Current systems
| Home | | Hospital pharmacy |Chapter: Hospital pharmacy : Medicines supply and automation
In recognising that many processes had changed little since the 1970s and 1980s, a number of factors have influenced the systems and processes for the supply of medicines in UK hospitals over the past decade.
Current systems
In recognising that
many processes had changed little since the 1970s and 1980s, a number of
factors have influenced the systems and processes for the supply of medicines
in UK hospitals over the past decade. Hospitals have a much higher occupancy
rate, with reduced lengths of stay. There has been an increased emphasis on
clinical governance and growing awareness of medication errors. Patients have
more chronic illnesses and complex medication regimens. The European Community
Directive 92/27 was incorporated into UK law on 1 January 1999. It required,
amongst other things, that all medicines supplied to patients should include a
patient information leaflet (PIL) and be labelled with the product batch number
and expiry date. The directive was one of the key drivers behind the
introduction of original pack dispensing into hospital practice. Traditional
practice of limiting discharge supplies and split-ting packs risked non-compliance
with the law and possible prosecution.
Along with
individual patient dispensing and the more recent models of supply, the use of
patient bedside medicine cabinets is now widely adopted as an established
practice across the NHS. The benefits of the cabinets are that individual
patients’ medicines are kept at their bedside, reducing the risk of selection
errors and errors of omission and, in addition, the traditional nursing drug
trolley, which was traditionally crammed with a huge array of medicines, is now
a much more streamlined operation which also has the benefit of reducing
selection error.
It is perhaps
helpful to mention the arrangements under which hospital pharmacies operate at
this point. Unlike community pharmacies, hospital pharmacy departments do not
require premises registration with the General Pharmaceutical Council to
provide services to their wards and out-patients. Whilst at the time of writing
the Medicines Act is under review, the current exemption is based on section 10
of the Act and relates to a ‘hospital’s normal business’. Hospital pharmacies
do have quality systems and detailed standard operating procedures for
dispensing and supply just as required for registered pharmacies. However, many
hospital pharmacies do register: this became common when Crown immunity was
removed over 20 years ago. This permits them to undertake other activities not
‘normal business of a hospital’ and where this is the case the responsible
pharmacist requirements apply. A detailed discussion of this is beyond the
remit of this chapter. Details about responsible pharmacist can be found on the
General Pharmaceutical Council website at
http://www.pharmacyregulation.org/regulatingpharmacy/thepharmacyregister/responsiblepharmacist/index.aspx.
Non-stock dispensing
The choice of
inpatient supply system for a hospital lies anywhere on a spectrum between
total stock and almost complete individual dispensing. Whilst the former was
the traditional Scottish system and the latter is favoured in private hospitals
because it facilitates charging, the choice in NHS hospitals throughout the UK
should now be based on a careful risk appraisal of the options and resources
(principally staff) available.
'One-stop dispensing'
Original pack
dispensing has now been widely adopted across most hospitals in the UK and is
referred to as ‘one-stop dispensing’ or ‘dispensing for discharge’. The concept
is to combine inpatient and discharge dispensing into a single supply, labelled
with directions for use. In this system, patients’ medicines are supplied as
soon as they are needed, and labelled for discharge so that only one supply is
made during the patient’s stay. Manufacturers’ original packs are usually
dispensed and the patient is discharged with what remains after use in
hospital. If this is less than a minimum quantity agreed with local general
practitioners (GPs), usually 2 weeks’ supply, an additional pack is issued.
Large numbers of individually dispensed items cannot be handled in a
conven-tional medicines trolley, so each patient normally has a bedside
medicines cabinet, which can also be used for the patient’s own drugs (PODs:
see later in chapter) or in a self-administration scheme. To operate
efficiently, a judge-ment needs to be made about which medicines can be
relabelled for discharge early in the patient’s admission, and which cannot.
For example, aspirin 75 mg tablets for cardiovascular disease are almost
universally prescribed and taken by patients as a once-daily dose and,
similarly, statins are also taken once at night. Therefore it would be
reasonably safe to make the assumption that, provided the patient continues to
take the medicine after discharge, the directions will probably not change.
However, in the case of warfarin, corti-costeroids or antibiotics, for example,
it is likely that doses or duration of treatment will change before or at the
point of discharge, such that labelling them before this point is somewhat
risky. These also reduce the risk of medi-cation error by limiting the choices
for selection at administration times and allow nurses to give more
individualised patient care. There is a need to keep the contents of cabinets
up to date with prescription changes and, at discharge, to check that the pack
quantity and label are still appropriate and that the cabinet is empty, all of
which may be undertaken by a pharmacist or technician.
Patients benefit by
having PILs provided and by avoiding the wait for discharge medicines to be
dispensed, provided that the prescription is written in good time, and also by
having more time before ordering repeat prescrip-tions. The hospital can meet
its legal obligation on PILs and also benefits from speedier discharges.
The Royal
Pharmaceutical Society’s Hospital Pharmacists Group has pro-duced useful guidance
on the introduction of one-stop dispensing, use of PODs and self-administration
schemes. Using patient packs at the time of discharge, a possible intermediate
step to one-stop dispensing, has also been successful.
The review of
medicines management in NHS hospitals undertaken by the Audit Commission in
2001 and the recommendations made have had a pro-found impact on the
modernisation of the dispensing process. Many NHS hospitals have installed
automated dispensing systems in the past decade as a consequence of the
recommendations. A number of commercial systems are now available that
accurately pick original patient packs to support the one-stop dispensing
process and support re-engineering of services. Figure 4.1 provides an example
of such a system the ARX Rowa from the Countess of Chester NHS Foundation
Trust.
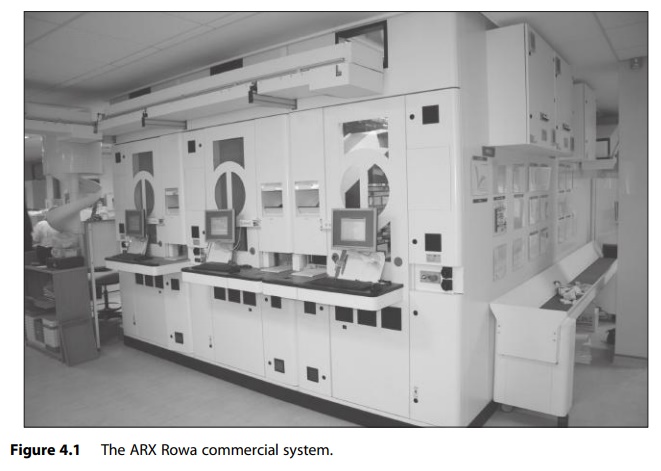
Scanning of bar
codes is also used in loading such machines, enabling the robot to identify
different products, strengths or pack sizes. Products can be packed very
compactly because any gaps can be filled without regard to any human need for
selection, as positions are memorised by the system’s com-puter. The machines
can also occupy less floor space than an equivalent amount of conventional
shelving. A number of studies have shown the bene-ficial impact on dispensing
errors, reduced dispensary turnaround times, simplified ordering systems,
improved reliability of service and more efficient use of staff.
Patients' own drugs
Patients admitted to
hospital are usually asked to bring their medicines with them to facilitate the
recording of their drug history and some trusts run publicity campaigns on bus
adverts and in GP practices to promote this. Traditionally, PODs were routinely
returned to pharmacy for destruction once a hospital supply was obtained.
However, the move to dispensing of prescriptions in primary care using
manufacturers’ original packs has given much greater confidence in their
continued usefulness, but only for the patient to whom they were originally
supplied. Before use their suitability must be assessed, with this being
variously undertaken by pharmacists, technicians, doctors or nurses at
different hospitals. Most hospitals will have a policy or set of procedures
covering this. Reuse of patients’ own medicines has a number of benefits,
including the reduced risk of medication errors, since PODs can be used a
reference to patients’ medicines consumption prior to admission.
When the directions
are inappropriate, relabelling by pharmacy staff may be permissible. As with
one-stop dispensing, further checks on directions and quantities are required
on discharge. The importance of these, including the check that the locker has
been emptied, has been shown by reported errors, which also highlight the need
for thorough training of those involved. Guidance on implementation includes
the need for publicity to encourage patients to bring in their medicines.
Unit dose systems
Unit dose systems
have been adopted quite widely in North America and many European countries but
have only been tried to a limited extent in the UK. The concept is that
pharmacy provides medicines to wards in single-unit packages, either just prior
to the time of administration or on a daily or (for long-stay) weekly basis,
placing them in the patient’s individually labelled drawer in a medicine
cabinet, trolley or cassette. Because of the labour-intensive nature of this
work, and the advent of original pack dispensing, it has not been widely adopted
in the UK.
Related Topics
