Imbalances of the CNS
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Central Nervous System
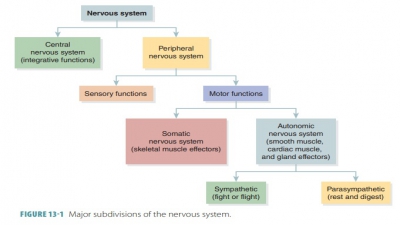
Brain dysfunctions are common and varied and may be caused by many different factors. This section focuses on brain trauma, cerebrovascular accidents, degenerative brain disorders, spinal cord trauma, poliomyelitis, and amyotrophic lateral sclerosis.
Imbalances of
the CNS
Brain dysfunctions are common and
varied and may be caused by many different factors. This section focuses on
brain trauma, cerebrovascular accidents, degenerative brain disorders, spinal
cord trauma, poliomyelitis, and amyotrophic lateral sclerosis.
Brain Trauma
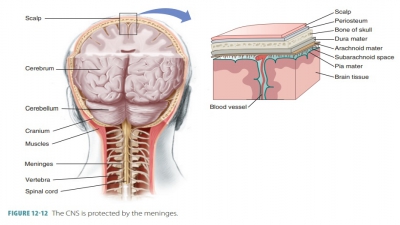
One of the leading causes of accidental death in the United States is head injury that results in brain trauma. In a car accident, for example, the brain is damaged by local injury at the site of the blow (the coup injury) and the reverse effect as the brain con-tacts the opposite end of the skull (the contrecoup injury). An alteration in brain function after a blow to the head, which is usually temporary, is called a concussion . Symptoms of a concussion include dizziness and loss of consciousness. Concussions, regardless of their severity, can damage the brain. If serious, the brain is bruised, resulting in permanent neurological damage. This is known as acontusion, which can range from the patient remaining con-scious to varying lengths of loss of consciousness. If the brain stem is contused, a coma develops that may last for hours or from which the patient will never awaken.
Brain trauma may also involve subdural hemorrhage or subarachnoid
hemorrhage. These occur when
blood vessels in one of these brain areas are ruptured. The patient is often
lucid at first after the trauma, but then develops neurolog-ical deterioration
due to the hemorrhage. Accumu-lating blood compresses brain tissue and
increases intracranial pressure. When the brain stem becomes forced inferiorly
through the foramen magnum, the patient’s blood pressure, respiration, and
heart rate become uncontrolled. Treatment of intracranial hemorrhage is via
surgery to remove the localized hematoma
(blood mass) and repair vessel ruptures. Traumatic head injury may also cause
swelling of the brain, called cerebral
edema, which can aggravate a brain
injury or even be fatal itself.
Cerebrovascular Accident (Stroke)
The most common nervous disorder
is a cerebrovas-cular accident, which is also called a
stroke or a brain attack. Strokes are the
third leading cause of death in North
America and occur when the brain’s blood cir-culation is blocked, causing the
death of brain tissue (FIGURE 12 -18). Deprivation of blood to a body tis-sue, called ischemia, impairs delivery of oxygen and nutrients. Strokes are usually
caused by blood clots that block cerebral arteries. The
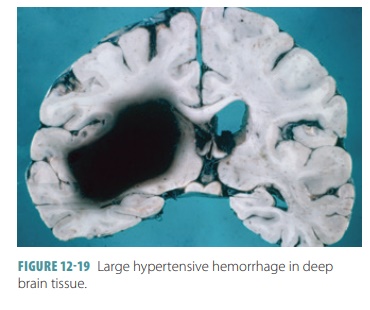
second most common cause is rupture of blood vessels in the brain, often due to
hypertension (FIGURE 12-19). Aneurysm is the third most common cause of stroke (FIGURE 12- 20).
Usually, the survivor of a cerebrovascular accident is paralyzed on one side of
the body (hemiplegia).

The most critical component of a
cerebrovascular accident is its long-term effect that often results in the
death of brain neurons. Neurons that are completely deprived of oxygen
disintegrate relatively quickly, releasing an overabundance of glutamate (an excit-atory
neurotransmitter).
In strokes, glutamate acts as an excitotoxin, which overexcites the
surrounding cells until they die. High levels of calcium ions damage
mitochondria of brain cells and initiate specific protein synthesis to cause
cell death via free radicals and inflammatory agents. Stroke treatments include
plasminogen activator to dissolve
blood clots and robotic surgery. New advancements include the use of stem cells
to replace damaged brain neurons. Temporary episodes of reversible cerebral
ischemia are known as transient
ischemic attacks. They last between five and 50
minutes, causing tempo-rary paralysis, numbness, or speech impairment.
Degeneration of the Brain
The three primary degenerative
brain disorders include Alzheimer’s
disease, Parkinson’s disease, and Huntington’s
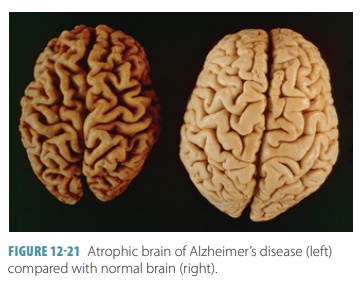
disease. Alzheimer’s
disease is a progressive disease that
eventually results in demen-tia (mental
deterioration). Up to 50% of people over age
85 die because of some Alzheimer-related factor. Symptoms include
disorientation, short attention span, and loss of language abilities. The brain
is over-come with senile plaques that form between neurons and neurofibrillary tangles inside the
neurons. The brain begins to shrink as its cells die (FIGURE 12 -21). This
primarily occurs in the basal forebrain and hippocampus. Glutamate
excitotoxicity is also involved in the progression of Alzheimer’s disease.
Parkinson’s
disease results from
degeneration of dopamine-releasing neurons in the substantia nigra, and
usually begins when a person is in his or her 50s or 60s. Symptoms include
“pill- rolling” hand movements, tremor of the hands at rest, a stony facial
expression, slowness in movements, a shuffling gait when walking, and a
forward-bending posture when walking. Although of unknown cause, Parkinson’s
disease may occur due to abnormalities in mito-chondrial proteins and their
degradation pathways. Treatments involve the medications elodea (L-dopa) and darnel, deep brain stimulation, gene
therapy, and stem cell implantation.
Huntington’s
disease usually develops
during middle age and is a fatal, hereditary disorder. Hun-tingtin proteins mutate and
accumulate, causing death of brain
tissue. The basal nuclei and cerebral cortex degenerate. Symptoms include
nearly continuous jerky movements (chorea),
which are involuntary, and even-tual severe mental deterioration. Huntington’s
disease is usually fatal within 15 years of symptom onset. This dis-order’s
symptoms oppose Parkinson’s disease because there is overstimulation of the
motor drive instead of inhibition. Treatments include medications to block the
effects of dopamine and stem cell implantation.
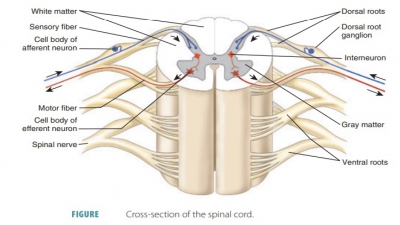
Spinal Cord Trauma
The spinal cord is able to
stretch extensively, yet direct pressure on it may cause serious loss of
function. Localized damage to either the cord itself or the spinal roots causes
either paralysis or paresthesias. Flaccid
paralysis of the skeletal muscles occurs
because of severe ventral root or ventral horn cell damage. Because nerve
impulses do not reach the skeletal muscles, they become unable to move
invol-untarily or voluntarily and atrophy because of lack of stimulation. Spastic paralysis occurs if just the
upper motor neurons of the primary motor cortex are dam-aged. This is because
the spinal motor neurons remain intact, with spinal reflex activity continuing
to irregu-larly stimulate the muscles. The muscles stay healthy for a longer
time but lose voluntary control. They may become permanently shortened as a
result.
If the spinal cord is cut in half
(transected), total motor and sensory loss occurs in body regions below the
site of the damage. For example, transection between the T 1 and L1
levels affects both lower limbs (paraplegia). If transection occurs in the cervical region, all four limbs are
affected (quadriplegia). Paralysis of one side of the body (hemiplegia) is usu-ally caused by brain injury and not spinal cord
injury.
Spinal shock is a collection of symptoms
caused by spinal cord transection.
There is a transient period of functional loss after injury and immediate
depression of all reflex activity that is caudal to the lesion site. All
muscles below the injury site become paralyzed and insensitive, blood pressure
is reduced, and reflexes of the bowel and bladder stop. Within a few hours
after injury, neural function usually returns. If this does not occur within 48
hours, paralysis is usually permanent.
Poliomyelitis
Poliomyelitis is defined as inflammation of the
gray matter of the spinal cord caused
by the poliovi-rus, which usually enters the body via water that is
contaminated with feces, destroying the ventral horn motor neurons. Symptoms of
poliomyelitis begin with headache, fever, muscle weakness and pain, and loss of
specific somatic reflexes. Paralysis
eventually develops, with affected muscles experiencing atrophy. Poliomy-elitis
may be fatal due to cardiac arrest or paralysis of the respiratory muscles. The
polio vaccines have nearly eradicated the disease worldwide.
The poliomyelitis epidemic of the 1940s and 1950s claimed many victims,
and many survivors are today experiencing postpolio
syndrome signified by sharp, burning muscular pain, extreme lethargy, and
pro-gressive muscle weakness and atrophy. Of unknown cause, postpolio syndrome
is believed to be related to continual loss of neurons, which occurs throughout
normal aging. A polio survivor may not have sufficient reserve neurons to
compensate for this loss over time.
Amyotrophic Lateral Sclerosis
Amyotrophic lateral sclerosis,
commonly referred to as Lou Gehrig’s disease, is a neuromuscular
condition that progressively destroys the ventral horn motor neurons and
pyramidal tract fibers, causing loss of the ability to swallow, speak, and
breathe. This condition is usually fatal within five years of onset. It is
caused by a combination of genetic and environmental factors. Mutations are
inherited in 10% of patients, with spon-taneous mutations probably occurring in
the remain-der. Recent advancements have localized the mutation to genes
involved in RNA processing. Excitotoxic cell death is probably involved because
of the presence of excess amounts of extracellular glutamate. The only
treatment that has prolonged the lives of amyotrophic lateral sclerosis
patients is the drug called riluzole,
which interferes with glutamate signaling.