Treatment Of Diarrhoeas
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs For Constipation And Diarrhoea
Diarrhoea is too frequent, often too precipitate passage of poorly formed stools. In pathological terms, it occurs due to passage of excess water in faeces.
TREATMENT OF DIARRHOEAS
Diarrhoea is too frequent, often too precipitate passage of
poorly formed stools. In pathological terms, it occurs due to passage of excess
water in faeces.
Diarrhoeal diseases constitute a major cause of morbidity and
mortality worldwide; especially in developing countries. More than 5 million
children under the age of 5 years die every year due to diarrhoea. A nationwide
study has estimated that diarrhoea kills > 1 million children in India
annually. Recurrent or protracted diarrhoea is also a major cause of proteincalorie
malnutrition in developing countries. Even mild diarrhoea, and that in adults,
is a disabling symptom and an inconvenience.
Relevant Pathophysiology
Water and electrolytes
are absorbed as well as secreted in the intestine. Jejunum is freely permeable
to salt and water which are passively absorbed secondary to nutrient (glucose,
amino acids, etc.) absorption. In the ileum and colon active Na+K+ATPase mediated
salt absorption occurs, primarily in the mature cells lining the villous tips,
water follows iso-osmotically. In addition glucose
facilitated Na+ absorption takes
place in the ileum by Na+ glucose cotransporter; one Na+ ion is
transported along with each molecule of glucose absorbed. This mechanism
remains intact even in severe diarrhoeas.
Absorption of Cl¯ and
HCO3¯ is passive (paracellular) as well as by exchange of HCO3¯
for Cl¯ (transcellular). Bicarbonate is absorbed also by the secretion of H+ (similar
to that in proximal tubule of kidney) and Na+ accompanies it. K+ is excreted in
faecal water by exchange with Na+, as well as by secretion into mucus and in
desquamated cells. The osmotic load of luminal contents plays an important role
in determining final stool water volume. When nonabsorbable solutes are present
and in disaccharidase deficiency (which occurs during starvation), the stool
water is increased. Inhibition of Na+K+ATPase and structural damage to mucosal
cell (by Rota virus) causes diarrhoea by reducing absorption.
Intracellular cyclic
nucleotides are important regulators of absorptive and secretory processes
(Fig. 48.1). Stimuli enhancing cAMP or cGMP cause net loss of salt and water,
both by inhibiting NaCl absorption in villous cells and by promoting anion
secretion (Na+ accompanies) in the crypt cells which are primarily secretory.
Many bacterial toxins, e.g. cholera toxin, exotoxin elaborated by Enterotoxigenic E. coli (ETEC), Staph. aureus, Salmonella, etc. activate
adenylyl cyclase which enhances secretion that reaches its peak after 3–4 hours
and persists until the stimulated cells are shed in the normal turnover, i.e.
36 hours after a single exposure. Concurrent inhibition of absorption adds to
the rate of salt and water loss. Prostaglandins (PGs) and intracellular Ca2+
also stimulate the secretory process. All acute enteric infections produce
secretory diarrhoea. The heat stable toxin (ST) of ETEC, Clostridium difficile and E.
histolytica cause accumulation of cGMP which also stimulates anion
secretion (less potent than cAMP) and inhibits Na+ absorption.
Diarrhoea associated
with carcinoid (secreting 5HT) and medullary carcinoma of thyroid (secreting
calcitonin) is mediated by cAMP. Excess of bile acids also cause diarrhoea by
activating adenylyl cyclase.
Traditionally, hypermotility of bowel has been ascribed a
crucial role in diarrhoea. However, changes in intestinal motility are now
thought to be of secondary importance and may be due to fluid accumulation in
the lumen. Decreased segmenting activity in the intestine may promote diarrhoea
by allowing less time for the absorptive processes.
Principles Of Management
Rational management of diarrhoea depends on establishing the
underlying cause and instituting specific therapy (only if necessary), since
most diarrhoeas are self-limiting. Majority of entero-pathogens are taken care
of by motility and other defence mechanisms of the gut. Therapeutic measures
may be grouped into:
·
Treatment of fluid depletion, shock and
acidosis.
·
Maintenance of nutrition.
·
Drug therapy.
The relative importance of each is governed by the severity and
nature of diarrhoea.
REHYDRATION
In majority of cases, this is the only measure needed.
Rehydration can be done orally or i.v.
Intravenous Rehydration
It is needed only when
fluid loss is severe i.e., > 10% body weight, (if not promptly corrected, it
will lead to shock and death) or if patient is losing > 10 ml/kg/hr, or is
unable to take enough oral fluids due to weakness, stupor or vomiting. The
recommended composition of i.v. fluid (Dhaka fluid) is:
NaCl 85 mM = 5 g
KCl 13 mM = 1 g
NaHCO3 48 mM = 4 g
in 1 L of water or 5% glucose
solution.
This provides 133 mM
Na+, 13 mM K+, 98 mM Cl¯ and 48 mM HCO3 ¯. Ringer lactate (Na+ 130, Cl¯
109, K+ 4, lactate 28 mM) recommended by WHO (1991) could be used
alternatively.
Volume equivalent to 10% BW should be infused over 2–4 hours;
the subsequent rate of infusion is matched with the rate of fluid loss. In most
cases, oral rehydration can be instituted after the initial volume replacement.
Oral Rehydration
Advent of oral
rehydration therapy (ORT) is
considered a major advance of recent times. If the fluid loss is mild (5–7% BW)
or moderate (7.5–10% BW) ORT can be instituted from the very beginning.
Rationale Of ORS Composition
Oral rehydration is
possible if glucose is added with salt. It capitalizes on the intactness of
glucose coupled Na+ absorption, even when other mechanisms have failed or when intestinal
secretion is excessive—the secreted fluid lacks glucose and cannot be
reabsorbed. The composition of oral rehydration salt/solution (ORS) has been
debated. The general principles are:
a)
It should be isotonic or somewhat hypotonic,
i.e. total osmolarity 200–310 mOsm/L (diarrhoea fluids are approximately isotonic
with plasma).
b)
The molar ratio of glucose should be equal to
or somewhat higher than Na+ (excess glucose will be utilized in absorbing Na+
present in the intestinal secretions in addition to that present in ORS
itself), but not exceed 110 mM.
c)
Enough K+ (15–25 mM) and bicarbonate/ citrate
(8–12 mM) should be provided to make up the losses in stool.
The WHO recommended a
standard formula which provided Na+ 90 mM, K+ 20 mM, Cl¯ 80 mM, citrate (base)
10 mM, glucose 110 mM and had a total osmolarity of 310 mOsm/L. Trisod. citrate
was included in place of sod. bicarbonate because bicarbonate containing powder
caked and developed a brown colour due to formation of furfural compounds with glucose:
had a short shelf life.
It has been argued
that the composition of ORS should be varied according to that of the diarrhea
stool. The average electrolyte composition (mM) of 3 important infective diarrhea
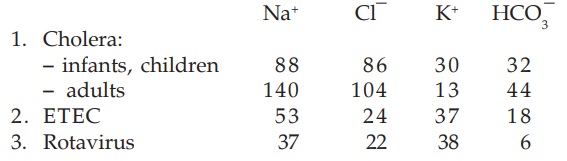
stools is:
As can be seen, the standard WHOORS is based on the composition
of cholera stools, particularly in children. When used in noncholera diarrhoea,
this WHOORS occasionally produces periorbital edema due to excess Na+
absorption. Based also on the Na+ content of ETEC stools, many pediatricians
have favoured 60 mM Na+ and 90 mM glucose ORS for noncholera diarrhoeas.
New Formula WHO-ORS
In 2002 a new formula low
Na+ low glucose ORS has been released by the WHO. Over the past 20 years WHO
sponsored studies were carried out in several developing countries among
children and adults suffering from diarrhoeas. It was found that maximum water
absorption occurs from a slightly hypotonic solution and when glucose concentration
is between 60–110 mM. At higher concentrations, glucose appears in the stools
and takes its osmotic penalty—stool volume is increased. Recent studies showed
that efficacy of ORS in children with acute noncholera diarrhoea is improved by
reducing Na+ and glucose concentration to 75 mM, and total osmolarity to 245
mOsm/L. The need for supplemental i.v. therapy was reduced by 33%. A combined
analysis of studies with low osmolarity ORS has revealed that stool volume is
reduced by 20% and incidence of vomiting by 30%. The new formula ORS has proven
as effective and as safe in cholera as well, both in children and in adults,
but there is some risk of hyponatremia in adults with cholera.
The WHO and UNICEF have recommended replacement of standard (310
mOsm/L) ORS formula by the new (245 mOsm/L).
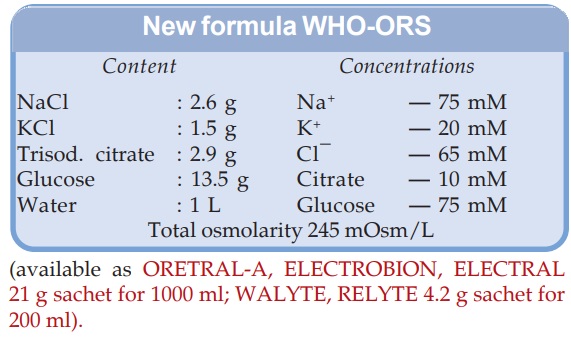
(available as ORETRALA, ELECTROBION,
ELECTRAL 21 g sachet for 1000 ml; WALYTE, RELYTE 4.2 g sachet for 200
ml).
Potassium is an important constituent of ORS, since in most
acute diarrhoeas K+ loss is substantial. The base (bicarbonate, citrate,
lactate) is added to correct acidosis due to alkali loss in stools. It may
independently promote Na+ and water absorption. However, relying on the ability
of the kidney to restore acidbase balance, acidotic states have been managed
without an exogenous base. Base free ORS has been found to be equally effective
in rehydrating, though correction of acidosis is slower. Thus, there is a trend
to consider base as a nonessential constituent of ORS, but if present it may be
beneficial, especially in severe cases with overt acidosis.
Administration Of ORT
Patients are encouraged to drink ORS at ½–1
hourly intervals, initially 5–7.5% BW volume equivalent is given in 2–4 hours
(5 ml/kg/hr in children). Thirst due to volume depletion provides an adequate
driving force. Subsequently it may be left to demand, but should at least cover
the rate of loss in stools. In a weak child who refuses to drink ORS at the
desired rate—it can be given by intragastric drip; restoring hydration in 6
hours should be aimed.
ORT is not designed to stop diarrhoea, but to restore and
maintain hydration, electrolyte and pH balance until diarrhoea ceases, mostly
spontaneously. It is the best and not a second choice approach to i.v.
hydration. About 300 million litre of ORS is being used annually, and is
estimated to be preventing 0.5 million child deaths worldwide.
Non-diarrhoeal Uses Of ORT
a) Postsurgical, postburn
and posttrauma maintenance of hydration and nutrition (in place of i.v.
infusion).
b) Heat stroke.
c) During changeover from
parenteral to enteral elimentation.
Super ORS
This is a solution
which in addition to rehydrating may lead
to decrease in purging rates and improvement in diarrhoea by enhanced
absorption. Improvement in ORS by adding certain actively transported amino acids
(alanine, glycine which cotransport Na+) has been tried. Their efficacy is marginal,
and not extended to noncholera diarrhoea; cost-effectiveness may not be
favourable. There is compelling evidence, however, that a complex substrate
like boiled rice powder 40–50 g/L is an efficient substitute for glucose. The
rice starch is slowly hydrolysed at the brush border or in the lumen into glucose
which is absorbed: does not cause osmotic diarrhoea even when larger quantity
is added: more calories can be administered. Rice has 7% protein: yields amino
acids which may themselves stimulate salt and water absorption. It has been
found to reduce stool volume compared to WHOORS in cholera patients. Moreover,
rice is cheap and widely available. Thus, rice (or wheat, maize, potato) based
ORS appears to be suitable for developing countries.
MAINTENANCE OF NUTRITION
Contrary to
traditional view, patients of diarrhoea should not be starved. Fasting
decreases brush border disaccharidase enzymes and reduces absorption of salt,
water and nutrients; may lead to malnutrition if diarrhoea is prolonged or recurrent.
Feeding during diarrhoea has been shown to increase intestinal digestive
enzymes and cell proliferation in mucosa. Simple foods like breast milk or ½
strength buffalo milk, boiled potato, rice, chicken soup, banana, sago, etc.
should be given as soon as the patient can eat.
DRUG THERAPY
It consists of:
·
Specific antimicrobial drugs.
·
Nonspecific antidiarrhoeal drugs.
ANTIMICROBIALS
One or more
antimicrobial agent is almost routinely prescribed to every patient of diarrhoea.
However, such drugs have a limited role in the overall treatment of diarrhoeal
patients; the reasons are:
i. Bacterial pathogen is
responsible for only a fraction of cases.
ii. Even in bacterial diarrhoea,
antimicrobials alter the course of illness only in selected cases.
iii. Antimicrobials may
prolong the carrier state.
Diarrhoea patients can
generally be placed in one of the two categories:
a) Abundant watery
diarrhoea lacking mucus or blood, usually dehydrating with frequent vomiting,
but little or no fever—are generally caused by adhesive but noninvasive
enterotoxigenic bacteria such as cholera, ETEC, Salmonella enteritidis or by rota virus and other viruses which stimulate massive secretion by
activating cAMP: ORS and not antimicrobials are the main therapy.
b) Slightly loose, smaller
volume stools, frequently with mucus and/or blood, mild dehydration, usually
attended with fever and abdominal pain, but not vomiting—are indications of
mucosal invasion, generally caused by entero-invasive organisms like Shigella, enteropathogenic E. coli (EPEC), Campy. jejuni, Salmonella typhimurium,
Yersinia enterocolitica, E. histolytica, Clostri. difficile; antimicrobials
are needed in many of these.
A. Antimicrobials Are Of No Value In diarrhoea due to noninfective causes, such as:
·
Irritable bowel syndrome (IBS)
·
Coeliac disease
·
Pancreatic enzyme deficiency
·
Tropical sprue (except when there is secondary
infection)
·
Thyrotoxicosis.
Rotavirus is an important pathogen
of acute diarrhoea, especially in
children in developed countries. It along with other diarrhoea causing viruses,
is not amenable to chemotherapy.
Salmonella
food poisoning is generally a self-limiting disease. Antibiotics
have been widely used, but may be harmful rather than beneficial—treated patients
pass organisms in stool for longer periods than untreated patients. However,
very severe illness or that in infants, elderly or immune-compromized patients
may be treated with ciprofloxacin/azithromycin/i.v. ceftriaxone.
B. Antimicrobials
Are Useful Only In Severe Disease (but not in mild cases):
i) Travellers’ Diarrhoea:
mostly due to ETEC, Campylobacter or
virus: cotrimoxazole, norfloxacin, doxycycline and erythromycin reduce the
duration and total fluid needed only in severe cases.
ii)
EPEC: is less common, but causes Shigellalike invasive illness.
Cotrimoxazole, colistin, nalidixic acid or norfloxacin may be used in acute
cases and in infants. Efficacy of ampicillin has declined due to development of
resistance.
iii)
Shigella enteritis: only when associated with blood and mucus in stools may be treated with ciprofloxacin,
norfloxacin or nalidixic acid; cotrimoxazole and ampicillin are alternatives,
but many strains are resistant to these.
iv) Salmonella
typhimurium enteritis is often invasive; severe cases may be treated
with a fluoroquinolone, cotrimoxazole or ampicillin.
v) Yersinia
enterocolitica: common in colder places, not in tropics. Cotrimoxazole
is the most suitable drug in severe cases; ciprofloxacin is an alternative.
C. Antimicrobials Are Regularly Useful in:
i) Cholera: Though not life
saving, tetracyclines reduce stool volume to nearly ½. Cotrimoxazole is an
alternative, especially in children. Lately, multidrug resistant cholera
strains have arisen: can be treated with norfloxacin/ciprofloxacin. Ampicillin
and erythromycin are also effective.
ii) Campylobacter
jejuni: Norfloxacin and other fluoroquinolones eradicate the organism
from the stools and control diarrhoea. Erythromycin is fairly effective and is
the preferred drug in children.
iii)
Clostridium difficile: produces antibiotic associated pseudomembranous
enterocolitis. The drug of choice for it is metronidazole, while vancomycin
given orally is an alternative. Offending antibiotic must be stopped.
iv) Diarrhoea associated with bacterial growth in blind loops/diverticulitis
may be treated with tetracycline or metronidazole.
v) Amoebiasis
metronidazole, diloxanide furoate,
vi) Giardiasis are effective drugs (see Ch. No. 60).
NON-SPECIFIC ANTIDIARRHOEAL AGENTS
These are classified and their uses listed in Table 48.2.
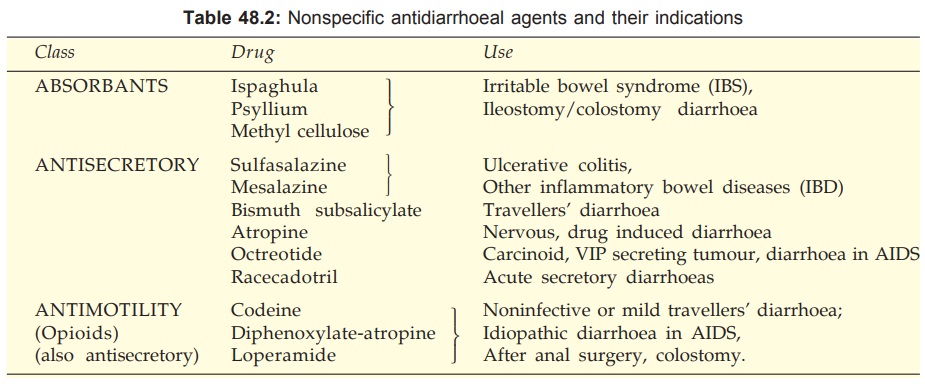
1. Absorbants
These are colloidal
bulk forming substances which
absorb water and swell. They modify the consistency and frequency of stools and
give an impression of improvement, but do not reduce the water and electrolyte
loss. They are of value in selected conditions (Table 48.2). Ispaghula and other
bulk forming colloids are useful in both constipation and diarrhoea phases of
IBS and reduce abdominal pain as well.
2. Antisecretory
Drugs
Sulfasalazine (Salicylazosulfapyridine)
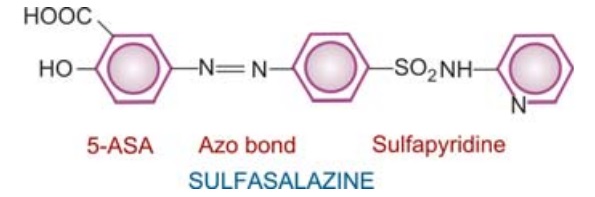
It is a compound of 5aminosalicylic acid (5ASA) with
sulfapyridine linked through an azo bond that has a specific therapeutic effect
in inflammatory bowel diseases (IBDs) like ulcerative colitis and Crohn’s
disease.
Having low solubility,
it is poorly absorbed from the ileum. The azo bond is split by colonic bacteria
to release 5ASA and sulfapyridine. The former exerts a local anti-inflammatory
effect, the mechanism of which is not clear. Though it inhibits both COX and
LOX, decreased PG and LT production appears to play a minor role in the therapeutic
effect. Inhibition of cytokine, PAF, TNFα and nuclear
transcription factor (NFκB) generation seems to be more important.
Migration of inflammatory cells into bowel wall is interfered and mucosal
secretion is reduced— affords considerable relief in ulcerative colitis and
related inflammatory bowel diseases. Given during an exacerbation it reduces
number of stools, abdominal cramps and fever, but is less effective than
corticosteroids; may be employed for mild to moderate exacerbation. A dose of
3– 4 g/day induces remission over a few weeks in many cases, but relapses are
common after stoppage. Maintenance therapy with 1.5–2 g/day has been found to
postpone relapse as long as taken. The primary value of sulfasalazine is in
maintaining remission, while corticosteroids are reserved to treat acute exacerbations.
The beneficial effect
of sulfasalazine is clearly not due to any antibacterial action (bowel flora remains
largely unaffected): sulfapyridine moiety only serves to carry 5ASA to the
colon without being absorbed proximally. However, part of the released
sulfapyridine is absorbed in the colon and is responsible for adverse effects
like rashes, fever, joint pain, haemolysis and blood dyscrasias. Nausea,
vomiting, headache, malaise and anaemia are other frequent side effects. Upto
1/3rd patients suffer intolerable adverse effects. Oligozoospermia and
male infertility is reported. Sulfasalazine interferes with folate absorbtion;
folic acid supplementation should be given during its use.
Sufasalazine has also
been used as a disease modifying drug in rheumatoid arthritis: the absorbed
sulfapyridine appears to be responsible for the therapeutic effect.
SALAZOPYRIN, SAZOEN
0.5 g tab.
Mesalazine (Mesalamine)
These are the official names given to 5ASA. Realizing that 5ASA
is the active moiety in ulcerative colitis, but is not effective orally because
of inability to reach the large bowel (it is absorbed in the small intestine),
it has been formulated as delayed release preparations by coating with acrylic
polymer. The pattern of release over the length of jejunum, ileum and colon
differs among the different formulations, but most of them do effectively
deliver 5ASA to the distal small bowel and colon. A daily dose of 2.4 g has
been found to improve over 50% patients of ulcerative colitis (upto 80% mild-to-moderate
cases). Less than half of the 5ASA released from these preparations is
absorbed, acetylated in the liver and excreted in urine. Like sulfasalazine,
the primary use of mesalazine is in preventing relapses, though it may also be
employed to treat mild-to-moderate exacerbations.
MESACOL, TIDOCOL 400
mg tab, ETISA 500 mg sachet.
Adverse Effects
Coated mesalazine is
better tolerated than
sulfasalazine. Side effects noted are nausea, diarrhoea, abdominal pain and
headache, but are mild and less frequent. Rashes and hypersensitivity reactions
are rare. Bone marrow depression and decreased sperm count has not occurred.
Mesalazine has nephrotoxic potential, because 30–40% of 5ASA is released in the
ileum and is absorbed. It is contraindicated in renal and hepatic impairment.
Drug Interactions Coated mesalazine may enhance the gastric toxicity of glucocorticoids and hypoglycaemic
action of sulfonylureas. Interaction with coumarins, furosemide,
spironolactone, methotrexate and rifampicin are possible.
5-ASA Enemas: Another mode of delivery
of 5-ASA to colon is to
administer it by a retention enema: 1–2 g enema once or twice daily is
effective in distal ulcerative colitis, including some refractory cases.
MESACOL ENEMA 4 g/60
ml.
Olsalazine
It consists of two molecules of 5ASA coupled together by azo bond. It is poorly absorbed in
the ileum, the azo bond is split in the colon to provide 5ASA locally. No separate
carrier moiety is needed. Olsalazine is probably the most reliable preparation
for delivery of 5ASA to the colon. However, it often aggravates diarrhoea
initially by decreasing transit time through the bowels.
Balsalazine
This is 5-ASA linked to 4aminobenzoylβalanine as the
carrier. The 5-ASA is released in the colon and the carrier is poorly absorbed.
Corticosteroids
Prednisolone (40 mg/day) or equivalent are highly
effective in controlling symptoms/inducing remission in both ulcerative colitis
and Crohn’s disease. They are the drugs of choice for moderately severe
exacerbations. Hydrocortisone enema, or foam (ENTOFOAM 10%) can be used for topical
treatment of proctitis and distal ulcerative colitis. Corticosteroids
are generally discontinued after remission is induced, and mesalazine started
during steroid therapy is continued to prevent relapses.
A sizeable percentage of severe IBD patients either relapse on
stoppage of the steroid (steroid-dependent) or do not respond to it (steroid-resistant).
Increasing use of specific immunosuppressant drugs is now being made in such
IBD patients, particularly to avoid long-term steroid therapy which carrys
hazards.
Immunosuppressants
Azathioprine is the most commonly used immunosuppressant in
IBD. Though the response is delayed— occurring after weeks or months, it has
lower toxicity. Azathioprine is used for moderate-to-severe Crohn’s disease as
well as ulcerative colitis, especially as a steroid sparing drug or in steroid
resistant cases. It has good remission maintaining property.
Methotrexate is also effective in
IBD and acts faster, but higher doses are
needed than for rheumatoid arthritis. In IBD, efficacy by oral route is lower.
Thus, it has a limited role in severe Crohn’s disease only.
Cyclosporine can be used to maintain remission in both Crohn’s as well as ulcerative colitis, but is
not a first line immunosuppressant because of renal toxicity, and poor oral
efficacy in IBD.
Infliximab: This chimeric antiTNFα immunoglobulin has shown promising effect in IBD and is being
increasingly used for severe uncontrolled cases.
Bismuth Subsalicylate
Taken as suspension
(60 ml 6 hourly) it is thought
to act by decreasing PG synthesis in the intestinal mucosa, thereby reducing
Cl¯ secretion. It has some prophylactic value in travellers’ diarrhoea;
(probably due to weak antibacterial action also), but it is rather inconvenient
to carry and take.
Anticholinergics
Atropinic drugs can
reduce bowel motility and
secretion, but have poor efficacy in secretory diarrhoeas. They may benefit
nervous/drug (neostigmine, metoclopramide, reserpine) induced diarrhoeas and
provide some symptomatic relief in dysenteries, diverticulitis.
Octreotide
This somatostatin
analogue has a long plasma t½ (90
min) as well as potent antisecretory/ antimotility action on the gut. It has
been used to control diarrhoea in carcinoid and vasoactive intestinal peptide
(VIP) secreting tumours, and for refractory diarrhoea in AIDS patients, but needs
to be given by s.c. injection.
Opioids
In addition to their
well recognized antimotility action, opioids reduce
intestinal secretion. Loperamide has been clearly shown to reduce secretion,
probably through specific opioid receptors, but does not affect mucosal cAMP or
cGMP levels.
Racecadotril
This recently
introduced prodrug is rapidly converted to thiorphan,
an enkephalinase inhibitor. It prevents degradation of endogenous enkephalins
(ENKs) which are mainly δ opioid receptor agonists. Racecadotril
decreases intestinal hypersecretion, without affecting motility, by lowering
mucosal cAMP due to enhanced ENK action. It is indicated in the shortterm
treatment of acute secretory diarrhoeas. In contrast to loperamide/diphenoxylate,
it is not contraindicated in children. The elimination t½ as thiorphan is 3 hr.
Side effects are nausea, vomiting, drowsiness, flatulence.
Dose: 100 mg (children 1.5
mg/kg) TDS for not more than 7 days.
CADOTRIL, RACIGYL 100
mg cap, 15 mg sachet; REDOTIL 100 mg cap.
3. Antimotility Drugs
These are opioid drugs which increase small bowel tone and
segmenting activity, reduce propulsive movements and diminish intestinal
secretions while enhancing absorption. The major action appears to be mediated
through μ opioid receptors located
on enteric neuronal network, but direct action on intestinal smooth muscle and
secretory/absorptive epithelium has also been demonstrated. The δ receptors are
believed to promote absorption and inhibit secretion, while the μ receptors enhance
absorption and decrease propulsive movements. Overall they increase resistance
to luminal transit and allow more time for the absorptive processes. No
tolerance develops to their constipating action.
Codeine
This opium alkaloid has prominent constipating
action at a dose of 60 mg TDS. The antidiarrhoeal effect is attributed
primarily to its peripheral action on small intestine and colon. It does have
central effects, but dependence producing liability is low. Side effects are
nausea, vomiting and dizziness. It should be used only for short periods and
with caution in children.
Diphenoxylate (2.5 mg) + atropine (0.025 mg): LOMOTIL tab
and in 5 ml liquid.
Dose: 5–10 mg, followed by
2.5–5 mg 6 hourly.
It is a synthetic opioid, chemically related to pethidine; used
exclusively as constipating agent; action is similar to codeine. The anti-diarrhoeal
action is most prominent, but because it is absorbed systemically and crosses
blood-brain barrier—CNS effects do occur. Atropine is added in sub-pharmacological
dose to discourage abuse by taking several tablets. Abuse liability is rated
low, and overdose will produce disturbing atropinic side effects. It has caused
respiratory depression, paralytic ileus and toxic megacolon in children.
Response is more variable in them—contraindicated below 6 years of age.
Loperamide
It is an opiate
analogue with major peripheral μ opioid and additional
weak anticholinergic property. As a constipating agent it is much more potent
than codeine. Because of poor water solubility—little is absorbed from the
intestines. Entry into brain is negligible—CNS effects are rare and occur only with
high doses; no abuse liability. The duration of action is longer (12 hr) than
codeine and diphenoxylate.
In addition to its
opiate like action on motility, loperamide also inhibits secretion: directly
interacts with calmodulin—this may be responsible for the anti-diarrhoeal
action. It improves faecal continence by enhancing anal sphincter tone.
Adverse Effects: Abdominal cramps and
rashes are the most common
side effects. Paralytic ileus, toxic megacolon with abdominal distension is a
serious complication in young children—fatalities have occurred, probably due
to absorption of toxins from the intestines: contraindicated in children < 4
yr. Loperamide appears to be the most effective and most suitable of the antimotility
drugs.
Dose: 4 mg followed by 2
mg after each motion (max. 10 mg in a
day); 2 mg BD for chronic diarrhoea.
IMODIUM, LOPESTAL,
DIARLOP: 2 mg tab, cap.
Liquid formulation has
been withdrawn.
The utility of
antimotility drugs in diarrhoea is limited to noninfective diarrhoea, mild traveller’s
diarrhoea, and when diarrhoea is exhausting or idiopathic diarrhoea in AIDS
patients. Their use is a shortterm measure only.
Antimotility drugs are
contraindicated in acute infective diarrhoeas because they delay clearance of
the pathogen from the intestine. If invasive organisms (Shigella, EPEC, EH, etc.) are present, antimotility drugs can be
disastrous. They are contraindicated in irritable bowel syndrome, ulcerative
colitis and diverticulosis because they increase intraluminal pressure.
Antimotility drugs can
be used to induce deliberate shortterm constipation, e.g. after anal surgery,
and to reduce the volume, fluidity and bag cleaning frequency in
ileostomy/colostomy patients.
NOTE:
Drugs Controller General of India has banned the following category of antidiarrhoeal
drugs:
· Containing adsorbants like Kaolin, pectin,
attapulgite, activated charcoal, etc.
· Containing phthalylsulfathiazole,
succinylsulfathiazole, sulfaguanidine, neomycin, streptomycin, dihydrostreptomycin.
· For pediatric use containing
diphenoxylate, loperamide, atropine, belladonna,
hyosciamine, halogenated hydroxyquinolines.
·
Fixed dose combinations of antidiarrhoeals
with electrolytes.
·
Fixed dose combination of loperamide with
furazolidone.
·
Fixed dose combination of antidiarrhoeals with
antihistaminics
Related Topics
