Antiamoebic Drugs
| Home | | Pharmacology |Chapter: Essential pharmacology : Antiamoebic And Other Antiprotozoal Drugs
These are drugs useful in infection caused by the protozoa Entamoeba histolytica.
ANTIAMOEBIC DRUGS
These are drugs useful
in infection caused by the protozoa Entamoeba
histolytica.
Amoebiasis has a
worldwide distribution (over 40 million people are infected), but it is endemic
in most parts of India and other developing countries. Poor environmental
sanitation and low socioeconomic status are important factors in the spread of
the disease, which occurs by faecal contamination of food and water. Amoebic
cysts reaching the intestine transform into trophozoites which either live on
the surface of colonic mucosa as commensals— form cysts that pass into the
stools (luminal cycle) and serve to propagate the disease, or invade the
mucosa—form amoebic ulcers (Fig. 60.1) and cause acute dysentery (with blood
and mucus in stools) or chronic intestinal amoebiasis (with vague abdominal
symptoms, amoeboma).
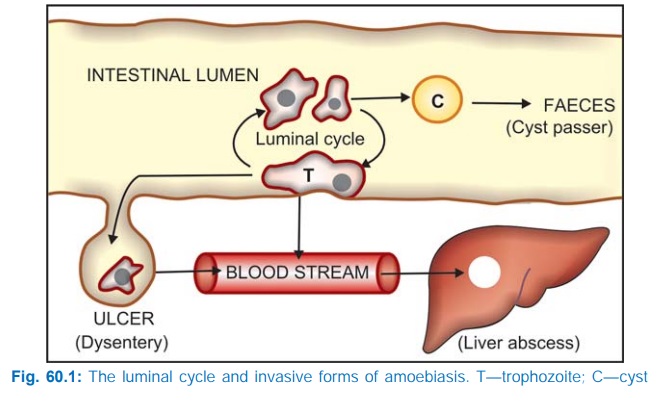
Occasionally the
trophozoites pass into the blood stream, reach the liver via portal vein and cause amoebic liver abscess. Other organs like
lung, spleen, kidney and brain are rarely involved in extraintestinal
amoebiasis. In the tissues, only trophozoites are present; cyst formation does
not occur. Tissue phase is always secondary to intestinal amoebiasis, which may
be asymptomatic. In fact, most chronic cyst passers are asymptomatic. In the
colonic lumen, the Entamoebae live in
symbiotic relationship with bacteria, and a reduction in colonic bacteria
reduces the amoebic population.
The ‘Brazil root’ or Cephaelis ipecacuanha was used for the
treatment of dysentery in the 17th century. The pure alkaloid emetine obtained
from it was found to be a potent antiamoebic in 1912 and remained the most efficacious
and commonly used drug till 1960. Many 8hydroxyquinolines (quiniodochlor, etc.)
became very popular drugs for diarrhoeas and amoebic dysentery, but have come
under a cloud since they were held responsible for causing epidemics of SMON in
Japan in 1970. Soon after its triumph as an antimalarial in 1948, chloroquine
was found to be an effective and safe drug for hepatic amoebiasis. Diloxanide
furoate was a useful addition in 1960, covering mainly chronic intestinal form
of the disease. However, the most remarkable development was the demonstration
of antiamoebic property of metronidazole in the early 1960s. This drug had been
introduced a few years back as a well tolerated, orally effective agent for
trichomonas vaginitis. Of the many congeners of metronidazole that were tested,
tinidazole has emerged in the 1970s as a good alternative, and others have been
added subsequently.
CLASSIFICATION
1. Tissue Amoebicides
a) For both intestinal and extraintestinal amoebiasis:
Nitroimidazoles: Metronidazole, Tinidazole, Secnidazole, Ornidazole,
Satranidazole
Alkaloids: Emetine,
Dehydroemetine
b) For extraintestinal amoebiasis
only: Chloroquine
2. Luminal
Amoebicides
a)
Amide : Diloxanide furoate,
Nitazoxanide
b) 8-Hydroxyquinolines: Quiniodochlor (Iodochlorohydroxyquin, Clioquinol), Diiodohydroxyquin
(Iodoquinol)
c)
Antibiotics: Tetracyclines
