Spinal Nerves
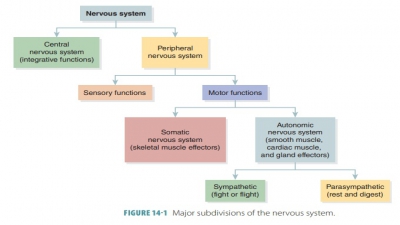
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Peripheral Nervous System and Reflex Activity
There are 31 pairs of spinal nerves originating from the spinal cord.
Spinal Nerves
There are 31 pairs of spinal nerves originating from the spinal cord. They are identified by their associa-tions with adjacent vertebrae. They are mixed nerves, allowing back and forth communication between the spinal cord and the upper limbs, lower limbs, neck, and trunk. Spinal nerves have both sensory and motor fibers. Spinal nerves are grouped according to the location from which they arise. As each spinal nerve passes through the intervertebral foramen, it is grouped with the vertebra above it. This is true for all spinal nerves except for those in the cervical area. There are eight pairs of cervical nerves (C1-C8), 12 pairs of thoracic nerves (T1-T12), five pairs of lumbar nerves (L1-L5), five pairs of sacral nerves (S1-S5), and one pair of coccygeal nerves (Coc 1). They are identified by increased numbering moving down the spine. The lumbar, sacral, and coccygeal nerves descend past the end of the spinal cord to form the cauda equina (horse’s tail). Spinal nerves from the sacral region of the cord innervate the leg muscles. Although there are eight pairs of cervical nerves, there are only seven cer-vical vertebrae. The first seven pairs exit the vertebral canal superior to the vertebrae for which they are named. However, C8 emerges inferior to the sev-enth cervical vertebra, which is between C7 and T1. Cervical spinal nerves innervate the muscles of the neck. Below the cervical area of the spine, the spinal nerves leave the vertebral column inferior to the vertebra that has the same number.
Spinal nerves are only 1–2 cm in length and divide just after emerging from each foramen.Each spinal nerve divides into a small dorsal ramus, a larger ventral ramus , and an extremely small meningeal branch. The meningeal branchreenters the vertebral canal, innervating the menin-ges and blood vessels that lie inside. Each ramus is mixed, similar to the actual spinal nerve. Rami communicantes contain visceral (autonomic) nerve fibers that attach to the base of the ventral rami or each thoracic spinal nerve.
Spinal Nerve Innervation
From the spinal nerves, the rami and their primary branches supply all the somatic region of the body from the neck down, which consists of the skin and skeletal muscles. The posterior body trunk is supplied by the dorsal rami and the remainder of the trunk and limbs are supplied by the thicker ventral rami. Rami differ from roots in several ways. Each root is either sensory or motor and lies medial to the spinal nerves, which they actually form. Rami carry both sensory and motor fibers and lie distal to the spinal nerves, from which they are laterally branched. All ventral rami (except for T2-T12) branch out, joining each other lateral to the vertebral column.
The main portions of the spinal nerves com-bine (except in the thoracic region) to form complex networks called plexuses. The ventral rami are the only rami that form plexuses. Recombined spinal nerve fibers innervate certain body parts, even though these fibers may originate from other spinal nerves. Each branch of a plexus formed from ventral rami contains fibers from several spinal nerves and fibers from the ventral rami, which travel to peripheral body portions via different routes. Every muscle in a spe-cific limb receives its nerve supply from several spinal nerves, not just a single nerve. Therefore, damage to one spinal root or segment does not totally paralyze a limb muscle.
Innervation of Specific Body Regions
The complete somatic region of the body, which includes the skeletal muscles and skin from the neck down, is supplied by the spinal nerve rami and their main branches. The posterior body trunk is supplied by the dorsal rami. The remainder of the trunk and the limbs are supplied by the thicker ventral rami. It is important to understand that roots lie medial to the spinal nerves, and also form them. Every root is either sensory or motor, not both. Rami lie distal to the spi-nal nerves and are their lateral branches. They also carry sensory and motor fibers.
All ventral rami, except for T1 to T 12, join each other lateral to the vertebral column. They form complex interlaced nerve networks known as nerve plexuses. These plexuses occur in the cervical, brachial, lumbar, and sacral areas. They mostly serve the limbs. However, only the ventral rami form plexuses.
Inside a plexus, the fibers from various ventral rami cross each other. They are redistributed and each branch of the plexus has fibers from several spi-nal nerves. The fibers from each ventral ramus travel to peripheral areas of the body, utilizing several paths. Therefore, every limb muscle receives a nerve supply from more than one spinal nerve. Damage to one spinal root or segment, therefore, will not totally paralyze any limb muscle.
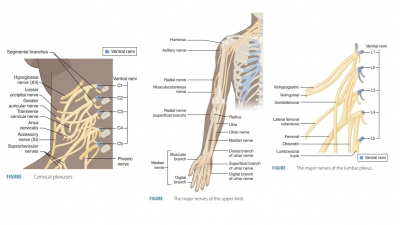
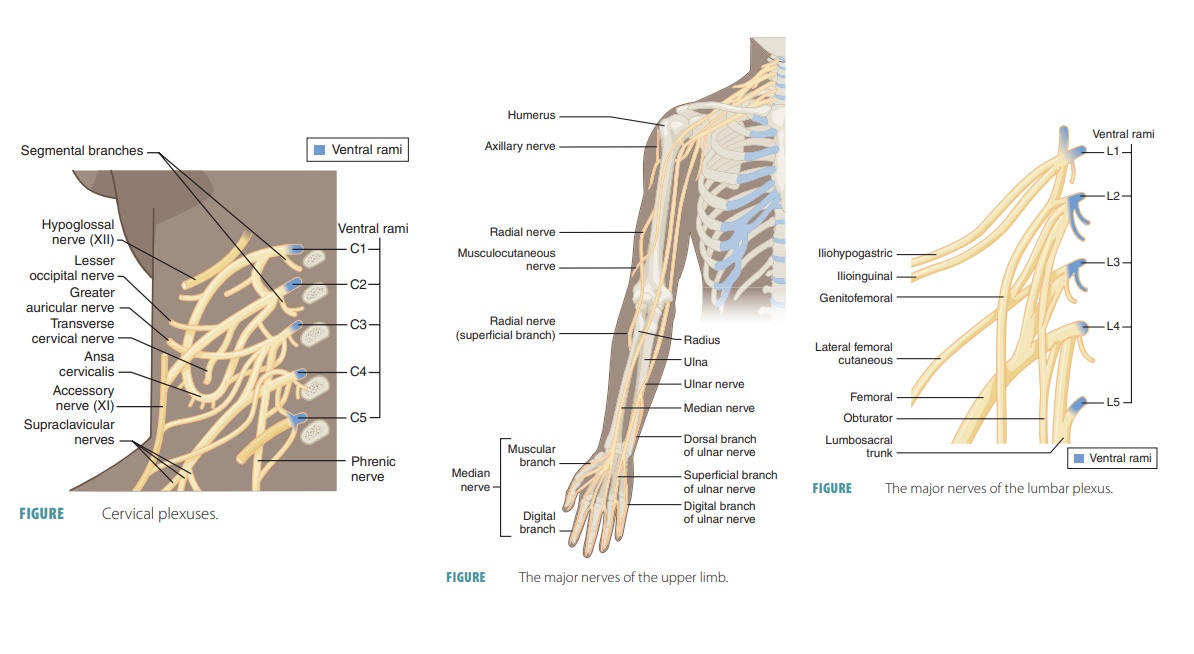
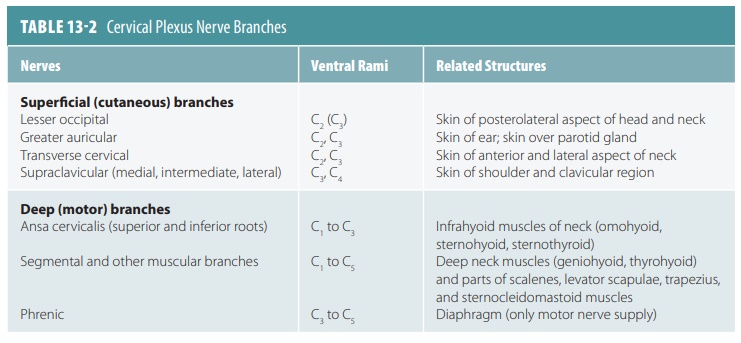
Cervical Plexuses
The cervical plexuses deep in the neck are formed from branches of the first four cervical nerves (FIGURE 13-4). Under the sternocleidomastoid muscle, a looped cervical plexus is formed from the ventral rami of the first four cervical nerves. Most branches of this plexus are cutaneous nerves supplying the skin alone ( TABLE 13 -2) . Sensory impulses are trans-mitted from the skin of the neck, ear region, posterior head, and shoulder. The anterior neck is innervated by other branches.
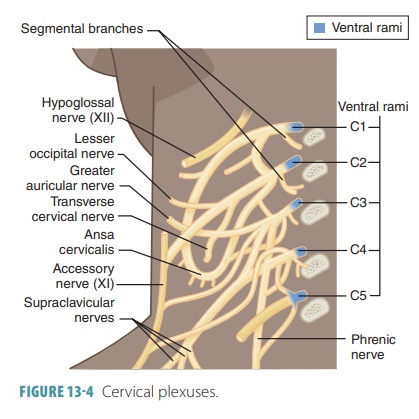
Fibers from the third, fourth, and fifth cer-vical nerves are combined into the right and left phrenic nerves, conducting motor impulses to the diaphragm. Each phrenic nerve runs inferiorly through the thorax, supplying sensory and motor fibers to the diaphragm, which is the most import-ant muscle that causes the movements required for breathing.
Brachial Plexuses
The ventral rami of cervical nerves C5 to T1 form the brachial plexuses, found in the shoulders between the neck and armpits. They supply the skin and mus-cles of the arms and hands, most importantly includ-ing the musculocutaneous, median, radial, ulnar, and axillary nerves. The brachial plexuses communicate with the sympathetic trunk and are composed of the anterior branches of the lower four cervical (C5-C8) and first two thoracic nerves (T1 and T2). Sometimes, C4 is also involved. The plexuses appear braided and allow sensory and motor axons from the spinal cord to cross and recross. The brachial plexus is a very complex struc-ture, basically made up of ventral rami, which form trunks, then divisions, and then cords. The three cords of the brachial plexus move along the axillary artery, where the main nerves of the upper limb originate (FIGURE 13- 5). The brachial plexus ends in the axilla. Trauma to a nerve of the brachial plexus may cause wrist drop.
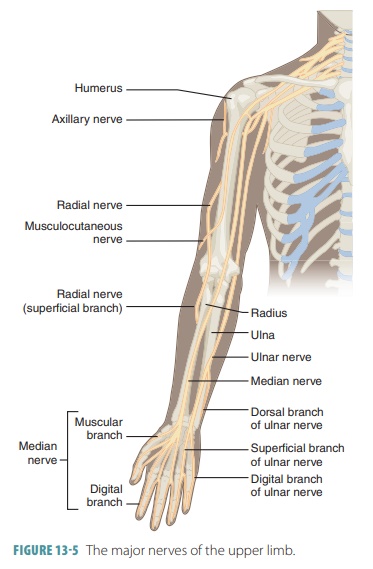
The axillary nerve branches from the poste-rior cord, running posteriorly to the surgical neck of the humerus. The musculocutaneous nerve is the major end branch of the lateral cord and runs inferiorly in the anterior arm. The median nerve runs down through the arm to the anterior forearm, branching off to the skin and most flexor muscles. The ulnar nerve branches off the medial cord of the bra-chial plexus to descend along the arm’s medial aspect to the elbow, behind the medial epicondyle, and along the ulna and medial forearm. The radial nerve is the largest branch of the brachial plexus and continues from the posterior cord. It wraps around the humerus, running anteriorly around the lateral epicondyle at the elbow, branching toward the radius and hand.
Lumbosacral Plexuses
The lumbosacral plexuses are made up of the last tho-racic nerve and the lumbar, sacral, and coccygeal nerves and extend into the pelvic cavity; they are associated with the skin and muscles of the lower abdominal wall, buttocks, external genitalia, thighs, legs, and feet. Their major branches include the femoral, obturator, and sciatic nerves. The lumbosacral plexuses are so named because of substantial overlap of the lumbar and sacral plexuses, with many lumbar plexus fibers combining with the sacral plexus through the lumbosacral trunk.
The lumbar plexuses are nervous plexuses in the lumbar region, formed by parts of the first four lumbar nerves and parts of the subcostal nerve. The nerves of the lumbar plexuses pass in front of the hip joints and mostly support the anterior muscles of the thighs. Each lumbar plexus lies within the psoas major muscle, branching proximally to innervate abdominal wall muscles and the psoas muscle itself. The major branches of the lumbar plexus descend to innervate the medial and anterior thigh (FIGURE 13-6).
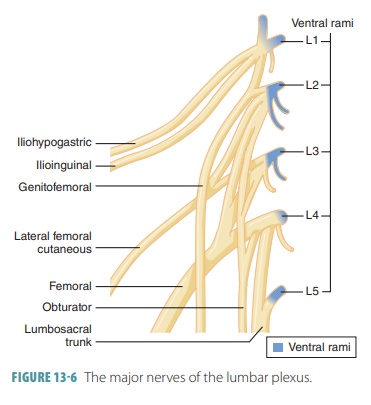
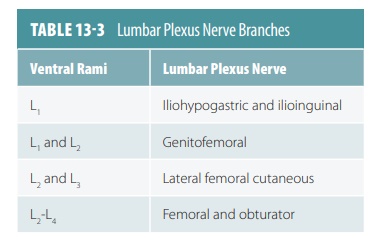
The largest terminal nerve of the lumbar plexus is the femoral nerve, which runs deep to the inguinal ligament. It enters the thigh, dividing into several large branches. Its motor branches innervate the quadriceps (anterior thigh muscles), which are vital for flexing the thigh and extending the knee. The cutaneous branches of the femoral nerve innervate the skin of the anterior thigh and the leg’s medial surface (from knee to foot). The obturator nerve enters the medial thigh through the obturator foramen, innervating the adductor mus-cles. The genitofemoral and saphenous nerves are also found in the lumbar plexus. TABLE 13-3 explains the branches of the lumbar plexus.
The sacral plexus lies immediately caudal to the lumbar plexus, arising from spinal nerves L4 to S4. It has approximately 12 named branches, half of which serve the buttocks and lower limbs. The remainder serves the structures of the pelvis and the perineum. TABLE 13-4 summarizes the largest branches of the sacral plexus.
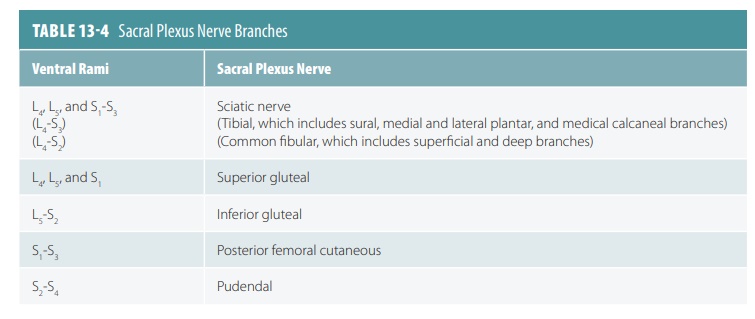
The sciatic nerve is the largest branch of the sacral plexus and is also the longest and thickest nerve in the entire body. It supplies all of each lower limb except the anteromedial thigh. The sciatic nerve is actually two nerves in a common sheath, called the tibial and common fibular nerves. The sciatic nerve moves from the pelvis, through the greater sciatic notch, deeply into the gluteus maximus muscle. It then enters the posterior thigh medial to the hip joint, with motor branches to the hamstring muscles and adductor magnus. In the hamstrings, it comprises all muscles that extend the thigh and flex the knee. Just above the knee, the tibial and common fibular nerves diverge into different directions.
The tibial nerve continues through the popli-teal fossa, posterior to the knee joint, supplying the posterior compartment muscles of the leg as well as the skin of the posterior calf and sole of the foot. The common fibular nerve (also called the common pero-neal nerve) descends to wrap around the neck of the fibula and divides into superficial and deep branches. The branches innervate the knee joint, skin of the leg (anterior and lateral), and dorsum of the foot. They also innervate the anterolateral leg, so its extensors can dorsiflex the foot.
Anterolateral Thorax and Abdominal Wall
The intercostal nerves are those made up of the ven-tral rami of T1 to T12. They mostly course anteriorly and are deep to each rib. The intercostal nerves supply the intercostal muscles, the skin and muscles of the anterolateral thorax, and the majority of the abdom-inal wall. Along their length, there are cutaneous branches to the skin. There are two thoracic nerves that are very different from the rest. Most of the fibers of the extremely small T1 nerve enter the brachial plexus. The T12 nerve lies inferior to the 12th rib, meaning that it is actually a subcostal nerve.
1. List the amounts of spinal nerves that originate in each of the five major divisions of the spinal cord.
2. Explain the distribution of fibers with a nerve plexus.
3. Explain the most important nerve of the cervical plexus.
4. List the five primary nerves of the brachial plexus and explain their locations.
5. Differentiate between the lumbar plexus and the sacral plexus.
Related Topics