Composition of Oral Rehydration Solution
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs For Constipation And Diarrhoea
Oral rehydration is possible if glucose is added with salt. It capitalizes on the intactness of glucose coupled Na+ absorption, even when other mechanisms have failed or when intestinal secretion is excessive—the secreted fluid lacks glucose and cannot be reabsorbed.
ORAL REHYDRATION SOLUTION
In majority of cases, this is the only measure needed. Rehydration can be done orally or i.v.
Intravenous Rehydration
It is needed only when fluid loss is severe i.e., > 10% body weight, (if not promptly corrected, it will lead to shock and death) or if patient is losing > 10 ml/kg/hr, or is unable to take enough oral fluids due to weakness, stupor or vomiting. The recommended composition of i.v. fluid (Dhaka fluid) is:
NaCl 85 mM = 5 g
KCl 13 mM = 1 g
NaHCO3 48 mM = 4 g
in 1 L of water or 5% glucose solution.
This provides 133 mM Na+, 13 mM K+, 98 mM Cl¯ and 48 mM HCO3 ¯. Ringer lactate (Na+ 130, Cl¯ 109, K+ 4, lactate 28 mM) recommended by WHO (1991) could be used alternatively.
Volume equivalent to 10% BW should be infused over 2–4 hours; the subsequent rate of infusion is matched with the rate of fluid loss. In most cases, oral rehydration can be instituted after the initial volume replacement.
Oral Rehydration
Advent of oral rehydration therapy (ORT) is considered a major advance of recent times. If the fluid loss is mild (5–7% BW) or moderate (7.5–10% BW) ORT can be instituted from the very beginning.
Rationale Of ORS Composition
Oral rehydration is possible if glucose is added with salt. It capitalizes on the intactness of glucose coupled Na+ absorption, even when other mechanisms have failed or when intestinal secretion is excessive—the secreted fluid lacks glucose and cannot be reabsorbed. The composition of oral rehydration salt/solution (ORS) has been debated. The general principles are:
a) It should be isotonic or somewhat hypotonic, i.e. total osmolarity 200–310 mOsm/L (diarrhoea fluids are approximately isotonic with plasma).
b) The molar ratio of glucose should be equal to or somewhat higher than Na+ (excess glucose will be utilized in absorbing Na+ present in the intestinal secretions in addition to that present in ORS itself), but not exceed 110 mM.
c) Enough K+ (15–25 mM) and bicarbonate/ citrate (8–12 mM) should be provided to make up the losses in stool.
The WHO recommended a standard formula which provided Na+ 90 mM, K+ 20 mM, Cl¯ 80 mM, citrate (base) 10 mM, glucose 110 mM and had a total osmolarity of 310 mOsm/L. Trisod. citrate was included in place of sod. bicarbonate because bicarbonate containing powder caked and developed a brown colour due to formation of furfural compounds with glucose: had a short shelf life.
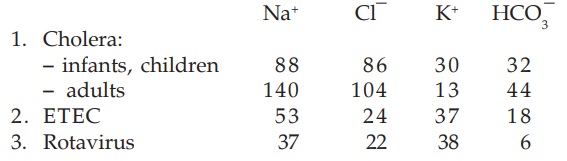
It has been argued that the composition of ORS should be varied according to that of the diarrhea stool. The average electrolyte composition (mM) of 3 important infective diarrhea stools is:
As can be seen, the standard WHOORS is based on the composition of cholera stools, particularly in children. When used in noncholera diarrhoea, this WHOORS occasionally produces periorbital edema due to excess Na+ absorption. Based also on the Na+ content of ETEC stools, many pediatricians have favoured 60 mM Na+ and 90 mM glucose ORS for noncholera diarrhoeas.
New Formula WHO-ORS
In 2002 a new formula low Na+ low glucose ORS has been released by the WHO. Over the past 20 years WHO sponsored studies were carried out in several developing countries among children and adults suffering from diarrhoeas. It was found that maximum water absorption occurs from a slightly hypotonic solution and when glucose concentration is between 60–110 mM. At higher concentrations, glucose appears in the stools and takes its osmotic penalty—stool volume is increased. Recent studies showed that efficacy of ORS in children with acute noncholera diarrhoea is improved by reducing Na+ and glucose concentration to 75 mM, and total osmolarity to 245 mOsm/L. The need for supplemental i.v. therapy was reduced by 33%. A combined analysis of studies with low osmolarity ORS has revealed that stool volume is reduced by 20% and incidence of vomiting by 30%. The new formula ORS has proven as effective and as safe in cholera as well, both in children and in adults, but there is some risk of hyponatremia in adults with cholera.
The WHO and UNICEF have recommended replacement of standard (310 mOsm/L) ORS formula by the new (245 mOsm/L).
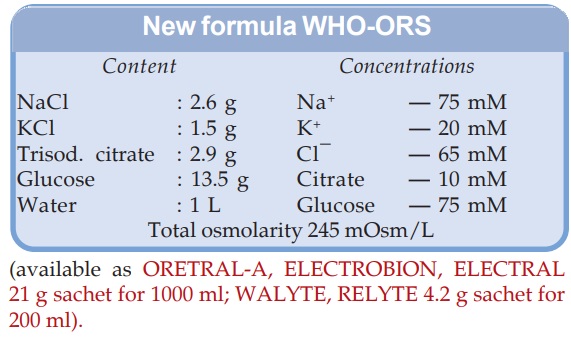
(available as ORETRALA, ELECTROBION, ELECTRAL 21 g sachet for 1000 ml; WALYTE, RELYTE 4.2 g sachet for 200 ml).
Potassium is an important constituent of ORS, since in most acute diarrhoeas K+ loss is substantial. The base (bicarbonate, citrate, lactate) is added to correct acidosis due to alkali loss in stools. It may independently promote Na+ and water absorption. However, relying on the ability of the kidney to restore acidbase balance, acidotic states have been managed without an exogenous base. Base free ORS has been found to be equally effective in rehydrating, though correction of acidosis is slower. Thus, there is a trend to consider base as a nonessential constituent of ORS, but if present it may be beneficial, especially in severe cases with overt acidosis.
Administration Of ORT
Patients are encouraged to drink ORS at ½–1 hourly intervals, initially 5–7.5% BW volume equivalent is given in 2–4 hours (5 ml/kg/hr in children). Thirst due to volume depletion provides an adequate driving force. Subsequently it may be left to demand, but should at least cover the rate of loss in stools. In a weak child who refuses to drink ORS at the desired rate—it can be given by intragastric drip; restoring hydration in 6 hours should be aimed.
ORT is not designed to stop diarrhoea, but to restore and maintain hydration, electrolyte and pH balance until diarrhoea ceases, mostly spontaneously. It is the best and not a second choice approach to i.v. hydration. About 300 million litre of ORS is being used annually, and is estimated to be preventing 0.5 million child deaths worldwide.
Non-diarrhoeal Uses Of ORT
a) Postsurgical, postburn and posttrauma maintenance of hydration and nutrition (in place of i.v. infusion).
b) Heat stroke.
c) During changeover from parenteral to enteral elimentation.
Super ORS
This is a solution which in addition to rehydrating may lead to decrease in purging rates and improvement in diarrhoea by enhanced absorption. Improvement in ORS by adding certain actively transported amino acids (alanine, glycine which cotransport Na+) has been tried. Their efficacy is marginal, and not extended to noncholera diarrhoea; cost-effectiveness may not be favourable. There is compelling evidence, however, that a complex substrate like boiled rice powder 40–50 g/L is an efficient substitute for glucose. The rice starch is slowly hydrolysed at the brush border or in the lumen into glucose which is absorbed: does not cause osmotic diarrhoea even when larger quantity is added: more calories can be administered. Rice has 7% protein: yields amino acids which may themselves stimulate salt and water absorption. It has been found to reduce stool volume compared to WHOORS in cholera patients. Moreover, rice is cheap and widely available. Thus, rice (or wheat, maize, potato) based ORS appears to be suitable for developing countries.
Related Topics
