Antiviral chemotherapy- Control of Viruses
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Viruses
Antivirals can act at different stages of the viral replication cycle, with the most effective treatments targeting unique viral enzymes, such as proteases, polymerases and the reverse transcriptase .
CONTROL OF VIRUSES
ANTIVIRAL CHEMOTHERAPY
A number of antivirals
are in use in the UK ( British National Formulary, 2009) for a range of
viral infections, including HIV, herpesvirus
infections, viral hepatitis, influenza and respiratory syncytial virus.
Antiviral treatments are particularly important for persons at high risk,
notably immunocompromised patients. Most antivirals are prodrugs that need to
be activated within the cell, usually by a kinase, and other cellular enzymes.
Antivirals can act at
different stages of the viral replication cycle, with the most effective
treatments targeting unique viral enzymes, such as proteases, polymerases and
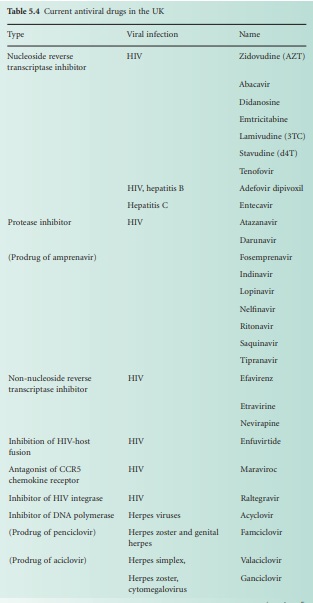
the reverse transcriptase (Table 5.4). A number of targets are being
investigated to prevent viral attachment to the host cell: competition for CD4
receptors using a pentapeptide identical in sequence to the terminal amino
acids of HIV gp120; inhibition of herpes simplex virus (HSV) ribonucleotide
reductase; competition for the cell receptor using a hexapeptide fusion
sequence at the N terminus of the influenza haemagglutinin viral receptor.
Proteases are particularly important for the uncoating process preventing the release
of viral nucleocapsid and for the cleavage of viral polypeptide gene products
(e.g. indinavir sulphate). The replication of viral DNA is also a wellexploited
target with the use of nucleoside analogues (e.g. idoxiuridine is incorporated
into viral and cellular DNA instead of thymidine), nonnucleoside analogues
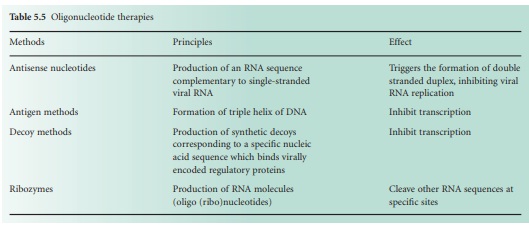
(e.g. nevirapine and foscarnet) and oligonucleotides (Table 5.5). These nucleic
acid oligomers with base sequence complementary to conserved regions of
proviral DNA have been successful use in the prevention of viral mRNA function.
The inhibition of HIV reverse transcriptase has led to the synthesis of many
successful antivirals (Table 5.4). The release of the mature virions after the
multiplication process can also be blocked. This is the case of neuraminidase
inhibitors (e.g. zanamivir and ozaltamivir) preventing the shedding of virions.
Unfortunately, antiviral
chemotherapy is associated with a number of problems. Many viral diseases only
become apparent after extensive viral multiplication and tissue damage have
occurred, delaying treatments. Many antivirals are toxic (e.g. nucleoside
analogues) since viral replication often depends on the use of host cell
enzymes. There is also scope for improving the pharmacokinetic properties of
antivirals, providing a better penetration and retarding drug degradation. The
use of prodrugs has improved drug adsorption. Finally, antiviral monotherapy
often leads to the development of virus resistance. Emerging HIV resistance has
been well documented and current treatments are based on a triple therapy.
HIV
There is no cure for HIV
infections as yet. The role of antivirals is to slow or halt disease
progression. Since their discovery and use, these drugs (Table 5.4), called antiretrovirals,
have considerably prolonged the life expectancy of patients, although not
without some important side effects. Antiretroviral treatments aim to reduce
HIV plasma levels for as much and as long as possible. Several antiretroviral
drugs are usually given together to avoid emerging viral resistance. Initiation
of HIV treatment (HAART) is therefore complex and involves two nucleoside
reverse transcriptase inhibitors and two nonnucleoside reverse transcriptase
inhibitors. Alternative regimens are possible following treatment failure and
deterioration of a patient’s condition. The use of antiretrovirals for
prophylaxis after exposure is also possible, where a patient has been exposed
to HIVcontaminated materials (e.g. needle injury). Such use follows guidelines
available locally (e.g. hospital) or nationally (e.g. Department of Health,
British Association for Sexual Health and HIV).
The immune
reconstitution syndrome and the lipodystrophy syndrome have been associated with
antiretroviral treatments. The latter includes fat redistribution, insulin resistance,
hyperglycaemia and dyslipidaemia. In addition, these antivirals can be damaging
to liver function and have been associated with osteonecrosis following longterm
combination treatments. A number of side effects are commonly associated with
the use of antiretrovirals: gastrointestinal disturbance, anorexia, pancreatitis,
liver damage, dyspnoea, cough, headache, insomnia, dizziness, fatigue, blood
disorders, myalgia, arthralgia, rash, urticaria and fever. Protease inhibitors
are metabolized by cytochrome P450 and therefore have a significant potential
for drug interactions. Nonnucleoside reverse transcriptase inhibitors have been
shown to interact with a number of drugs metabolized in the liver. They have
been associated with a number of side effects such as rash, psychiatric and
central nervous system disturbances, and even fatal hepatitis.
Herpesvirus infections
Herpesviridae is a
family of viruses that include the herpes simplex virus, chickenpox
(varicella), shingles (herpes zoster) and cytomegalovirus. Mild herpes simplex
virus infections in healthy individuals are treated with a topical antiviral
drug (e.g. treatment of cold sores). However, for primary herpetic
gingivostomatitis a change of diet and analgesics are recommended. For severe
infections (e.g. neonatal herpes infection, infection in immunocompromised
patients) a systemic antiviral drug is used (Table 5.4). Antiviral treatments
for chickenpox are recommended in patients at risk and in neonates to reduce
risks of severe diseases. In healthy adults, treatment taken with 24 hours of
the appearance of a rash may decrease the duration and severity of symptoms.
Systemic antivirals are used to decrease the severity and duration of shingles
when taken within 72 hours of the onset of rash. Antivirals for herpes are also
associated with a number of side effects which vary depending on the drug, but
may include nausea, vomiting, stomach pain, headache, fatigue, rash, and
increase in serum and urine uric acid. Antivirals for the treatment of
cytomegalovirus are usually given to immunocompromised patients and they tend
to be more toxic with notable nephrotoxicity (e.g. cidofovir) and a number of
documented side effects (e.g. ganciclovir, foscarnet)
Viral hepatitis
Hepatitis B and C are
major causes of viral chronic hepatitis. The initial treatment for acute
hepatitis B is with interferons (peginterferon alfa 2a) which may reduce the
risk of chronic infection. However, the use of interferon is limited by a poor
response rate in patients and frequent relapse. A number of antivirals are
licensed for the treatment of chronic hepatitis B (Table 5.4). The choice of
antivirals depends upon the initial response to peginterferon alfa, emerging
viral resistance, and co infection with
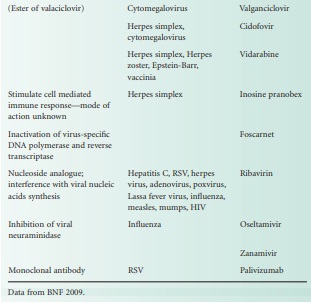
HIV. For the treatment of chronic hepatitis C, a combination of ribavarin and
peginterferonalfa is recommended, although the choice and duration of treatment
depends upon the viral genotypes and viral load. These antivirals are also
associated with a number of side effects including nausea, vomiting, abdominal
pain and diarrhoea.
Influenza
Two antivirals are
recommended for the treatment of influenza according to the National Institute
of Health and Clinical Excellence (NICE) guidelines (Table 5.4). Oseltamivir
was extensively used for the prevention and control of the swine flu outbreak
in the UK in 2009. Following an intensive use, at least two major limitations
in the usefulness of the drug have been identified. First, the drug needs to be
taken within a few hours of the onset of symptoms, which proved very difficult
with a number of symptoms from mild ‘cold-like’ to severe ‘flulike’ symptoms
reported. Second, the side effects, especially in young children and
adolescents, have been very severe, prompting many parents to stop the
medication, decreasing the willingness to give the antivirals to children who
have been possibly exposed to the virus.
Respiratory syncytial virus
Respiratory syncytial
virus (RSV) is responsible for severe bronchiolitis notably in infants. A
monoclonal antibody (palivizumab) or an antiviral drug (ribavirin) is indicated
for the treatment of RSV (Table 5.4). The antiviral is associated with a number
of severe side effects.
Related Topics
