Antidepressant Drugs
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs Used In Mental Illness: Antidepressant And Antianxiety Drugs
These are drugs which can elevate mood in depressive illness. Practically all antidepressants affect monoaminergic transmission in the brain in one way or the other and many of them have other associated properties.
ANTIDEPRESSANT
DRUGS
Classification
I. Reversible Inhibitors of MAOA
(RIMAs)
Moclobemide, Clorgyline
II. Tricyclic Antidepressants
(TCAs)
a.
NA + 5HT reuptake
inhibitors Imipramine,
Amitriptyline, Trimipramine, Doxepin, Dothiepin, Clomipramine
b.
Predominantly NA
reuptake inhibitors Desipramine,
Nortriptyline, Amoxapine, Reboxetine
III. Selective Serotonin Reuptake
Inhibitors (SSRIs)
Fluoxetine, Fluvoxamine,
Paroxetine, Sertraline, Citalopram, Escitalopram
IV. Atypical Antidepressants
Trazodone, Mianserin,
Mirtazapine, Venlafaxine, Duloxetine, Tianeptine, Amineptine, Bupropion
Many other drugs like
Protriptyline, Maprotiline, Nafazodone are marketed in other countries.
MAO INHIBITORS
MAO is a mitochondrial
enzyme involved in the oxidative deamination of biogenic amines (Adr, NA, DA, 5HT).
Two isoenzyme forms of MAO have been identified.
MAO-A: Preferentially
deaminates 5HT and NA, and is inhibited by clorgyline, moclobemide.
MAO-B: Preferentially deaminates phenylethylamine and is
inhibited by selegiline.
Dopamine is degraded equally by both isoenzymes. Their
distribution also differs. Peripheral adrenergic nerve endings, intestinal
mucosa and human placenta contain predominantly MAOA, while MAOB predominates
in certain areas (mainly serotonergic) of brain and in platelets. Liver contains
both isoenzymes. Two hydrazine drugs—isoniazid
and iproniazid were used for
tuberculosis in 1951; the latter was especially found to cause disproportionate
elevation of mood. Its capacity to inhibit degradation of biogenic amines was
soon discovered and was believed to be responsible for the mood elevating action.
Its less hepatotoxic congeners like phenelzine
and isocarboxazid and some
nonhydrazine MAO inhibitors (related to amphetamine) like tranylcypromine were used as antidepressants in the 1960s. They inhibited MAO irreversibly and were
nonselective for the two isoforms. Because of high toxicity and interactions
with foods and other drugs, they have become obsolete.
The selective MAO-A inhibitors possess antidepressant property.
Selegiline selectively inhibits MAO-B at lower doses (5–10 mg/day), but these
are not effective in depression. It is metabolized to amphetamine and at higher
doses it becomes nonselective MAO inhibitor— exhibits antidepressant and
excitant properties.
Nonselective MAO Inhibitors
The nonselective MAO inhibitors elevate the mood of depressed
patients; in some cases it may progress to hypomania and mania. Excitement and
hypomania may be produced even in nondepressed individuals.
The active metabolites of non-selective MAO inhibitors inactivate
the enzyme irreversibly. The drugs themselves stay in the body for relatively
short periods, but their effects last for 2–3 weeks after discontinuation: they
are ‘hit and run’ drugs—return of MAO activity depends on synthesis of fresh enzyme;
tissue monoamine levels remain elevated long after the drug has been largely
eliminated.
Interactions
These drugs inhibit a number of other enzymes as well, and
interact with many food constituents and drugs.
1. Cheese
reaction
Certain varieties of cheese,
beer, wines, pickled meat
and fish, yeast extract contain large quantities of tyramine, dopa, etc. In MAO
inhibited patients these indirectly acting sympathomimetic amines escape
degradation in the intestinal wall and liver → reaching into
systemic circulation they displace large amounts of NA from transmitter loaded
adrenergic nerve endings → hypertensive
crisis, cerebrovascular accidents. When such a reaction occurs, it can be
treated by i.v. injection of a rapidly acting α blocker, e.g.
phentolamine. Prazosin or chlorpromazine are alternatives.
2. Cold
and cough remedies
They contain ephedrine or other sympathomimetics—hypertensive
reaction can occur.
3. Reserpine, guanethidine,
tricyclic antidepressants
Excitement, rise in BP
and body temperature can occur when these drugs are given to a patient on MAO
inhibitors. This is due to their initial NA releasing or uptake blocking
action.
4. Levodopa
Excitement and
hypertension occur due to increase in
biological t½ of DA and NA that are produced from levodopa.
5. Antiparkinsonian
anticholinergics
Hallucinations and symptoms similar to those of atropine
poisoning occur.
6. Barbiturates, alcohol, opioids,
antihistamines
Action of these drugs is intensified and prolonged.
Respiration may fail.
7. Pethidine
High fever, sweating, excitation, delirium, convulsions and severe respiratory depression
have occurred. The most accepted explanation is—MAO inhibitors retard
hydrolysis of pethidine but not its demethylation. Thus, excess of norpethidine (normally a minor metabolite—see p. 459) is produced which has
excitatory actions.
Reversible Inhibitors of MAO-A (RIMAs)
Moclobemide
It is a reversible and
selective MAOA inhibitor with
short duration of action; full MAO activity is restored within 1–2 days of
stopping the drug. Because of competitive enzyme inhibition, tyramine is able
to displace it—potentiation of pressor response to ingested amines is weak,
dietary restrictions are not required. Clinical trials have shown moclobemide
to be an efficacious antidepressant, comparable to TCAs, except in severe
cases. It lacks the anticholinergic, sedative, cognitive, psychomotor and
cardiovascular adverse effects of typical TCAs and is safer in overdose. This
makes it a particularly good option in elderly patients and in those with heart
disease.
Dose: 150 mg BDS–TDS (max
600 mg/day)
RIMAREX 150, 300 mg
tabs.
Adverse effects are
nausea, dizziness, headache, insomnia, rarely excitement and liver damage.
Chances of interaction with other drugs and alcohol are little, but caution is
advised while coprescribing pethidine, SSRIs and TCAs.
Moclobemide has
emerged as a well tolerated alternative to TCAs in mild to moderate depression
and in social phobia.
TRICYCLIC ANTIDEPRESSANTS (TCAS)
Imipramine, an analogue of CPZ was found during clinical trials
(1958) to selectively benefit depressed but not agitated psychotics. In
contrast to CPZ, it inhibited NA and 5HT reuptake into neurones. A large number
of congeners were soon added and are collectively called tricyclic antidepressants (TCAs).
Pharmacological Actions
The most prominent action of TCAs is their ability to inhibit
norepinephrine transporter (NET) and serotonin transporter (SERT) located at
neuronal/platelet membrane at low and therapeutically attained concentrations.
The TCAs inhibit
monoamine reuptake and interact with a variety of receptors viz. muscarinic, α adrenergic, histamine
H1, 5HT1, 5 HT2 and occasionally dopamine D2.
However, relative potencies at these sites differ among different compounds.
The newer selective serotonin reuptake inhibitors (SSRIs) and atypical
antidepressants interact with fewer receptors and have more limited spectrum of
action (produce fewer side effects). The actions of imipramine are described as
prototype.
1. CNS
Effects differ in
normal individuals and the depressed.
In normal individuals It induces a peculiar clumsy feeling, tiredness, light-headedness,
sleepiness, difficulty in concentrating and thinking, unsteady gait. These
effects tend to provoke anxiety. There is no mood elevation or euphoria;
effects are rather unpleasant and may become more so on repeated administration.
In depressed patients Little acute effects
are produced, except
sedation (in the case of drugs which have sedative property). After 2–3 weeks
of continuous treatment, the mood is gradually elevated, patients become more
communicative and start taking interest in self and surroundings. Thus, TCAs
are not euphorients but only antidepressants. In depressed patients who have
preponderance of REM sleep, this phase is suppressed and awakenings during
night are reduced. The EEG effects of low doses are similar to hypnotics but
high doses cause desynchronization. Sedative property varies among different
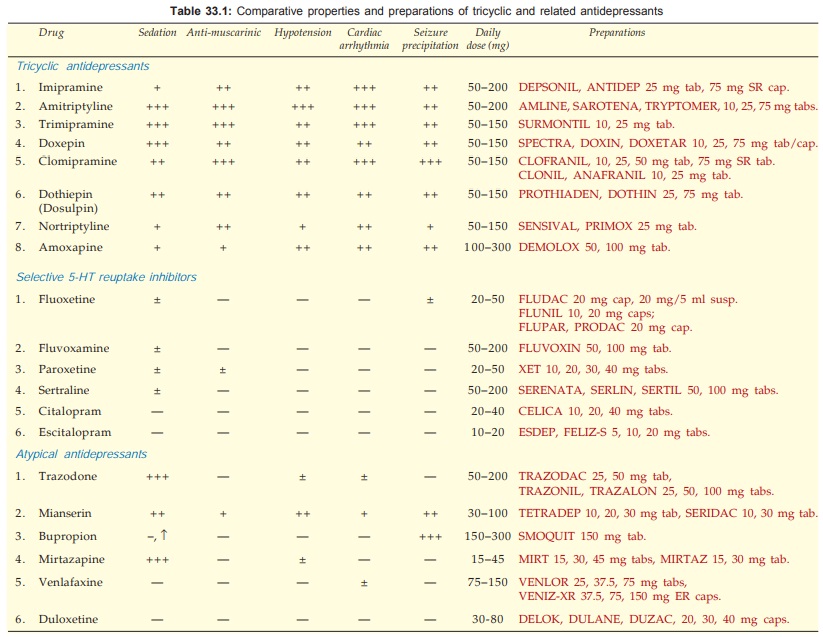
compounds: (see Table 33.1). The more
sedative ones are suitable for depressed patients showing anxiety and
agitation. The less sedative or stimulant ones are better for withdrawn and
retarded patients.
The TCAs lower seizure
threshold and produce convulsions in overdose. Clomipramine, maprotiline and
bupropion have the highest seizure precipitating potential. Amitriptyline and
imipramine depress respiration in overdose only.
Mechanism Of Action
The TCAs and related drugs inhibit active reuptake of biogenic
amines NA and 5HT into their respective neurones and thus potentiate them.
They, however, differ markedly in their selectivity and potency for different amines
(see classification above).
Most of the compounds
do not inhibit DA uptake, except bupropion. Moreover, amphetamine and cocaine
(which are not antidepressants but CNS stimulants) are strong inhibitors of DA
uptake. However, it has been proposed that TCAs indirectly facilitate dopaminergic
transmission in forebrain that may add to the mood elevating action.
Reuptake inhibition
results in increased concentration of the amines in the synaptic cleft in the
CNS and periphery. Tentative conclusions drawn are:
•
Inhibition of DA uptake correlates with stimulant
action; but is not primarily involved in antidepressant action.
•
Inhibition of NA and 5HT uptake is associated
with antidepressant action.
Several findings
indicate that uptake blockade is not directly responsible for antidepressant
action, e.g. uptake blockade occurs quickly but antidepressant action develops after
weeks; mianserin is antidepressant but has no uptake blocking action. Initially
the presynaptic α2 and 5HT1
autoreceptors are activated by the increased amount of NA/5HT in the synaptic
cleft resulting in decreased firing of locus coeruleus (noradrenergic) and
raphe (serotonergic) neurones. However, on long-term administration, antidepressants
desensitise presynaptic α2, 5HT1A, 5HT1D
autoreceptors and induce other adaptive changes in the number and sensitivity of
pre and post synaptic NA and/or 5HT receptors as well as in amine turnover of
brain, the net effect of which is enhanced noradrenergic and serotonergic
transmission. Thus, uptake blockade appears to initiate a series of time-dependent
changes that culminate in antidepressant effect.
Trimipramine is a weak NA/5HT reuptake blocker, but an equally
effective antidepressant. None of these compounds, except amoxapine and to some
extent maprotiline, block DA receptors or possess antipsychotic activity.
2. ANS
Most TCAs are potent
anticholinergics—cause dry mouth, blurring of vision, constipation and urinary
hesitancy as side effect. The anticholinergic potency is graded in Table 33.1
They potentiate exogenous and endogenous NA by blocking uptake,
but also have weak α1 adrenergic blocking
action. Some, e.g. amitriptyline, doxepin, trimipramine have slight H1
antihistaminic action as well.
3. CVS Effects on cardiovascular
function are prominent, occur at
therapeutic concentrations and may be dangerous in overdose.
Tachycardia: due to
anticholinergic and NA potentiating
actions.
Postural Hypotension: due to inhibition of
cardiovascular reflexes and α1 blockade.
ECG Changes And Cardiac Arrhythmias: T wave suppression or
inversion is the most consistent change. Arrhythmias occur in overdose due to
interference with intraventricular conduction, combination of NA potentiating +
ACh blocking actions and direct myocardial depression. Older patients are more
susceptible. The SSRIs and atypical antidepressants are safer in this regard.
Tolerance And Dependence
Tolerance to the
anticholinergic and hypotensive effects of imipramine like drugs develops gradually,
though antidepressant action is sustained.
Psychological
dependence on these drugs is rare, because their acute effects are not
pleasant.
There is some evidence
of physical dependence occurring when high doses are used for long
periods—malaise, chills, muscle pain may occur on discontinuation and have been
considered withdrawal phenomena. Gradual withdrawal is recommended, but
antidepressants do not carry abuse potential.
Pharmacokinetics
The oral absorption of
TCAs is good, though often slow. They are highly bound to plasma and tissue
proteins—have large volumes of distribution (~20 L/kg). They are extensively
metabolized in liver; the major route for imipramine and amitriptyline is
demethylation whereby active metabolites—desipramine and nortriptyline respectively
are formed. Few others also produce active metabolites. Inactivation occurs by
oxidation and glucuronide conjugation. Various CYP isoenzymes like CYP2D6, CYP
3A4, CYP 1A2 and others metabolise tricylic and related anti-depressants. Metabolites
are excreted in urine over 1–2 weeks. The plasma t½ of amitriptyline,
imipramine and doxepin range between 16–24 hours. The t½ is longer for some of
their active metabolites. Because of relatively long t½s, once daily dosing (at
bed time) is practicable in the maintenance phase.
An unusual therapeutic window phenomenon has
been observed, i.e. optimal antidepressant effect is exerted at a narrow band
of plasma concentrations (between 50–200 ng/ml of imipramine, amitriptyline,
nortriptyline). Both below and above this range, beneficial effects are
suboptimal.
Wide variation in the
plasma concentration attained by different individuals given the same dose has
been noted. Thus, doses need to be individualized and titrated, but plasma concentrations
are not a reliable guide for adjusting the dose of TCAs.
Adverse Effects
Side effects are
common
with
tricyclic antidepressants.
• Anticholinergic: dry mouth, bad taste, constipation,
epigastric distress, urinary retention (especially in males with enlarged prostate),
blurred vision, palpitation.
• Sedation, mental confusion and weakness,
especially with amitriptyline and more sedative congeners.
•
Increased appetite and weight gain is noted
with most TCAs and trazodone, but not with SSRIs and bupropion.
• Some patients receiving any antidepressant may
abruptly switch over to a dysphoricagitated state or to mania. Most likely,
these are cases of bipolar depression, the other pole being unmasked by the antidepressant.
Patients receiving higher doses and TCAs are at greater risk than those
receiving lower doses and SSRIs or bupropion.
• Sweating and fine tremors are relatively
common.
• Seizure threshold is lowered—fits may be precipitated,
especially in children. Bupropion, maprotiline, clomipramine, amoxapine have greater
propensity, while desipramine and SSRIs are safer in this regard.
• Postural hypotension, especially in older
patients; less severe with desipramine-like drugs and insignificant with SSRIs.
• Cardiac arrhythmias, especially in patients
with ischaemic heart disease—may be responsible for sudden death in these
patients. Amitriptyline and dosulpin are particularly dangerous in overdose;
higher incidence of arrhythmias is reported.
•
Rashes and jaundice due to hypersensitivity
are rare. Mianserin is more hepatotoxic.
Acute Poisoning
It is frequent;
usually self-attempted by the depressed patients, and may endanger life.
Manifestations are:
Excitement, delirium
and other anticholinergic symptoms as seen in atropine poisoning, followed by
muscle spasms, convulsions and coma. Respiration is depressed, body temperature
may fall, BP is low, tachycardia is prominent. ECG changes and ventricular
arrhythmias are common.
Treatment is primarily supportive
with gastric lavage, respiratory
support, fluid infusion, maintenance of BP and body temperature. Acidosis must
be corrected by bicarbonate infusion.
Diazepam may be
injected i.v. to control convulsions and delirium. Most important is the
treatment of cardiac arrhythmias, for which propranolol/lidocaine may be used; class
IA and IC antiarrhythmics and digoxin prolong cardiac conduction—are
contraindicated.
Physostigmine (0.5–2
mg i.v.) reverses many central and peripheral anticholinergic and sometimes
cardiac effects. However, it is seldom used since arrhythmias are occasionally
worsened and hypotension accentuated by this treatment.
Interactions
·
TCAs potentiate directly acting sympathomimetic amines (in cold/asthma
remedies). Adrenaline containing local
anaesthetic should be avoided. However TCAs attenuate the actions of indirect
sympathomimetics (ephedrine, tyramine).
·
TCAs abolish the antihypertensive action of guanethidine and clonidine by preventing their transport into adrenergic neurones.
· TCAs potentiate CNS depressants, including alcohol and antihistaminics.
· Phenytoin, phenylbutazone,
aspirin and CPZ can displace TCAs from
protein binding sites and cause toxicity.
·
Phenobarbitone induces as well as
competitively inhibits imipramine metabolism.
· Carbamazepine and other enzyme inducers
enhance metabolism of TCAs.
· SSRIs inhibit metabolism of several drugs (see later) including TCAs—dangerous
toxicity can occur if the two are given concurrently.
·
By their anticholinergic property, TCAs delay
gastric emptying and retard their own as well as other drug’s absorption.
However, digoxin and tetracyclines may be more completely
absorbed. When used together, the anticholinergic action of neuroleptics and TCAs
may add up.
·
MAO inhibitors—dangerous
hypertensive crisis with excitement
and hallucinations has occurred when given with TCAs.
Amoxapine
This tetracyclic
compound is unusual in that it
blocks dopamine D2 receptors in addition to inhibiting NA reuptake. It is
chemically related to the antipsychotic drug loxapine and has mixed
antidepressant + neuroleptic properties—offers advantage for patients with
psychotic depression. Risk of extrapyramidal side effects is also there.
Seizures (including status epilepticus) occur in its overdose.
Reboxetine
This is a newer selective NA reuptake blocker with
weak effect on 5HT reuptake. Antimuscarinic and sedative actions are minimal.
It appears to produce fewer side effects and may be safer in overdose than the
older TCAs. Usual side effects are insomnia, dry mouth, constipation, sexual
distress and urinary symptoms.
Dose: 4 mg BD or 8 mg OD.
NAREBOX 4, 8 mg tab.
SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIS)
The major limitations
of conventional TCAs are:
·
Frequent anticholinergic, cardiovascular and
neurological side effects.
·
Relatively low safety margin, hazardous in overdose;
fatalities common.
·
Lag time of 2–4 weeks before antidepressant
action manifests.
·
Significant
number of patients
respond incompletely and some do not respond.
To overcome these
shortcomings, a large number of newer antidepressants have been developed since
1980s. The most significant of these are the SSRIs which selectively inhibit
membrane associated SERT. Though, none of the newer drugs has surpassed older
TCAs in overall efficacy, some patients not responding to one type of drug may
respond to the other. More importantly the newer drugs have improved
tolerability, both in therapeutic use as well as in overdose. It has been
claimed that certain drugs (bupropion, venlafaxine, mirtazapine) have faster
onset of antidepressant action, this has not been unequivocally established.
The relative safety
and better acceptability of SSRIs has made them 1st line drugs in depression
and allowed their extensive use in anxiety, phobias, OCD and related disorders.
The SSRIs produce little or no sedation, do not interfere with cognitive and
psychomotor function or produce anticholinergic side effects. They are devoid
of α adrenergic blocking
action—postural hypotension does not occur—suitable for elderly patients. They
have practically no seizure precipitating propensity and do not inhibit cardiac
conduction—overdose arrhythmias are not a problem. Prominent side effects are
gastrointestinal; all SSRIs frequently produce nausea (due to 5HT3
receptor stimulation), but tolerance develops over time. Weight gain is not a problem
with SSRIs, but they more commonly interfere with ejaculation or orgasm. A new
constellation of mild side effects, viz.
nervousness, restlessness, insomnia, anorexia, dyskinesia, headache and
diarrhoea is associated with them, but patient acceptability is good. Increased
incidence of epistaxis and ecchymosis has been reported, probably due to
impairment of platelet function. Gastric blood loss due to NSAIDs may be
increased by SSRIs.
The SSRIs inhibit drug
metabolizing isoenzymes CYP2D6 and CYP3A4: elevate plasma levels of TCAs,
haloperidol, clozapine, terfenadine, astemizole, warfarin, β blockers, some BZDs
and carbamazepine. ‘Serotonin syndrome’ manifesting as agitation, restlessness,
sweating, twitchings followed by convulsions can be precipitated when any
serotonergic drug is taken by a patient receiving SSRIs. Some degree of
tolerance to antidepressant action of SSRIs has been noted in few patients
after months of use. Discontinuation reaction consisting of paresthesias,
bodyache, bowel upset, agitation and sleep disturbances occurs in some
patients. However, risk of switching over to hypomania during treatment is less
with SSRIs than with TCAs.
The overall
antidepressant efficacy of SSRIs is similar to that of TCAs, though some
patients not responding to one may respond to the other. Because of freedom
from psychomotor and cognitive impairment, SSRIs are preferred for prophylaxis
of recurrent depression.
In severe depression,
however, TCAs appear to be more efficacious. Metaanalysis of comparative trials
has shown no significant difference in efficacy among individual SSRIs, but there
are pharmacokinetic differences and incidence of particular side effects
differs somewhat.
Fluoxetine
A bicyclic compound,
prototype of the SSRIs and the
longest acting; plasma t½ is 2 days and that of its active demethylated
metabolite is 7–10 days. It has been approved for use in children 7 years or
older for depression and OCD on the basis of similar efficacy and side effect
profile as in adults, but should be given to children only when psychotherapy
fails. It has caused more agitation and dermatological reactions than other
SSRIs. Because of slower onset of antidepressant effect, it is considered less
suitable for patients needing rapid effect, but is more appropriate for poorly compliant
patients. Its stimulant effect could worsen patients showing agitation.
Fluvoxamine
It is a shorter-acting
SSRI with a t½ of 18 hours and no
active metabolite.
Relatively more
nausea, agitation and discontinuation reactions have been reported with fluvoxamine.
However, it has been more commonly used in hospitalized patients and in some
anxiety disorders or OCD.
Paroxetine
Another short acting
SSRI (t½ 20 hours) which does not
produce active metabolite. A higher incidence of g.i. side effects and discontinuation
reaction than with other SSRIs has bee noted.
Sertraline
This SSRI has gained
popularity, since in clinical
trials fewer patients stopped sertraline due to side effects. Efficacy in
juvenile depression has been demonstrated. Drug interactions due to inhibition
of CYP isoenzymes are less likely to occur with it. Its plasma t½ is 26 hours
and it produces a longerlasting active metabolite.
Citalopram
This SSRI shares with
sertraline a lower propensity to
cause drug interactions. Its t½ is 33 hours and no active metabolite is known.
However, few deaths due to overdose of citalopram are on record, because of
which it is to be avoided in patients likely to attempt suicide.
Escitalopram
It is the active S(+)
enantiomer of citalopram,
effective at half the dose, with similar properties. Side effects are milder and
safety is improved.
Other Uses of SSRIs
The SSRIs are now 1st choice drugs for OCD, panic disorder, social
phobia, eating disorders, premenstrual dysphoric disorder and post traumatic stress
disorder. They are also being increasingly used for many anxiety disorders,
body dysmorphic disorder, compulsive buying and kleptomania. Elevation of mood
and increased work capacity has been reported in post-myocardial infarction and
other chronic somatic illness patients. Thus, SSRIs are being used to improve
outlook on life and to feel good, even in apparently nondepressed patients.
Wisdom of such use though is questionable.
ATYPICAL ANTIDEPRESSANTS
Trazodone
It is the first
atypical antidepressant; selectively but less efficiently blocks 5HT uptake and
has prominent α blocking as well as
weak 5HT2 antagonistic action. The latter may contribute to its
antidepressant effect. It is sedative but not anticholinergic, causes
bradycardia rather than tachycardia, does not interfere with intracardiac
conduction—less prone to cause arrhythmia—better suited for the elderly. Nausea
is felt, especially in the beginning. Mild anxiolytic effect has been noted and
it has benefited cases of OCD. Inappropriate, prolonged and painful penile
erection (priapism) occurs in few recipients resulting in impotence in a fraction
of these. The α1 adrenergic blocking
property has been held responsible for this effect as well as for postural
hypotension. In general, trazodone is well tolerated and relatively safe in
overdose: seizures donot occur. Its t½ is short (~6 hr).
Mianserin
It is unique in not inhibiting either NA or 5HT
uptake; but blocks presynaptic α2 receptors—increases
release and turnover of NA in brain which may be responsible for antidepressant
effect. Antagonistic action at 5HT2,
5HT1c as well as H1 receptors has also been shown. It is
a sedative—relieves associated anxiety and
suppresses panic attacks. While anticholinergic and cardiac side effects are
less prominent, it has caused seizures in overdose—but fatality is low. Blood
dyscrasias and liver dysfunction have been reported—have restricted its use.
Tianeptine
This antidepressant is
reported to increase rather
than inhibit 5HT uptake, and is neither sedative nor stimulant. It has shown
efficacy in anxio-depressive states, particularly with psychosomatic symptoms,
as well as in endogenous depression. Side effects are dry mouth, epigastric
pain, flatulence, drowsiness/ insomnia, tremor and bodyache.
Dose: 12.5 mg BD–TDS; STABLON 12.5 mg tab.
Amineptine
Like tianeptine it
enhances 5HT uptake, but has
antidepressant property. It produces anticholinergic side effects including
tachycardia, confusion and delirium. Postural hypotension, conduction
disturbances and arrhythmias can occur, especially in patients with heart
disease.
Dose: 100 mg BD at breakfast
and lunCh. No.
SURVECTOR 100 mg tab.
Venlafaxine
A novel antidepressant referred to as ‘serotonin and noradrenaline
reuptake inhibitor’ (SNRI), because it inhibits uptake of both these amines
but, in contrast to older TCAs, does not interact with cholinergic, adrenergic or
histaminergic receptors or have sedative property. Trials have shown it to be
as effective antidepressant as TCAs and may work in some resistant cases. A
faster onset of action has also been indicated. Venlafaxine does not produce
the usual side effects of TCAs; tends to raise rather than depress BP and is
safer in overdose. Prominent side effects are nausea, sweating, anxiety,
dizziness and impotence.
Duloxetine
A newer SNRI similar
to venlafaxine. It is neither sedative, nor anticholinergic, nor antihistaminic,
nor α blocker. Side
effects, including g.i. and sexual problems are milder, but some agitation,
insomnia and rise in BP can occur. Antidepressant efficacy is comparable to
TCAs and duloxetine is also indicated in panic attacks, diabetic neuropathic
pain and stress urinary incontinence in women (because it increases urethral
tone).
Mirtazapine
This antidepressant acts by a novel mechanism, viz. blocks α2 auto (on NA neurones)
and hetero (on 5HT neurones) receptors enhancing both NA and 5HT release. The
augmented NA further increases firing of serotonergic raphe neurones via α1 receptors. Selective
enhancement of antidepressive 5HT1 receptor action is achieved by
concurrent blockade of 5HT2 and 5HT3 receptors which are
held responsible for some of the adverse effects of high serotonergic tone.
Accordingly, it has been labelled as “noradrenergic and specific serotonergic
antidepressant” (NaSSA). It is a H1 blocker and quite sedative, but
not anticholinergic or antidopaminergic. Efficacy in mild as well as severe depression
is reported to be comparable to TCAs and benefit may start earlier.
Bupropion
This inhibitor of DA
and NA uptake has excitant
rather than sedative property. It is metabolized into an amphetamine like
compound. It has been marketed in a sustained release formulation as an aid to
smoking cessation. In clinical trials it has been found to yield higher smoking
abstinence and quitting rates than placebo. Bupropion may be acting by
augmenting the dopaminergic reward function. Better results have been obtained
when it is combined with nicotine patch. The nicotine withdrawal symptoms were
less severe in bupropion recipients. However, long-term efficacy is not known,
and it can cause insomnia, agitation, dry mouth and nausea, but not sexual side
effects. Seizures occur in over dose; the dose of 150 mg BD should not be
exceeded.
Uses
Endogenous (Major) Depression:
The aim is to relieve symptoms of depression and restore
normal social behaviour. The tricyclic and related antidepressants are of proven
value. Response takes at least 2–3 weeks to appear, full benefits take still
longer. Choice of a particular drug for an individual patient depends on the
secondary properties (sedative, anticholinergic, hypotensive, cardiotoxic,
seizure precipitating, etc.) as described above. The SSRIs are currently used
as first choice for their tolerability and safety. The newer atypical agents
also offer some advantages. The only antidepressants clearly shown to be
effective in juvenile depression are fluoxetine and sertraline. The TCAs are
mostly used as alternatives in nonresponsive cases, and are still the most
effective in severely depressed adults. Moclobemide is a better tolerated
option for mild to moderate depression, especially suited for elderly and
cardiac patients. However, antidepressants are not the answer to every grief,
loss, set back and other sad events that are part of life, but the less toxic
and more patient friendly SSRIs/ newer atypical antidepressants are now more
readily prescribed for depressive illness. After a depressive episode has been controlled,
continued treatment at maintenance doses (about 100 mg imipramine/day or equivalent)
for months is recommended to prevent relapse. Therapy is generally not
continued beyond one year. ECT may be given in the severely depressed,
especially initially while the effect of antidepressants is developing, because
no antidepressant has been clearly demonstrated to act fast enough. The TCAs or
SSRIs must be combined with lithium / valproate/ lamotrigine for bipolar depression,
and not used alone due to risk of switching over to mania.
Combination of a SSRI
with an atypical antipsychotic (such as olanzapine for its antimanic property)
is also accepted as a treatment option of bipolar depression.
Obsessive-Compulsive
And Phobic States:
The SSRIs are the
drugs of choice due to better patient acceptability. TCAs, especially clomipramine,
are highly effective in OCD and panic disorders: more than 25% improvement
occurs in OCD rating scale and panic attacks are reduced in >75% patients.
SSRIs and TCAs also reduce compulsive eating in bulimia, and help patients with body
dysmorphic disorder, compulsive buying
and kleptomania, though these
habits may not completely die.
Anxiety Disorders:
Antidepressants,
especially SSRIs, exert a delayed
but sustained beneficial effect in many patients of generalized anxiety disorder;
may be used along with a short course
of BZDs to cover exacerbations. SSRIs have also proven helpful in posttraumatic stress disorder.
Neuropathic
Pain:
Imipramine affords considerable
relief in diabetic and some other types of chronic pain. Amitriptyline reduces
intensity of postherpetic neuralgia in ~50% patients.
Attention Deficit-hyperactivity Disorder In Children:
TCAs with less
depressant properties like imipramine, nortriptyline
and amoxapine are now first line drugs in this disorder, comparable in efficacy
to amphetaminelike drugs, with the advantage of less fluctuating action and
fewer behavioral side effects.
Enuresis:
In children above 5
years, imipramine 25 mg at bedtime is effective, but bed wetting may again
start when the drug is stopped. Eldery subjects with bed wetting have also
benefited.
Migraine:
Amitriptyline has some prophylactic value, especially in
patients with mixed headaches.
Pruritus:
Some tricyclics have antipruritic action. Topical
doxepin has been used to relieve itching in atopic dermatitis, lichen simplex,
etc.
NOCTADERM 5%
cream.
Related Topics
