Salicylates - Aspirin
| Home | | Pharmacology |Chapter: Essential pharmacology : Nonsteroidal Anti-inflammatory Drugs And Antipyreticanalgesics
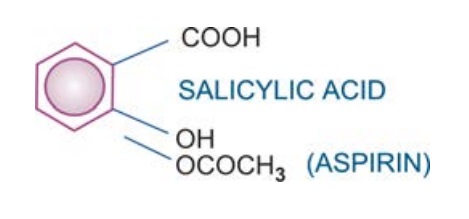
Aspirin is acetyl salicylic acid. It is rapidly converted in the body to salicylic acid which is responsible for most of the actions. Other actions are the result of acetylation of certain macro-molecules including COX. It is one of the oldest analgesic anti-inflammatory drugs and is still widely used.
SALICYLATES
Aspirin (prototype)
Aspirin is
acetyl salicylic acid. It is rapidly converted in the body to salicylic acid
which is responsible for most of the actions. Other actions are the result of
acetylation of certain macro-molecules including COX. It is one of the oldest
analgesic anti-inflammatory drugs and is still widely used.
Pharmacological Actions
1. Analgesic, Antipyretic, Anti-Inflammatory
Actions
Aspirin is a weaker analgesic than morphine type drugs: aspirin 600 mg ~
codeine 6 mg. However, it
effectively relieves inflammatory, tissue injury related, connective tissue and
integumental pain, but is relatively ineffective in severe visceral and
ischaemic pain. The analgesic action is mainly due to obtunding of peripheral
pain receptors and prevention of PG-mediated sensitization of nerve endings. A central
subcortical action raising threshold to pain perception also contributes, but
the morphinelike action on psychic processing or reaction component of the pain is missing. No sedation, subjective
effects, tolerance or physical dependence is produced.
Aspirin
resets the hypothalamic thermostat and rapidly reduces fever by promoting heat
loss (sweating, cutaneous vasodilatation), but does not decrease heat production.
Anti-inflammatory
action is exerted at high doses (3–6 g/day or 100 mg/kg/ day). Signs of
inflammation like pain, tenderness, swelling, vasodilatation and leucocyte infiltration
are suppressed. In addition to COX inhibition, quenching of free radicals may
contribute to its anti-inflammatory action.
2. Metabolic Effects
These are significant only at anti-inflammatory doses. Cellular
metabolism is increased, especially in skeletal muscles, due to uncoupling of
oxidative phosphorylation → increased heat production. There is increased
utilization of glucose → blood sugar may decrease (especially in diabetics)
and liver glycogen is depleted. However, hyperglycaemia is often seen at toxic
doses: this is due to central sympathetic stimulation → release of Adr and
corticosteroids. Chronic use of large doses cause negative N2
balance by increased conversion of protein to carbohydrate. Plasma free fatty
acid and cholesterol levels are reduced.
3. Respiration
The effects are dose dependent. At anti-inflammatory doses, respiration is
stimulated by peripheral (increased CO2 production) and central
(increased sensitivity of respiratory centre to CO2) actions.
Hyperventilation is prominent in salicylate poisoning. Further rise in
salicylate level causes respiratory depression; death is due to respiratory
failure.
4. Acidbase And Electrolyte Balance
Anti-inflammatory
doses produce significant changes in the acidbase and electrolyte composition
of body fluids. Initially, respiratory stimulation predominates and tends to
wash out CO2 despite increased production → respiratory
alkalosis, which is compensated by increased renal excretion of HCO¯ (with
accompanying Na+, K+ and water). Most adults treated with 4–5 g/day of aspirin
stay in a state of compensated
respiratory alkalosis.
Still higher doses
cause respiratory depression with CO2 retention, while excess CO2
production continues → respiratory
acidosis. To this are added dissociated salicylic acid as well as metabolic
acids (lactic, pyruvic, acetoacetic) which are produced in excess +
metabolically derived sulfuric and phosphoric acid which are retained due to
depression of renal function. All these combine to cause uncompensated metabolic acidosis
since plasma HCO3¯ is already low. Most children manifest this phase during salicylate poisoning; while in
adults it is seen in late stages of poisoning only.
Dehydration
occurs in poisoning due to increased water loss in urine (to
accompany Na+, K+ and HCO¯) increased sweating and hyperventilation.
5. CVS
Aspirin has no direct effect in therapeutic doses. Larger doses
increase cardiac output to meet increased peripheral O2 demand and
cause direct vasodilatation. Toxic doses depress vasomotor centre: BP may fall.
Because of increased cardiac work as well as Na+ and water retention, CHF may
be precipitated in patients with low cardiac reserve.
6. GIT
Aspirin and released salicylic acid irritate gastric mucosa → cause epigastric
distress, nausea and vomiting. It also stimulates CTZ: vomiting has a central
component as well at higher doses.
Aspirin
(pKa 3.5) remains unionized and diffusible in the acid gastric juice, but on
entering the mucosal cell (pH 7.1) it ionizes and becomes indiffusible. This
‘ion trapping’ in the gastric mucosal cell enhances gastric toxicity. Further,
aspirin pCh. No. coming in contact with gastric mucosa promotes local back
diffusion of acid → focal necrosis of mucosal cells and capillaries → acute ulcers, erosive
gastritis, congestion and microscopic haemorrhages. The occult blood loss in
stools is increased by even a single tablet of aspirin; averages 5 ml/day at anti-inflammatory
doses. Haematemesis occurs occasionally: may be an idiosyncratic reaction.
Soluble
aspirin tablets containing calcium carbonate + citric acid and other buffered
preparations are less liable to cause gastric ulceration.
7. Urate excretion
Doserelated effect is seen: < 2 g/day—urate
retention and antagonism of all other uricosuric drugs.
2–5
g/day—variable effects, often no change. > 5 g/day—increased urate
excretion.
Aspirin
is not suitable for use in chronic gout.
8. Blood
Aspirin, even in small doses, irreversibly inhibits TXA2
synthesis by platelets. Thus, it interferes with platelet aggregation and bleeding
time is prolonged to nearly twice the normal value. This effect lasts for about
a week (turnover time of platelets).
Longterm
intake of large dose decreases synthesis of clotting factors in liver and predisposes
to bleeding; can be prevented by prophylactic vit K therapy.
Pharmacokinetics
Aspirin
is absorbed from the stomach and small intestines. Its poor water solubility is
the limiting factor in absorption: microfining the drugpCh. No.s and inclusion
of an alkali (solubility is more at higher pH) enhances absorption. However,
higher pH also favours ionization, thus decreasing the diffusible form.
Aspirin is rapidly
deacetylated in the gut wall, liver, plasma and other tissues to release salicylic
acid which is the major circulating and active form. It is ~80% bound to plasma
proteins and has a volume of distribution ~0.17 L/kg. It slowly enters brain
but freely crosses placenta. Both aspirin and salicylic acid are conjugated in
liver with glycine → salicyluric acid (major pathway); and with glucuronic acid. Few
other minor metabolites are also produced. The metabolites are excreted by
glomerular filtration as well as tubular secretion. Normally, only 1/10th is
excreted as free salicylic acid, but this can be increased by alkalinization.
The plasma t½ of
aspirin as such is 15–20 min, but taken together with that of released
salicylic acid, it is 3–5 hours. However, metabolic processes get saturated
over the therapeutic range; t½ of anti-inflammatory doses may be 8–12 hours
while that during poisoning may be up to 30 hours. Thus, elimination is dose
dependent.
Adverse Effects
Side Effects that occur at
analgesic dose (0.3–1.5 g/day) are
nausea, vomiting, epigastric distress, increased occult blood loss in stools.
The most important adverse effect of aspirin is gastric mucosal damage and
peptic ulceration.
Hypersensitivity and Idiosyncrasy Though infrequent, these can be serious. Reactions
include rashes, fixed drug eruption, urticaria, rhinorrhoea, angioedema, asthma
and anaphylactoid reaction. Profuse gastric bleeding occurs in rare instances.
Anti-Inflammatory Doses (3–5 g/day) produce the syndrome called salicylism—dizziness,
tinnitus, vertigo, reversible impairment of hearing and vision, excitement and
mental confusion, hyperventilation and electrolyte imbalance. The dose has to
be titrated to one which is just below that producing these symptoms; tinnitus
is a good guide.
Aspirin therapy in
children with rheumatoid arthritis has been found to raise serum transaminases,
indicating liver damage. Most cases are asymptomatic but it is potentially
dangerous. An association between salicylate therapy and ‘Reye’s syndrome’, a
rare form of hepatic encephalopathy seen in children having viral (varicella,
influenza) infection has been noted.
In adults also, longterm
therapy with high dose aspirin can cause insidious onset hepatic injury. Salt
and water retention occurs in a dose related manner.
Acute salicylate poisoning It is more common in
children. Fatal dose in adults is estimated to be 15–30 g, but is considerably
lower in chil dren. Serious toxicity is seen at serum salicylate levels > 50
mg/dl. Manifestations are:
Vomiting,
dehydration, electrolyte imbalance, acidotic breathing, hyper/hypoglycaemia,
petechial haemorrhages, restlessness, delirium, hallucinations, hyperpyrexia, convulsions,
coma and death due to respiratory failure + cardiovascular collapse.
Treatment is symptomatic and
supportive. Most important is
external cooling and i.v. fluid with Na+, K+, HCO¯ and glucose: according to
need determined by repeated monitoring. Gastric lavage to remove unabsorbed
drug; forced alkaline diuresis or haemodialysis to remove absorbed drug is
indicated in severe cases. Blood transfusion and vit K should be given if
bleeding occurs.
Precautions And Contraindications
·
Aspirin is contraindicated in patients who are
sensitive to it and in peptic ulcer, bleeding tendencies, in children suffering
from chicken pox or influenza. Due to risk of Reye’s syndrome pediatric
formulations of aspirin are prohibited in India and the UK.
·
In chronic liver disease: cases of hepatic
necrosis have been reported.
·
It should be avoided in diabetics, in those
with low cardiac reserve or frank CHF and in juvenile rheumatoid arthritis.
·
Aspirin should be stopped 1 week before elective
surgery.
·
Given during pregnancy it may be responsible
for low birth weight babies. Delayed or prolonged labour, greater postpartum
blood loss and premature closure of ductus arteriosus are possible if aspirin
is taken at or near term.
·
It should be avoided by breastfeeding mothers.
·
Avoid high doses in G6PD deficient
individuals—haemolysis can occur.
Interactions
Aspirin displaces
warfarin, naproxen, sulfonylureas, phenytoin and methotrexate from
binding sites on
plasma proteins: toxicity of these drugs may occur. Its antiplatelet action
increases the risk of bleeding in patients on oral anticoagulants.
It inhibits tubular secretion of uric acid (at analgesic doses)
and antagonizes uricosuric action of probenecid. Tubular secretion of methotrexate
is also interfered.
Aspirin blunts diuretic action of furosemide and thiazides and
reduces K+ conserving action of spironolactone. Competition between canrenone
(active metabolite of spironolactone) and aspirin for active transport in proximal
tubules has been demonstrated.
Aspirin reduces protein bound iodine levels by displacement of
thyroxine; but hypothyroidism does not occur.
USES
1. As Analgesic
For headache (including mild migraine), backache, myalgia,
joint pain, pulled muscle, toothache, neuralgias and dysmenorrhoea; it is
effective in low doses (0.3–0.6 g 6–8 hourly). Analgesic effect is maximal at ~
1000 mg (single dose).
2. As Antipyretic
It is effective in fever of any origin; dose is same
as for analgesia. However, paracetamol, being safer, is generally preferred.
Antipyretics are not useful in fever due to heat stroke; only external cooling
lowers body temperature.
3. Acute Rheumatic Fever
Aspirin is the first drug to be used in all
cases; other drugs are added or substituted only when it fails or in severe
cases (corticosteroids act faster). In a dose of 4–5 g or 75–100 mg/kg/day (in
divided portions producing steady state serum salicylate concentration 15–30
mg/dl) it brings about marked symptomatic relief in 1–3 days. Dose reduction
may be started after 4–7 days and maintenance doses (50 mg/kg/day) are
continued for 2–3 weeks or till signs of active disease (raised ESR) persist.
Withdrawal should be gradual over the next 2 weeks.
Granulomatous
lesions, nodules, cardiac complications, valvular defects, chorea and duration
of disease are not altered by salicylate therapy.
4. Rheumatoid Arthritis
Aspirin in a dose of 3–5 g/day is effective
in most cases; produces relief of pain, swelling and morning stiffness, but
progress of the disease process is not affected. Since large doses of aspirin
are poorly tolerated for long periods it is rarely used now; other NSAIDs are
preferred.
5. Osteoarthritis
It affords symptomatic relief only; may be used on ‘as and when required’
basis, but paracetamol is the first choice analgesic for most cases.
6. Post-Myocardial Infarction And Poststroke Patients
By inhibiting platelet aggregation aspirin lowers the incidence of reinfarction.
TXA2 synthesis in platelets is inhibited at low doses. It has been
argued that high doses can reverse the beneficial effects by concurrently
inhibiting PGI2 (antiaggregatory and vasodilatory) synthesis in
vessel wall. Large studies have demonstrated that aspirin 60–100 mg/day reduces
the incidence of myocardial infarction (MI): it is now routinely prescribed to
postinfarct patients; many recommend it for primary prophylaxis as well. ‘New
onset’ or ‘sudden worsening’ angina is associated with high infarction rate. This
can be reduced to half by 100–150 mg aspirin per day for 12 weeks.
Aspirin reduces
‘transient ischaemic attacks’ and lowers incidence of stroke in such patients.
But the risk of stroke in postMI patients is not reduced.
7. Other less well established uses of aspirin
are:
i.
Pregnancyinduced hypertension and preeclampsia:
imbalance between TXA2 and PGI2 is believed to be
involved: aspirin 80–100 mg/day benefits many cases by selectively suppressing
TXA2 production.
ii.
Patent ductus arteriosus: aspirin can bring about
closure and avoid surgery.
iii.
Familial colonic polyposis: aspirin and other
NSAIDs suppress polyp formation and afford symptomatic relief in this rare
disorder.
iv.
Prevention of colon cancer: incidence of colon
cancer among regular aspirin users is much lower. Colonic tumours express large
quantities of COX2. However, the rofecoxib trial (APPROVE) was prematurely
terminated and the drug withdrawn due to increased incidence of cardiovascular
events. The Adenoma Prevention with Celecoxib (APC) trial has also been
terminated due to 2.5 fold increase in risk of major fatal/nonfatal
cardiovascular events.
v.
To prevent flushing attending nicotinic acid
ingestion, which is due to PGD2 release in the skin.
ASPIRIN 350 mg tab,
COLSPRIN 100, 325, 650 mg tabs,
ECOSPRIN 75, 150, 325
mg tabs, DISPRIN 350 mg tab,
LOPRIN 75, 162.5 mg
tabs.
An injectable
preparation has been made available recently; BIOSPIRIN: Lysine
acetylsalicylate 900 mg + glycine 100 mg/vial for dissolving in 5 ml water and
i.v. injection.
Other salicylates
(salicylamide, benorylate, diflunisal) are seldom if ever used.
Related Topics
