Clinical governance
| Home | | Hospital pharmacy |Chapter: Hospital pharmacy : Pharmacist prescribing
‘A framework through which NHS organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care by creating an environment.
Clinical governance
‘A framework through
which NHS organisations are accountable for continuously improving the quality
of their services and safeguarding high standards of care by creating an
environment in which excellence in clinical care will flourish’ is how clinical
governance was defined by the Department of Health. It can be argued that
non-medical prescribing sits easily with this approach, as it uses
appropriately trained individuals to provide excellent care and it helps to
improve patient services. Non-medical prescribing is based firmly on a
foundation of competence; prescribers are required by their regis-tering body
to maintain their competence within their area of expertise and their
competence to prescribe.
·
Pharmacists are instructed by the Code of Ethics:
·
At all stages of your professional working life you must
ensure that your knowledge, skills and performance are of a high quality, up to
date and relevant to your field of practice.
Although independent
prescribers have the ability to prescribe any item from the entire British
National Formulary, it is embedded in non-medical pre-scribing education that
practitioners must have a full knowledge of the medi-cine they prescribe and
the disease they are treating. In practice, pharmacist prescribers work to a
personal formulary based around their area of practice. A further fundamental
part of any pharmacist prescriber’s practice must be the participation in
continuing professional development and reflection upon how new learning
influences prescribing practice. Discussion groups have been set up for
prescribing pharmacists to allow them access to other pre-scribers for advice
and support.
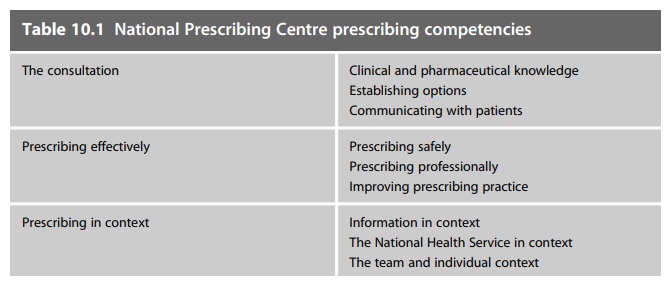
The National
Prescribing Centre has developed a competency framework to aid pharmacist
prescribers, those who commission their services and pro-vide governance. The
framework is divided into three main areas: (1) the consultation; (2)
prescribing effectively; and (3) prescribing in context. The areas of
competency are set out in Table 10.1. The framework can be used by individuals
to inform their continuing professional development or by an organisation to
ensure quality.
It is incumbent on
individual prescribers to apply clinical governance principles to their
practice; however, the organisation within which they conduct that practice
also has a duty of care to both the patient and the prescriber.21
Organisations have established non-medical prescribing com-mittees to provide a
governance framework for prescribers to work within. Committees vary in their
practice. However they:
·
keep a register of non-medical prescribers operating within
their organisation
·
ensure that the relevant organisational policies include and
incorporate non-medical prescribing
·
agree and approve clinical management plans and personal
formularies.
They also have a
role in agreeing which staff groups and individuals will be supported by the
organisation to train as non-medical prescribers. With the involvement of the
organisation in the selection of candidates for training it is hoped that
prescribers will utilise those skills once gained, as their position in the
service will already be established.
Within the clinical governance arena we have seen the emergence of quality being allied to waste reduction within patient services. Pharmacist prescribers are using their knowledge of medicines regimens and their expertise in individualising patients’ medicines to reduce medication errors within healthcare and this can only improve the quality of care offered to those patients.
