Mechanisms of ADR-Causing Cytopenias
| Home | | Pharmacovigilance |Chapter: Pharmacovigilance: Gastrointestinal ADRs
A reduction, below the recognised reference range, in the numbers of any cell type in the peripheral blood must be because of either a reduction in the production of that particular cell type by the marrow (myelosup-pression) or a shortened survival of the cell type in the peripheral blood.
MECHANISMS OF ADR-CAUSING
CYTOPENIAS
A
reduction, below the recognised reference range, in the numbers of any cell
type in the peripheral blood must be because of either a reduction in the
production of that particular cell type by the marrow (myelosup-pression) or a
shortened survival of the cell type in the peripheral blood.
MYELOSUPPRESSION
Reduction
in marrow output as an ADR may be caused by a reduction in marrow cellularity
(hypopla-sia or aplasia, depending on severity). This may glob-ally affect all
cell lines [as in aplastic anaemia (AA)] or may selectively affect only one
lineage [e.g. pure red cell aplasia (PRCA)]. It may also be caused by
interference with normal maturation in a cellular marrow (dysplasia), as in
megaloblastic or sideroblas-tic anaemia.
CYTOTOXIC DRUGS
Most
cytotoxic drugs cause ‘type A’ myelosup-pressive ADR by interfering with DNA
synthesis or producing chemical damage to DNA that inter-feres with its
replication. Others attack the mitotic spindle, inhibit protein synthesis or
induce cell differentiation (Chabner and Wilson, 1995). Normal cells recover,
but it is not surprising that dose-limiting toxicity is seen in the marrow that
contains the most mitotically active normal cells in the body.
A
rare indirect cause of drug-induced myelosup-pression is the late development
of myelodysplasia or leukaemia because of genetic damage from previous exposure
to cytotoxic and other drugs (Le Beau et
al., 1986), but this is not considered further here.
OTHER DRUGS
Non-cytotoxic
drug effects causing acquired marrow failure are more difficult to establish.
Theoretical mechanisms include the induction of defects in the haemopoietic
stem cells, damage to the stromal microenvironment of the marrow, inhibition of
the production or release of haemopoietic growth factors or induction of humoral
or cellular immunosuppres-sion of marrow cells (Young and Maciejewski, 1997).
CONSTITUTIONAL RISK FACTORS
Susceptibility
to type A reactions varies between individuals because of differences in
absorption and metabolism of the drug (pharmacokinetic changes) or differences
in target organ sensitivity (Rawlins and Thomas, 1998). Some apparently
idiosyncratic type B reactions may actually become more appropriately
classified as predictable type A reactions for partic-ular individuals with
constitutional risk factors, once mechanisms are elucidated and tests to
identify those at risk become available.
The
antibiotic chloramphenicol was one of the first drugs for which epidemiological
evidence indi-cated a causal association with apparently idiosyn-cratic AA. An
early report of the coincidence of this very rare reaction in a pair of
identical twins suggested the possibility of genetic susceptibility (Nagao and
Mauer, 1969).
The
antipsychotic agent clozapine has an epidemio-logically established association
with agranulocytosis (Amsler et al.,
1977), which is considered further later in this chapter. An apparently
increased risk of this complication correlated with human leucocyte anti-gen
(HLA) phenotype (Dettling et al.,
2001). Anal-ysis of a cohort of patients from the Long Island Jewish Medical
Centre in New York (Lieberman et al.,
1990) found that the HLA-B38 phenotype had an incidence of 83% in patients with
agranulocytosis and 20% in clozapine-treated patients who did not develop the
complication. The B-38 phenotype was part of a haplotype more common in the
Ashkenazi Jewish population, and the subsequent work identified two different
haplotype associations with clozapine-induced agranulocytosis, one in Ashkenazi
Jewish patients and one in non-Jewish patients (Corzo et al., 1994). The association of both haplotypes with vari-ants of
the heat-shock protein-70 (HSP-70), encoded by loci within the major
histocompatibility complex (MHC) region, suggests linkage rather than direct
association of the HLA in genetic susceptibility (Corzo et al., 1995).
6-Mercaptopurine
(6-MP) is a thiopurine used extensively in the treatment of childhood acute
lymphoblastic leukaemia. Azathioprine is a pro-drug of 6-MP in widespread use
as an immunosuppres-sive agent in a variety of autoimmune conditions. 6-MP is
inactivated by the enzyme thiopurine methyl-transferase (TPMT). Genetically
determined varia-tions in TPMT activity were found to be associated with
occasional unexpectedly severe myelosuppres-sion associated with 6-MP (Evans et al., 1991) and azathioprine (Lennard,
Van Loon and Weinshilboum, 1989). The determination of TPMT activity, either by
the measurement of enzyme activity or by the molecular detection of the
polymorphisms associated with reduced activity, is feasible and could allow
avoidance of drug in deficient patients and logi-cal dose stratification in
heterozygotes. A pharma-coeconomic case has been made for this approach before
the use of azathioprine in dermatological prac-tice (Jackson, Hall and
McLelland, 1997). Polymerase chain reaction-based (PCR–based) techniques for
rele-vant genotypic analysis offer an attractive alternative to the performance
of radiochemical activity assays in pharmacogenetic screening (Coulthard et al., 2000).
Methotrexate
(MTX) is a dihydrofolate reductase inhibitor used extensively as a cytotoxic
agent in lymphoid and other malignancies and as an immuno-suppressive agent
particularly in inflammatory arthri-tis. Polymorphisms in the
methylenetetrahydrofolate (MTHFR)
gene have been associated with variation in efficacy and toxicity of MTX in
rheumatoid arthritis patients (Urano et
al., 2002).
These
examples suggest that technologies for predicting the risk of previously
apparently completely idiosyncratic reactions may become available for at least
some drugs that may help to reduce the incidence of these dangerous
complica-tions.
SHORTENED PERIPHERAL BLOOD CELL SURVIVAL
Shortened
survival of cells in the peripheral blood by ADR is most commonly mediated by
immune destruction. Antibodies to the drug itself, alone or as a hapten in
association with cell surface anti-gens or in immune complexes, may initiate
effec-tor mechanisms that damage cells. Alternatively autoantibodies may occur
because of altered immune regulation. Peripherally destructive immune
mech-anisms in ADRs more commonly only affect one cell type but may involve red
cells, granulocytes or platelets. A shortened red cell survival (haemoly-sis)
may also be mediated by oxidant stress, particu-larly in more susceptible
individuals [e.g. those with inherited glucose-6-phosphate dehydrogenase (G6PD)
deficiency]. Red cell and platelet survival may both be shortened by
endothelial damage causing inap-propriate intravascular plasma coagulation or
platelet aggregation in disseminated intravascular coagula-tion (DIC) and
thrombotic thrombocytopenic purpura (TTP), respectively.
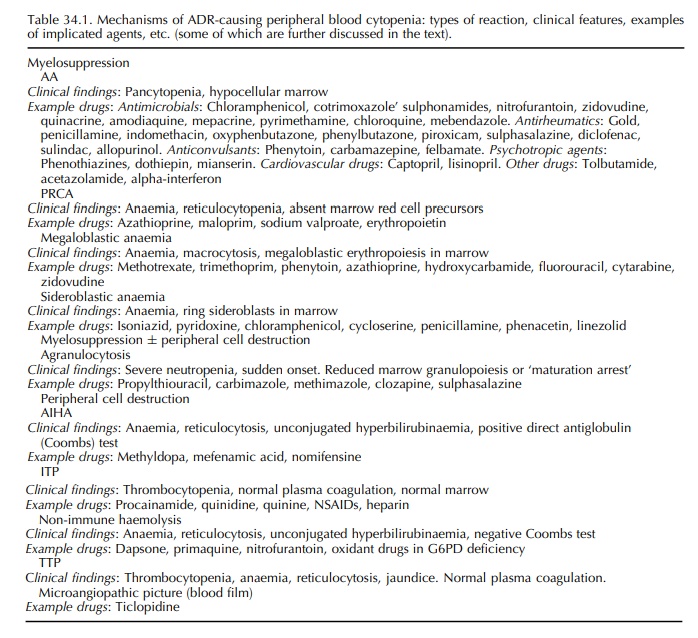
Table
34.1 lists mechanisms of cytopenias in ADR together with examples of implicated
agents.
Related Topics
