The history of clinical pharmacy in the UK
| Home | | Hospital pharmacy |Chapter: Hospital pharmacy : Clinical pharmacy
Clinical pharmacy is now practised in all healthcare settings, but its main origins lie in the hospital sector. Until the mid-1960s, hospital pharmacists were mostly engaged in traditional pharmaceutical activities such as dispensing and manufacturing.
The history of clinical pharmacy in the UK
Clinical pharmacy is
now practised in all healthcare settings, but its main origins lie in the
hospital sector. Until the mid-1960s, hospital pharmacists were mostly engaged
in traditional pharmaceutical activities such as dispensing and manufacturing.
Then, the increasing range and sophistication of medicines available, awareness
of medication errors and the widespread use of ward-based prescription charts
brought pharmacists out of the dispensary and on to the wards in increasing
numbers.
This was initially
described as ‘ward pharmacy’ and was mostly a post hoc process with the
emphasis on the safe and timely supply of medicines in response to medical and
nursing demands. However, the service quickly evolved into something
significantly more proactive, seeing pharmacists inter-acting with patients and
other healthcare professionals and directly interven-ing in the patient care
process. The growth in these services over the 1970s and 1980s was said to
represent a change in hospital pharmacy from product orientation to patient
orientation and was formally acknowledged as ‘clinical pharmacy’ in the 1986
Nuffield report. The report welcomed these changes and recommended an increased
role for hospital pharmacists through the development of clinical pharmacy
services.
The recommendations
made in the Nuffield report were officially recog-nised in a 1988 Health
Services circular that outlined the main aims of the Department of Health with
respect to hospital pharmacy:
the achievement of better patient care and financial savings
through the more cost-effective use of medicines and improved use of
pharmaceutical services obtained by implementing a clinical pharmacy service.
A number of key
areas where pharmacist input could assist other clinicians and benefit patients
were highlighted, including contributing to prescribing decisions, monitoring
and modifying drug therapy, counselling patients and involvement in clinical
trials. The document acknowledged that, by helping to ensure patient safety and
appropriate use of medicines, clinical pharmacy services could prove to be
cost-effective.
As clinical pharmacy
services expanded, there was increasing specialisa-tion, with the expertise of
individual pharmacists in certain therapeutic areas contributing to more
significant developments in service provision. The speed of progress was
demonstrated in a review undertaken in the early 1990s, which showed that the
majority of NHS hospitals in the UK provided clinical pharmacy services and
most hospital pharmacists participated in ward-based clinical pharmacy activities.
However, the range of clinical pharmacy ser-vices varied enormously, from
almost 100% of hospitals having pharmacists who monitored drug therapy to less
than 10% for services such as infection control, clinical audit or medical
staff education. Since then, the widespread development of clinical pharmacy
services has continued, with significant expansion in the number and range of
services provided at most hospitals.
Wide variations in
the extent and nature of hospital clinical pharmacy services were also noted in
the Nuffield report and large differences still exist across much of the UK.
This lack of uniformity applies not just to clinical pharmacy, but also covers
almost every aspect of hospital pharmacy services. The absence of specific
directions from government and from the pharmacy profession, coupled with the
varying degrees of success with which individual pharmacy managers in each
hospital have been able to develop services, has allowed diversity to flourish
with wide variations in the proportion of time spent on clinical pharmacy
activities, ranging from less than 30% of pharma-cist time at some hospitals to
over 70% of pharmacist time at others. The Audit Commission recommended that
hospitals undertake reviews of their staffing levels and consider whether there
were adequate resources to provide all aspects of clinical pharmacy services,
so it is likely that the national figures on implementation of clinical
pharmacy services will be changing for some time.
One of the
differences between hospital and community pharmacy is the location of the
patient and how this affects the dynamics of providing clinical pharmacy
services. Most hospitals provide their pharmaceutical services to patients on
(but not exclusively) wards of various kinds. Thus, in order to deliver care
the pharmacist needs to visit the ward and interact with the patient, doctor,
nurse and others, as well as have access to consult and contribute to the
patient’s medical records.
Clinical pharmacist
presence on wards allows dialogue with patients and professionals in addition
to ensuring supplies of medicines are adequate for patients’ needs, and that
medicines are stored appropriately and safely. Pharmacy technicians, assistants
and others work with ward staff to provide effective supply of commonly used
items and, with the pharmacists, are increasingly leading the introduction of
the reuse of patients’ own drugs (PODs) schemes to reduce waste and, where
appropriate, patient self-medication to support concordance.
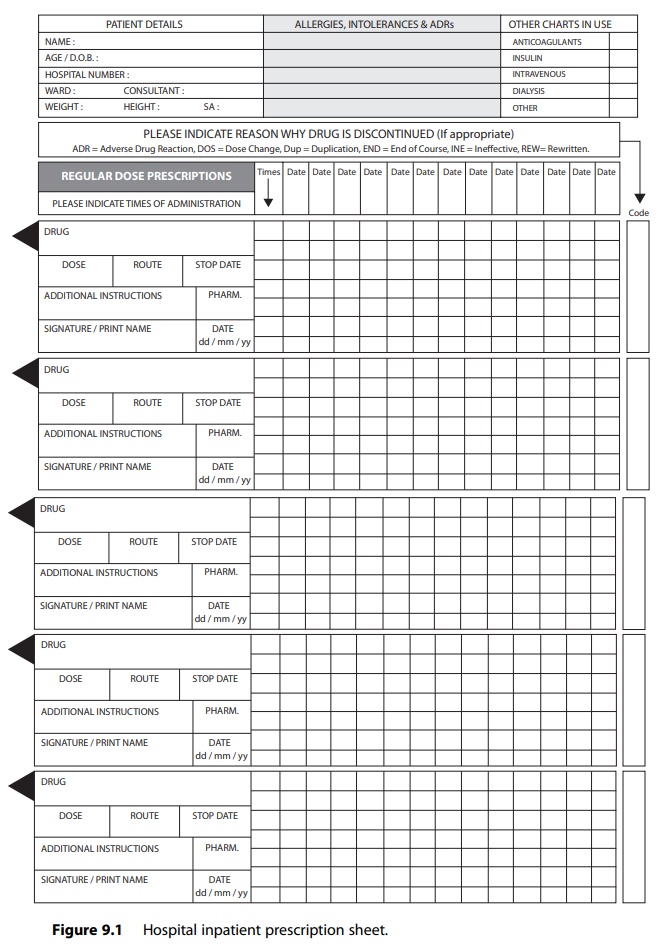
The importance of communicating
requests for medicines and the need to record administration of medicines have
led to the universal usage of the ward prescription chart. Various reports on
the value of recording the prescription and administration of medicines
emanated from situations where there was no record of them having been given.
Requiring nurses and doctors to record the administration of medicines offered
the rudiments of an audit trail for medicines.
The design and use
of these charts have consumed much time and energy from a variety of clinicians
in order to produce a hybrid document that serves the multiple purposes of
conveying: (1) patient details such as iden-tification, age, weight, gender and
allergies; (2) prescribing details such as medicine, form, dose, route and
frequency of administration and previous medicines; and (3) medicine
administration details including who adminis-tered (nurse, doctor, patient),
when and by which route. It also serves to indicate when a medicine has not
been given. An alert from the National Patient Safety Agency on reducing harm
from omitted and delayed medi-cines in hospital requires all healthcare
organisations to identify a list of critical medicines where timeliness of
administration is crucial.16 It also requires them to ensure that
medicine management procedures include guidance on the importance of
prescribing, supplying and administering critical medicines, timeliness issues
and what to do when a medicine has been omitted or delayed. Incident reports
should be regularly reviewed and an annual audit of omitted and delayed
critical medicines should be under-taken to ensure that system improvements to
reduce harms from omitted and delayed medicines are made. Figure 9.1 is an
extract from a typical hospital inpatient medicines chart.
The Welsh NHS took
this one step further in 2004 with the introduction of a new all-Wales
prescription chart, accompanied by prescription-writing standards and an
e-learning tool installed on the intranet systems of hospital trusts and
included in medical degree teaching.
The important sets
of prescription form data are essential for the efficient and effective
delivery of pharmaceutical care to the patient and also form the basis for the
development of electronic prescribing systems within the NHS. This is discussed
further in Chapter 15.
Related Topics
