Scale of the HCAI Problem-Prevalence and Incidence
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Public Health Microbiology: Infection Prevention And Control
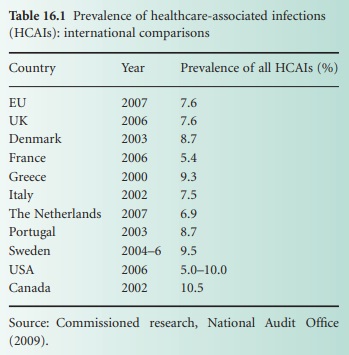
An assessment of the number of cases of HCAI and the risk of infection for different patient groups is based on a series of different measurements. Point prevalence studies have been undertaken in many countries to give a snapshot of the number, and the percentage, of patients with any type of HCAI in a particular healthcare setting on a specific day.
SCALE OF THE HCAI PROBLEM—PREVALENCE AND INCIDENCE
An assessment of the number of cases of
HCAI and the risk of infection for different patient groups is based on a
series of different measurements. Point prevalence studies have been undertaken
in many countries to give a snapshot of the number, and the percentage, of
patients with any type of HCAI in a particular healthcare setting on a specific
day. Prevalence studies in various developed countries over the last decade
have shown overall prevalence rates between 5% and 10% (Table 16.1). A
prevalence study in the four UK countries and the Republic of Ireland in 2006
showed an overall prevalence of 7.6%, ranging from 4.9% in the Republic of
Ireland to 8.2% in England. The low rates in the Republic of Ireland probably
reflected a rather younger patient population overall and the higher number in
England was linked almost entirely to much higher numbers of cases of CDI (2006
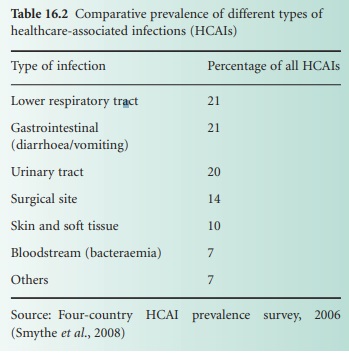
was the height of the epidemic of CDI in hospitals in England). The commonest
types of infection were urinary tract infection, followed by skin and soft
tissue infections and wound infections, respiratory infections, and gastro-intestinal
infections (Table 16.2).
Bloodstream infections accounted for only 7% of HCAIs but represent the most
severe end of the spectrum of disease. MRSA infections of all types accounted
for 16% of the HCAIs and CDI was 17% of the total in hospitals in England but
only 5% in Wales, Northern Ireland and the Republic of Ireland.
Prevalence studies provide valuable
comparisons between hospitals and countries and show the general contribution
of the various types of HCAI. However, they do not represent the actual number
of cases of different HCAIs over time, i.e. the incidence of infection in
different hospitals, wards or patient groups. For example, a point prevalence
of 8.2% does not mean that 8.2% of the patients admitted to the hospitals in
England developed an HCAI because the infected patients tend to be more
seriously ill and have longer stays in hospital both from their underlying
illness and as a result of their HCAI; therefore, the incidence is always less
than the point prevalence. Incidence is measured by ongoing and continued
surveillance of specific infections in which all cases of the infection are
recorded and related to the number of patients at risk. The HCAIs that are most
commonly subject to surveillance programmes are bacteraemias (bloodstream infections)
caused by specific healthcare-associated pathogens such as MRSA or
ESBL-producing E. coli (because they
represent the most severe types of HCAI), SSIs (one of the key indicators of
the quality of a surgical service or an individual surgeon), and CDI.
Surveillance data are necessary for monitoring infection prevention and control
activities at national and regional level, which can provide useful comparisons
between hospitals for patients who may choose where they wish to have their treatment.
However, surveillance with timely feedback and data is particularly important
at local level, within individual hospitals to ensure delivery of a high quality
of care. Most surveillance programmes have depended on voluntary reporting of
the infections to regional or national programmes but in several countries some
high-profilveillance programmes have been made mandatory to ensure that
infection prevention and control is made a high priority for health service
managers and clinicians alike. Mandatory surveillance of MRSA bacteraemia was
introduced in England in 2001, followed CDI, glycopeptide-resistant enterococcal
bacteraemia and SSIs in orthopaedic surgery in 2004. Similar approaches have
been applied in other UK countries, the Republic of Ireland, European countries
and the USA (mostly at an individual state level).
A further development of basic surveillance (i.e. reporting numbers of
cases) is the application of enhanced surveillance in which information about
patient demographics, risk factors, and outcomes is included. This can then be
linked to root cause analysis of individual cases to provide valuable
information about target areas for preventive measures.
What Has Surveillance Told Us?
Mandatory surveillance of MRSA bacteraemia in England showed a steady
rise in cases to a peak of 7700 in 2004. Public and political concern about
MRSA resulted in the government setting a target for a 50% reduction in MRSA
bacteraemia over the 3 years 2005–2008. The surveillance data enabled active
performance management through all levels of the (national) health service,
provided pressures for improved infection prevention and control actions, and
showed show the target was being achieved. Information from enhanced surveillance
within this programme showed the importance of patients’ ages and underlying
conditions as particular risk factors, and most significantly showed the
importance of intravenous catheters and cannulae, renal dialysis catheters,
urinary catheters and chronic wounds and ulcers as sites of MRSA infection
leading to bacteraemia.
A similar approach was taken with CDI when mandatory surveillance showed
that there were 55 000 cases in patients over 65 years of age in England in
2006; as these represent about 75% of cases, this means that there were around
70 000 cases overall. Guidance on prevention and control measures (based on the
1994 guidance) and a target to reduce the number of cases by 30% by 2011
focused activities in NHS hospitals and the 30% reduction was achieved within
the first year (2008–2009).
SSI surveillance in orthopaedic surgery has been a national requirement
in all UK countries for several years. This is a type of surgery with relatively
low rates of infection (<5%) but surveillance has focused attention on infective
complications, shown differences between surgical procedures, and also shown a
steady improvement in rates in all the countries. However, the very short
length of stay now usual for patients after these operations means that some
infections only manifest themselves when the patient is at home. This has shown
the need for including some system of post discharge surveillance for surgical
site infection to give a realistic picture of these HCAIs. This approach is
being pioneered in the UK and the Republic of Ireland in relation to infections
following caesarean section births where there is a clear opportunity for
professional input to post-discharge surveillance because the mothers are seen
at home by a midwife or health visitor.
The HCAI Challenge
The surveillance programmes in various countries have shown the scale of
the challenge set by HCAI in modern health and social care services. Why has
this situation developed? There is a strong argument that during the last quarter
of the 20th century, infections (including HCAI) had not been regarded as an
important part of modern medical practice. There had been a view from the late
1960s onwards that infectious diseases had been conquered and that antibiotics
and vaccines provided the answer. The importance of infection prevention and
control measures was not given its former position in clinical training of
doctors and nurses. Modern medicine was making tremendous progress in the
treatment of malignant diseases, cardiovascular disease, transplantation, and
chemotherapy, and in the management of chronic diseases. Life expectancy
increased markedly and the proportion of very elderly people in the population,
with their inevitable healthcare needs, rose rapidly. This created a vulnerable
patient population at high risk of infection, but these infections were
regarded as incidental nuisances rather than the major risk to a patients’
health and potential mortality which they are. Infections were regarded as the
province of the infection specialists (medical microbiologists, infection
control nurses) who had plenty of interesting work to do but a generally low
profile. The situation changed with the advent of the 21st century and the
recognition of the human and financial costs of HCAIs in a modern healthcare
service.
Related Topics
