Gastroesophageal reflux disease (GERD)
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs For Emesis, Reflux And Digestive Disorders
It is a very common problem presenting as ‘heartburn’, acid eructation, sensation of stomach contents coming back in food-pipe, especially after a large meal, aggravated by stooping or lying flat.
GASTROESOPHAGEAL REFLUX DISEASE (GERD)
It is a very common
problem presenting as ‘heartburn’, acid eructation, sensation of stomach
contents coming back in food-pipe, especially after a large meal, aggravated by
stooping or lying flat. Some cases have an anatomical defect (hiatus hernia)
but majority are only functional (LES relaxation in the absence of swallowing).
Repeated reflux of acid gastric contents into lower 1/3rd of
esophagus causes esophagitis, erosions, ulcers, pain on swallowing, dysphagia
strictures, and increases the risk of esophageal carcinoma.
The primary barrier to
reflux is the tone of LES which can be altered by several influences:
Inherent tone: of sphincteric smooth
muscle.
Hormonal: gastrin
increases, progesterone decreases (reflux is common in pregnancy).
Neurogenic:
vagus is motor to the sphincter, promotes esophageal peristalsis.
Dietary:
fats, alcohol, coffee, chocolates decrease, while protein rich foods increase LES tone.
Drugs: anticholinergics,
tricyclic antidepressants, Ca2+ channel blockers, nitrates reduce LES tone.
Smoking: relaxes
LES.
Delayed gastric
emptying and increased intragastric pressure may overcome the LES barrier to
reflux. GERD is a wide spectrum of conditions from occasional heartburn to
persistent incapacitating reflux which interferes with sleep and results in
esophageal, laryngotracheal and pulmonary complications. Severity of GERD may
be graded as:
Stage 1: occasional heartburn
(<3 episodes/week), mostly only in relation to a
precipitating factor, mild symptoms, no esophageal lesions.
Stage 2: > 3 episodes/week of moderately severe symptoms,
nocturnal awakening due to regurgitation, esophagitis present or absent.
Stage 3: Daily/chronic
symptoms, disturbed sleep, esophagitis/erosions/stricture,
symptoms recur soon after treatment stopped.
Though GERD is primarily a g.i. motility disorder, acidity of gastric
contents is the most important aggressive factor in causing symptoms and
esophageal lesions. The functional abnormality is persistent; dietary and other
lifestyle measures (light early dinner, raising head end of bed, weight
reduction and avoidance of precipitating factors) must be taken.
Treatment of GERD is individualized according to severity and
stage of the disorder.
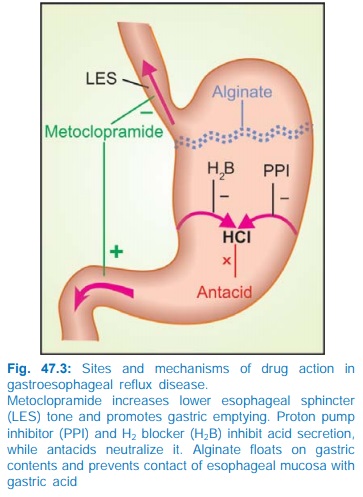
The site and mechanism of benefit afforded by different classes
of drugs in GERD is depicted in Fig. 47.3.
1. Proton Pump Inhibitors (PPIs)
These are the most effective drugs,
both for symptomatic relief as well as for healing of esophageal lesions.
Intragastric pH >4 maintained for ~18 hr/day is considered optimal for
healing of esophagitis. This level of acid suppression can be consistently
achieved only by PPIs. Therefore, PPIs are the drugs of choice for all stages
of GERD patients, particularly stage 2 and 3 cases. Symptom relief is rapid and
80–90% esophageal lesions heal in 4–8 weeks. Dose titration is needed according
to response in individual patients. Some patients require twice daily dosing.
Prolonged (often indefinite) therapy is required in chronic cases because
symptoms recur a few days after drug stoppage. PPIs have no effect on LES tone.
2. H2
Blockers
They reduce acidity of
gastric contents and have no
effect on LES tone. H2 blockers cause less complete acid suppression
than PPIs—adequate symptom relief is obtained only in mild cases; healing of
esophagitis may occur in 50–70% patients. H2 antagonists are indicated
in stage1 cases, or as alternative to PPIs in stage 2 or 3. The daily dose
should be divided into 2–3 portions for better response.
3. Antacids
Their use in GERD is
limited to occasional or
intercurrent relief of heartburn. Antacids are no longer employed for healing
of esophagitis.
4. Sodium Alginate
It forms a thick frothy
layer which floats on the
gastric contents like a raft may prevent contact of acid with esophageal
mucosa. It has no effect on LES tone. Combination of alginate with antacids may
be used in place of antacids alone, but real benefit is marginal.
REFLUX LIQUID: Sod.
alginate 200 mg + alum. hydrox. gel 300 mg + mag. trisilicate 125 mg/10 ml susp;
REFLUX FORTE Aginic acid 20 mg + sod. bicarb. 70 mg + alum. hydrox. 300 mg tab;
GAVISCON Alginic acid 500 mg + mag. trisilicate 25 mg + alum. hydrox. gel 100
mg + sod. bicarb. 170 mg tab.
5. Prokinetic
Drugs
Metoclopramide,
cisapride and other prokinetic
drugs may relieve regurgitation and heartburn by increasing LES tone, improving
esophageal clearance and facilitating gastric emptying, but do not affect gastric
acidity or promote healing of esophagitis. Symptom control afforded by
prokinetic drugs is inferior to that by PPIs/H2 blockers. Their use
in GERD has declined. Prokinetic drugs are occasionally added to PPI/H2
blocker therapy, but whether this improves outcome is not clear.
