schizophrenia, affective withdrawal and social maladjustment.
Dose: 20–60 mg (max 120 mg)
once weekly; SEMAP, FLUMAP, PENFLUR 20 mg tab.
Flupenthixol
It is less sedating
than CPZ; indicated in
schizophrenia and other psychoses, particularly in withdrawn and apathetic
patients, but not in those with psychomotor agitation or mania. Infrequently
used now.
Pimozide
It is a specific DA antagonist with little α adrenergic or
cholinergic blocking activity. Because of long duration of action (several
days; elimination t½ 48–60 hours) after a single oral dose, it is considered
good for maintenance therapy but not when psychomotor agitation is prominent.
Incidence of dystonic reactions is low, but it tends to prolong myocardial APD
and carries risk of arrhythmias. It has been particularly used in Gilles de la
Tourett’s syndrome and ticks.
Loxapine
A dibenzoxazepine
having CPZ like DA blocking and
antipsychotic activity. The actions are quick and short lasting (t½ 8 hr). No
clear cut advantage over other antipsychotics has emerged.
Atypical Antipsychotics
These are newer
(second generation) antipsychotics that have weak D2 blocking but potent 5HT2
antagonistic activity. Extrapyramidal side effects are minimal, and they may
improve the impaired cognitive function in psychotics.
Clozapine
An atypical
antipsychotic; pharmacologically distinct from others in that it has only weak
D2 blocking action, produces few/no extrapyramidal symptoms; tardive dyskinesia
is rare and prolactin level does not rise. It suppresses both positive and
negative symptoms of schizophrenia and many patients refractory to typical
neuroleptics respond. The differing pharmacological profile may be due to its
relative selectivity for D4 receptors (which are sparse in basal ganglia) and
additional 5HT2 as well as α blockade. It is quite sedating, moderately
potent anticholinergic, but paradoxically induces hypersalivation. Significant
H1 blocking property is present.
Clozapine is
metabolized primarily by CYP3A4 with an average t½ of 12 hours. Its major
limitation is higher incidence of agranulocytosis (0.8%) and other blood
dyscrasias: weekly monitoring of leucocyte count is required. High dose can
induce seizures even in nonepileptics. Other side effects are sedation,
unstable BP, tachycardia, urinary incontinence, weight gain and precipitation
of diabetes. Few cases of myocarditis have been reported which start like flu
but may progress to death.
Clozapine is used as a
reserve drug in resistant schizophrenia.
Risperidone
Another compound whose antipsychotic activity has been ascribed to a
combination of D2 + 5HT2 receptor blockade. In addition it has high
affinity for α1, α2 and H1
receptors: blockade of these may contribute to efficacy as well as side effects
like postural hypotension. However, BP can rise if it is used with selective
serotonin reuptake inhibitors. Risperidone is more potent D2 blocker than clozapine;
extrapyramidal side effects are less only at low doses (<6 mg/day).
Prolactin levels rise during risperidone therapy, but it is less epileptogenic
than clozapine, though frequently causes agitation. Caution has been issued
about increased risk of stroke in the elderly.
Olanzapine
This atypical antipsychotic; resembles clozapine in
blocking multiple monoaminergic (D2, 5HT2, α1, α2) as well as
muscarinic and H1 receptors. Both positive and negative symptoms of
schizophrenia appear to be benefited. A broader spectrum of efficacy covering
schizoaffective disorders has been demonstrated, and it is approved for use in
mania. Monotherapy with olanzapine may be as effective as a combination of
lithium/valproate + benzodiazepines.
Olanzapine is a potent antimuscarinic, produces dry mouth and
constipation. Weaker D2 blockade results in few extrapyramidal side effects and
little rise in prolactin levels, but is more epileptogenic than high potency
phenothiazines; causes weight gain and carries a higher risk of worsening
diabetes. Incidence of stroke may be increased in the elderly. Agranulocytosis
has not been reported with olanzapine. Olanzapine is metabolized by CYP1A2 and
glucuronyl transferase. The t½ is 24–30 hours.
Quetiapine
This new short-acting (t½ 6 hours) atypical
antipsychotic requires twice daily dosing. It
blocks 5HT1A, 5HT2, D2, α1, α2 and H1
receptors in the brain, but D2 blocking activity is low:
extrapyramidal and hyper-prolactinaemic side effects are minimal. However, it
is quite sedating (sleepiness is a common side effect), and postural
hypotension can occur, especially during dose titration. Urinary retention/
incontinence are reported in few patients. Weight gain and rise in blood sugar
are infrequent. Quetiapine has not been found to benefit negative symptoms of
schizophrenia, but can be used in mania/bipolar disorder. It is metabolized
mainly by CYP3A4; can interact with macrolides, antifungals, anticonvulsants,
etc.
Aripiprazole
This atypical
antipsychotic is unique in being a
partial agonist at D2 and 5HT1A receptor, but antagonist at 5HT2
receptor. It is minimally sedating, may even cause insomnia. Extrapyramidal
side effects, hyperprolactinaemia, hypotension and QT prolongation are not
significant. Little tendency to weight gain and rise in blood sugar has been
noted. Frequent side effects are nausea, dyspepsia, constipation and lightheadedness.
Aripiprazole is quite long-acting
(t½ ~ 3 days); dose adjustments should be done after 2 weeks treatment. It is
metabolized by CYP3A4 as well as CYP2D6; dose needs to be halved in patients
receiving ketoconazole or quinidine, and doubled in those taking carbamazepine.
Aripiprazole is indicated in schizophrenia as well as mania and bipolar
illness.
Ziprasidone
It is the latest
atypical antipsychotic with combined D2 + 5HT2A/2C + H1 +
α1 blocking activity.
Antagonistic action at 5HT1D + agonistic activity at 5HT1A
receptors along with moderately potent inhibition of 5HT and NA reuptake
indicates some anxiolytic and antidepressant property as well. Like other
atypical antipsychotics, ziprasidone has low propensity to cause extrapyramidal
side effects or hyperprolactinaemia. It is mildly sedating, causes modest
hypotension and little weight gain or blood sugar elevation. Nausea and
vomiting are the common side effects. More importantly, a doserelated
prolongation of QT interval occurs. It has the potential to induce serious
cardiac arrhythmias, especially in the presence of predisposing factors/drugs.
The t½ of ziprasidone
is ~8 hours; needs twice daily dosing. In comparative trials, its efficacy in
schizophrenia has been rated equivalent to haloperidol. It is also indicated in
mania.
Adverse Effects
Neuroleptics are very
safe drugs in single or infrequent doses: deaths from overdose are almost
unknown. However, side effects are common.
Based On Pharmacological Actions (Dose Related)
CNS Drowsiness, lethargy, mental confusion: more
with low potency agents; tolerance develops; increased appetite and weight gain
(not with haloperidol); aggravation of seizures in epileptics; even nonepileptics
may develop seizures with high doses of some antipsychotics like clozapine and
olanzapine. However, potent phenothiazines risperidone, quetiapine,
aripiprazole and ziprasidone have little effect on seizure threshold.
CVS Postural hypotension, palpitation,
inhibition of ejaculation (especially with thioridazine) are due to α adrenergic blockade;
more common with low potency phenothiazines. QT prolongation and cardiac
arrhythmias are a risk of overdose with thioridazine, pimozide and ziprasidone.
Anticholinergic Dry mouth, blurring of vision, constipation, urinary hesitancy in
elderly males (thioridazine has the highest propensity); absent in high potency
agents. Some like clozapine induce hypersalivation despite anticholinergic
property, probably due to central action.
Endocrine Hyperprolactinemia
(due to D2 blockade) is common
with typical neuroleptics and risperidone. This can lower Gn levels, but
amenorrhoea, infertility, galactorrhoea and gynaecomastia occur infrequently
after prolonged treatment. The atypical antipsychotics do not appreciably raise
prolactin levels.
Extrapyramidal
Disturbances These are the major dose
limiting side effects; more prominent with high potency drugs like
fluphenazine, haloperidol, pimozide, etc., least with thioridazine, clozapine,
and all other atypical antipsychotics, except high doses of risperidone. These
are of following types.
Parkinsonism with typical
manifestations— rigidity, tremor,
hypokinesia, mask like facies, shuffling gait; appears between 1–4 weeks of
therapy and persists unless dose is reduced. If that is not possible, one of
the anticholinergic antiparkinsonian drugs may be given concurrently. Though
quite effective, routine combination of the anticholinergic from the start of
therapy in all cases is not justified. Levodopa is not effective.
A rare form of extrapyramidal side effect is perioral tremors
‘rabbit syndrome’ that generally occurs after a few years of therapy. It often
responds to central anticholinergic drugs.
Acute Muscular
Dystonias Bizarre muscle spasms, mostly
involving linguofacial muscles —grimacing, tongue thrusting, torticollis,
locked jaw; occurs within a few hours of a single dose or at the most in the
first week of therapy. It is more common in children below 10 years and in
girls, particularly after parenteral administration; overall incidence is 2%. It
lasts for one to few hours and then resolves spontaneously. One of the central
anticholinergics, promethazine or hydroxyzine injected i.m. clears the reaction
within 10–15 min.
Akathisia Restlessness, feeling
of discomfort, apparent agitation manifested as a compelling desire to move
about, but without anxiety, is seen in some patients between 1–8 weeks of
therapy: upto 20% incidence. It may be mistaken for exacerbation of psychosis.
Mechanism of this complication is not understood; no specific antidote is
available. A central anticholinergic may reduce the intensity in some cases;
propranolol is more effective, but most cases require reduction of dose or an
alternative antipsychotic. Addition of diazepam may help.
Malignant Neuroleptic
Syndrome It occurs rarely with high doses
of potent agents; the patient develops marked rigidity, immobility, tremor,
fever, semi-consciousness, fluctuating BP and heart rate; myoglobin may be
present in blood—lasts 5–10 days after drug withdrawal and may be fatal. The
neuroleptic must be stopped promptly and symptomatic treatment given. Though,
antidopaminergic action of the neuroleptic may be involved in the causation of
this syndrome; anticholinergics are of no help. Intravenous dantrolene may
benefit. Bromocriptine in large doses has been found useful.
Tardive Dyskinesia It occurs late in
therapy, sometimes even after
withdrawal of the neuroleptic: manifests as purposeless involuntary facial and
limb movements like constant chewing, pouting, puffing of cheeks, lip licking,
choreoathetoid movements. It is more common in elderly women; probably a
manifestation of progressive neuronal degeneration along with supersensitivity
to DA. It is accentuated by anticholinergics and temporarily suppressed by high
doses of the neuroleptic (this should not be tried except in exceptional
circumstances). An incidence of 10–20% has been reported after long term treatment;
uncommon with clozapine and all other atypical antipsychotics. The dyskinesia
may subside months or years after withdrawal of therapy or may be lifelong.
There is no satisfactory solution of the problem.
Miscellaneous
Weight gain often occurs with long term
antipsychotic therapy; blood sugar and lipids may tend to rise. Risk of
worsening of diabetes is more with clozapine and olanzapine, but minimal with
haloperidol, aripiprazole and ziprasidone. Blue
pigmentation of exposed skin, corneal
and lenticular opacities, retinal
degeneration (more with thioridazine) occur rarely after long-term use of high doses of phenothiazines.
Hypersensitivity Reactions These are not dose related.
Cholestatic
Jaundice with portal
infiltration; 2–4% incidence; occurs
between 2–4 weeks of starting therapy. It calls for withdrawal of the
drug—resolves slowly. More common with low potency phenothiazines; rare with
haloperidol.
Skin rashes,
urticaria, contact dermatitis, photosensitivity (more with CPZ).
Agranulocytosis is rare; more common with clozapine.
Myocarditis Few cases have occurred with clozapine.
Interactions
·
Neuroleptics potentiate all CNS depressants
—hypnotics, anxiolytics, alcohol, opioids, antihistaminics and analgesics.
Overdose symptoms may occur.
·
Neuroleptics block the actions of levodopa and
direct DA agonists in parkinsonism.
·
Antihypertensive action of clonidine and methyldopa
is reduced, probably due to central α2 adrenergic blockade.
·
Phenothiazines and others are poor enzyme
inducers—no significant pharmacokinetic interactions. Enzyme inducers
(barbiturates, anticonvulsants) can reduce blood levels of neuroleptics.
Uses
1. Psychoses
Schizophrenia The antipsychotics are
used primarily in functional psychoses: have indefinable but definite
therapeutic effect in all forms: produce a wide range of symptom relief. They
control positive symptoms (hallucinations, delusions, disorganized thought,
restlessness, insomnia, anxiety, fighting, aggression) better than negative symptoms
(apathy, loss of insight and volition, affective flattening, poverty of speech,
social withdrawal). However, they tend to restore cognitive, affective and
motor disturbances and help upto 90% patients to lead a near normal life in the
society. But, some patients do not respond, and virtually none responds completely.
They are only symptomatic treatment, do not remove the cause of illness; long-term
(even lifelong) treatment may be required. They cause little improvement in
judgement, memory and orientation. Patients with recent onset of illness and
acute exacerbations respond better.
Choice of drug is
largely empirical, guided by the presenting symptoms (it is the target symptoms
which respond rather than the illness as a whole), associated features and mood
state, and on the type of side effect that is more acceptable in a particular
patient. Individual patients differ in their response to different antipsychotics;
there is no way to predict which patient will respond better to which drug. The
following may help drug selection:
·
Agitated, combative and violent—CPZ,
thioridazine, haloperidol, quetiapine.
·
Withdrawn and apathetic—trifluoperazine, fluphenazine,
aripiprazole, ziprasidone.
·
Patient with mainly negative symptoms and
resistant cases—clozapine, olanzapine, risperidone, aripiprazole, ziprasidone
(evidence of their higher efficacy is not firm).
·
Patient with mood elevation, hypomania—
haloperidol, fluphenazine, olanzapine.
·
If extrapyramidal side effects must be avoided
—thioridazine, clozapine or any other atypical antipsychotic.
·
Elderly patients who are more prone to sedation,
mental confusion and hypotension—a high potency phenothiazine, haloperidol,
aripiprazole or ziprasidone.
Currently, the newer atypical antipsychotics are being more
commonly prescribed. Though, there is no convincing evidence of higher
efficacy, they produce fewer side effects and neurological complications. They
are preferable for long-term use in chronic schizophrenia due to lower risk of
tardive dyskinesia. Of the standard neuroleptics, the high potency agents are
preferable over the older low potency ones.
Mania Antipsychotics are required
for rapid control; CPZ or haloperidol
may be given i.m.— act in 1–3 days; lithium or valproate may be started
simultaneously or after the acute phase. After 1–3 weeks when lithium has taken
effect, the neuroleptic may be withdrawn gradually. Recently, oral therapy with
one of the atypical antipsychotics olanzapine/risperidone/aripiprazole/quetiapine
is being preferred for cases not requiring urgent control.
Organic Brain Syndromes Neuroleptics are not very effective. May be used on a short-term
basis—one of the potent drugs is preferred to avoid mental confusion,
hypotension and precipitation of seizures.
The dose of
antipsychotic drugs should be individualized by titration with the symptoms and
kept at minimum. In chronic schizophrenia maximal therapeutic effect is seen
after 2–4 months therapy. However, injected neuroleptics control aggressive symptoms
of acute schizophrenia over hours or a few days. Combination of 2 or more
neuroleptics is not advantageous. However, a patient on maintenance therapy with
a non-sedative drug may be given additional CPZ or haloperidol by i.m.
injection to control exacerbations or violent behaviour.
In a depressed
psychotic, a tricyclic antidepressant may be combined. Benzodiazepines may be
added for brief periods in the beginning.
Low dose maintenance or
intermittent regimens of antipsychotics have been tried in relapsing cases.
Depot injections, e.g. fluphenazine/ haloperidol decanoate given at 2–4 week
intervals are preferable in many cases.
2. Anxiety
Neuroleptics relieve
anxiety but should not be used for
simple anxiety because of autonomic and extrapyramidal side effects:
benzodiazepines are preferable. However, those not responding or having a
psychotic basis for anxiety may be treated with a neuroleptic.
3. As Antiemetic
Neuroleptics are
potent antiemetics—control a
wide range of drug and disease induced vomiting at doses much lower than those
needed in psychosis. However, they should not be given unless the cause of
vomiting has been identified. They are effective in morning sickness but should
not be used for this purpose. They are ineffective in motion sickness: probably
because dopaminergic pathway through the CTZ is not involved in this condition.
4. Other Uses
To
potentiate hypnotics, analgesics and anaesthetics Justified only in
anaesthetic practice.
a)
Intractable hiccough may respond to parenteral
CPZ.
b) Tetanus CPZ is a secondary
drug to achieve skeletal muscle
relaxation.
c)
Alcoholic
hallucinosis, Huntington’s disease and Gilles de la Tourette’s syndrome are rare indications.
Related Topics
