Drugs for Cough
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs for Cough and Bronchial Asthma
Cough is a protective reflex, its purpose being expulsion of respiratory secretions or foreign particless from air passages. It occurs due to stimulation of mechano or chemoreceptors in throat, respiratory passages or stretch receptors in the lungs.
DRUGS FOR COUGH
Cough is a protective
reflex, its purpose being expulsion of respiratory secretions or foreign particless
from air passages. It occurs due to stimulation of mechano or chemoreceptors in
throat, respiratory passages or stretch receptors in the lungs. Cough may be
useful or useless. Useless (nonproductive) cough should be suppressed. Useful
(productive) cough serves to drain the airway, its suppression is not
desirable, may even be harmful, except if the amount of expectoration achieved is
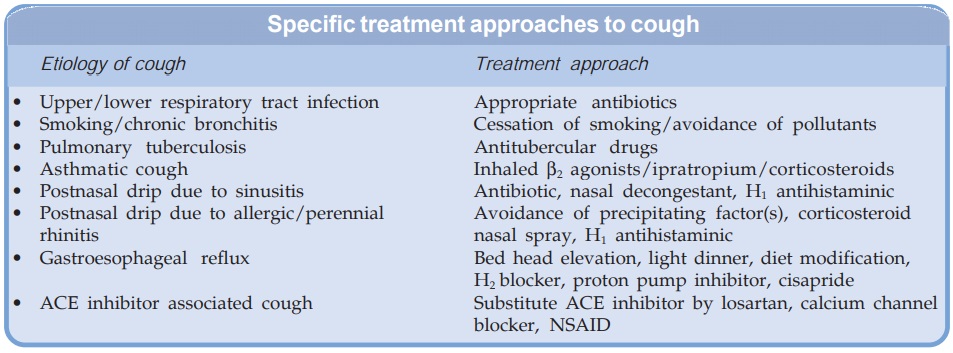
small compared to the effort of continuous coughing. Apart from specific
remedies (antibiotics, etc. see box),
cough may be treated as a symptom (nonspecific therapy) with:
1. Pharyngeal Demulcents
Lozenges, cough
drops, linctuses containing
syrup, glycerine, liquorice.
2. Expectorants (Mucokinetics)
a. Bronchial secretion enhancers
Sodium or Potassium
citrate, Potassium iodide, Guaiphenesin (Glyceryl guaiacolate), balsum of Tolu,
Vasaka, Ammonium chloride.
b.
Mucolytics
Bromhexine, Ambroxol,
Acetyl cysteine, Carbocisteine
3. Antitussives (Cough centre
suppressants)
a.
Opioids Codeine, Pholcodeine.
b.
Nonopioids Noscapine,
Dextromethorphan, Chlophedianol.
c. Antihistamines Chlorpheniramine,
Diphenhydramine, Promethazine.
4.
Adjuvant Antitussives
Bronchodilators Salbutamol,
Terbutalin.
Demulcents And Expectorants
Pharyngeal demulcents
sooth the throat and reduce afferent impulses from the inflamed/ irritated
pharyngeal mucosa, thus provide symptomatic relief in dry cough arising from
throat.
Expectorants
(Mucokinetics) are drugs believed to increase bronchial secretion or reduce its
viscosity, facilitating its removal by coughing.
Sodium and potassium
citrate are considered to increase bronchial secretion by salt action. Potassium
iodide is secreted by bronchial glands and can irritate the airway mucosa.
Prolonged use can affect thyroid function and produce iodism. It is rarely used
now. Guaiphenesin, vasaka, tolu balsum are plant products which are supposed to
enhance bronchial secretion and mucociliary function while being secreted by
tracheobronchial glands. Ammonium salts are nauseating—reflexly increase
respiratory secretions. A variety of expectorant formulations containing an
assortment of the above ingredients, often in combination with
antitussives/antihistaminics are marketed and briskly promoted, but objective
evidence of efficacy of these is nonconclusive.
Mucolytics
Bromhexine
A derivative of the alkaloid vasicine obtained from Adhatoda vasica (Vasaka), is a potent mucolytic and mucokinetic,
capable of inducing thin copious bronchial secretion. It depolymerises
mucopolysaccharides directly as well as by liberating lysosomal enzymes—
network of fibres in tenacious sputum is broken. It is particularly useful if mucus
plugs are present. Side effects are
rhinorrhoea and lacrimation, gastric
irritation, hypersensitivity.
Dose: adults 8 mg TDS, children 1–5 years 4 mg BD,
5–10 years 4 mg TDS.
BROMHEXINE 8 mg tablet,
4 mg/5 ml elixir.
Ambroxol A metabolite of bromhexine
having similar mucolytic
action, uses and side effects.
Dose:
15–30 mg TDS.
AMBRIL, AMBROLITE, AMBRODIL, MUCOLITE 30 mg
tab, 30 mg/5 ml liquid, 7.5 mg/ml drops.
Acetylcysteine
It opens disulfide bonds in mucoproteins present in sputum—makes it less viscid, but
has to be administered directly into the respiratory tract.
MUCOMIX 200 mg/ml inj in 1,2,5 ml amps; injectable solution may be
nebulized/instilled through trachiostomy tube.
Carbocisteine
It liquefies viscid sputum in the same way as acetylcysteine
and is administered orally (250–750 mg TDS). Some patients of chronic
bronchitis have been shown to benefit. Side effects are g.i. irritation and
rashes.
MUCODYNE 375 mg cap,
250 mg/5 ml syr.
It is available in
combination with amoxicillin or cephalexin for treatment of bronchitis,
bronchiectasis, sinusitis, etc.
CARBOMOX:
Carbocisteine 150 mg + amoxicillin 250 or 500 mg caps. CARBICEF: Carbocisteine
150 mg + cephalexin 250 or 500 mg caps.
Antitussives
These are drugs that act
in the CNS to raise the threshold of cough centre or act peripherally in the
respiratory tract to reduce tussal impulses, or both these actions. Because
they aim to control rather than eliminate cough, antitussives should be used only
for dry unproductive cough or if cough is unduly tiring, disturbs sleep or is
hazardous (hernia, piles, cardiac disease, ocular surgery).
Opioids
Codeine (see Ch. No. 34) An opium alkaloid, qualitatively
similar to but less potent than morphine. It is more selective for cough centre
and is treated as the standard antitussive; suppresses cough for about 6 hours.
The antitussive action is blocked by naloxone indicating that it is exerted
through opioid receptors in the brain. Abuse liability is low, but present;
constipation is the chief draw back. At higher doses respiratory depression and
drowsiness can occur—driving may be impaired. Like morphine, it is
contraindicated in asthmatics and in patients with diminished respiratory
reserve.
Dose: 10–30 mg; children 2–6
years 2.5–5 mg, 6–12 years 5–10 mg,
frequently used as syrup codeine phos. 4–8 ml.
CODINE
15 mg tab, 15 mg/5 ml linctus.
Pholcodeine It has practically no analgesic or addicting property, but is similar in efficacy as
antitussive to codeine and is longer acting—acts for 12 hours; dose: 10–15 mg. (ETHNINE 5 mg/5 ml
syr).
Non-Opioids
Noscapine (Narcotine) An opium alkaloid of
the benzoisoquinoline
series (see Ch. No. 34). It depresses
cough but has no narcotic, analgesic or dependence inducing properties. It is
nearly equipotent antitussive as codeine, especially useful in spasmodic cough.
Headache and nausea occur occasionally as side effect. It can release histamine
and produce bronchoconstriction in asthmatics.
Dose: 15–30 mg, children 2–6
years 7.5 mg, 6–12 years 15 mg.
COSCOPIN 7 mg/5 ml
syrup, COSCOTABS 25 mg tab.
Dextromethorphan A synthetic compound;
the disomer has selective
antitussive action (raises threshold
of cough centre) while lisomer is
analgesic. Dextromethorphan is as effective as codeine, does not depress
mucociliary function of the airway mucosa and is practically devoid of
constipating and addicting actions. The antitussive action lasts for ~ 6 hours
and is not blocked by naloxone: therefore not exerted through opioid receptors.
Side effect: Dizziness, nausea,
drowsiness, ataxia.
Dose: 10–20 mg, children 2–6
years 2.5–5 mg, 6–12 years 5–10 mg.
Chlophedianol It is a centrally acting
antitussive with slow onset and
longer duration of action. Side effect:
Dryness of mouth, vertigo, irritability.
Dose: 20–40 mg; DETIGON, TUSSIGON 20
mg/5 ml linctus with Ammon. chloride
50 mg and menthol 0.25 mg.
Antihistamines
Many H1
antihistamines have been conventionally added to antitussive/expectorant formulations
(see below). They afford relief in
cough due to their sedative and anticholinergic actions, but lack selectivity
for the cough centre. They have no expectorant property, may even reduce
secretions by anticholinergic action. They have been specially promoted for cough
in respiratory allergic states, though their lack of efficacy in asthma is
legendary.
Chlorpheniramine (2–5
mg), Diphenhydramine (15–25 mg) and Promethazine (15–25 mg; PHENERGAN 5 mg/5 ml
elixir) are commonly used. Second generation antihistamines like fexofenadine,
loratadine are ineffective.
Bronchodilators Bronchospasm can
induce or aggravate cough.
Stimulation of pulmonary receptors can trigger both cough and bronchoconstriction,
especially in individuals with bronchial hyperreactivity. Bronchodilators
relieve cough in such individuals and improve the effectiveness of cough in
clearing secretions by increasing surface velocity of airflow during cough.
They should be used only when an element of bronchoconstriction is present and
not routinely. Their fixed dose combinations with antitussives are not satisfactory
because of differences in time course of action of the components and liability
for indiscriminate use.
Fixed dose
combinations of a centrally acting antitussive with a bronchodilator or with an
antihistaminic having high atropinic activity have been banned in India, but
many are still marketed.
Aeromatic chest rub is widely advertized
as a cough remedy. Though it has
been shown to reduce experimentally induced cough in healthy volunteers, there
is no evidence of benefit in pathological cough.
Related Topics
