Miscellaneous Antibacterial Antibiotics
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Antibiotics And Synthetic Antimicrobial Agents: Their Properties And Uses
Miscellaneous Antibacterial Antibiotics, Chloramphenicol, Mupirocin, Fusidic acid, Antibiotics And Synthetic Antimicrobial Agents.
MISCELLANEOUS ANTIBACTERIAL
ANTIBIOTICS
CLINDAMYCIN
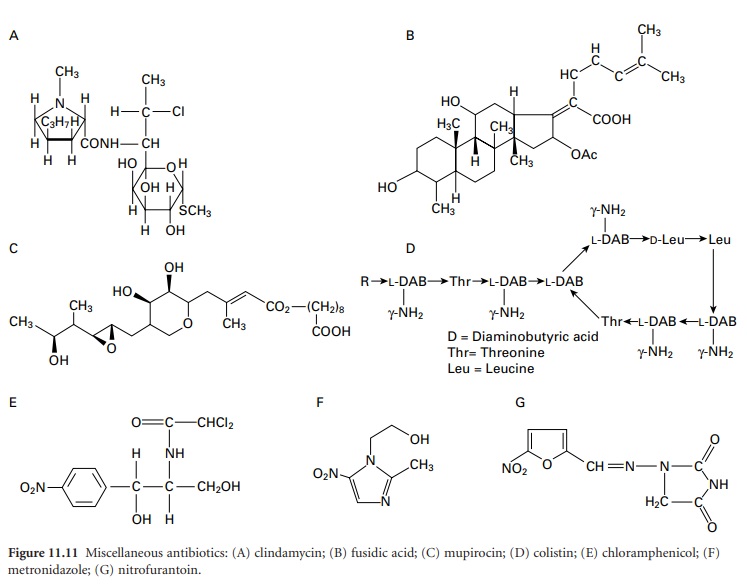
Clindamycin (Figure
11.11A) is another antibiotic possessing significant bacteristatic activity towards Gram-positive cocci
(including MRSA, but not Ent. faecalis), although rather less
activity is shown towards Gram-negative cocci and none at all against
enterobacteria. Clindamycin is not related
structurally to the macrolides (section 4) but has a similar
mechanism of action, so cross-resistance may occur between them. The
streptogramins also
have a similar
mechanism of action,
but it is
claimed that the quinupristin-dalfopristin combination does not demonstrate
cross-resistance to clindamycin or the macrolide antibiotics.
Clindamycin is currently recommended for the oral treatment of staphylococcal bone and joint
infections, acne, peritonitis, infections by anaerobic
bacteria and falciparum malaria. Together
with oral cephalosporins, it is one of the antibiotics most
firmly associated with
pseudomembranous colitis caused by Cl. difficile, and this reputation limits its use.
FUSIDIC ACID
Fusidic acid (Figure 11.11B)
is a steroid-like, bactericidal
antibiotic used primarily for its activity
against staphylococci. It does possess
activity against other Gram-positive
species, although streptococci are relatively resistant and Gram-negative bacilli
completely so. It is active
against penicillin-resistant strains of Staph. aureus, including MRSA, and may be administered in
combination with erythromycin or clindamycin for severe staphylococcal infections. Fusidic
acid is available
as a paediatric oral
suspension, cream and ointment, and,
in the form of its water-soluble sodium salt, as tablets or an intravenous injection. Resistance arises with relative
ease in vitro, but despite this, resistance is relatively uncommon
in clinical isolates.
MUPIROCIN
Mupirocin (Figure
11.11C) is an antibiotic active against
staphylococci, streptococci and a limited range of Gramnegative species. Its use is largely confined to topical treatment of Staph. aureus infections, particularly the
eradication of MRSA from the nose; for this purpose
it is claimed normally
to be more effective than chlorhexidine or fusidic acid.
COLISTIN
Colistin (Figure
11.11D) is the only member
of the polymyxin group of peptide antibiotics that is still
in use. It is active against
many types of Gram-negative bacteria, but not against cocci,
Serratia marcescens and Proteus
spp.; it is inactive against
Gram-positive organisms. Its use is largely
restricted to the treatment of Ps. aeruginosa
lung infections in cystic fibrosis
sufferers, in which
case it is nebulized
or given by intravenous injection, and in the treatment of infections, particularly in burns, caused by Acinetobacter species.
CHLORAMPHENICOL
Chloramphenicol (Figure
11.11E) is a true antibiotic but is manufactured totally by chemical
synthesis. It has a
broad spectrum
of activity including some rickettsias and larger viruses, but aplastic anaemia, which is dose-related
may result from
treatment in a proportion of patients
and this has largely
restricted its use as a systemic antibiotic to life-threatening infections with H. influenzae. It is,
however, still used significantly in the treatment of ophthalmic infections and in veterinary medicine.
METRONIDAZOLE AND OTHER NITROIMIDAZOLES
The nitroimidazoles are a group
of synthetic antimicrobials that are unusual
in possessing activity
against a wide range of organisms including bacteria,
protozoa, and some helminths. They
are similar in terms of their structure, mode of action,
uses and toxicity and the principal factor distinguishing them is
their pharmacokinetics. Metronidazole (Figure
11.11F) is by far the most commonly used, and
is the only one considered in this section, although nimorazole (no
longer available in the UK) and
tinidazole are alternative drugs that may afford the advantage of less frequent dosing.
They may all be regarded as prodrugs in the sense
that they become
active only after
reduction of the nitro group
in low redox
environments, so they
are able to kill cells
growing anaerobically by damaging
their DNA. This damage could,
in theory, occur in any type of cell regardless of its taxonomic status, and the fact that sufficiently reducing conditions do not arise in mammalian cells
is the reason
for the drugs’
lack of toxicity for humans.
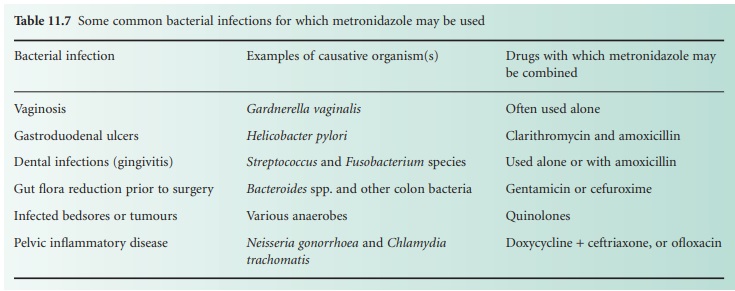
Metronidazole was introduced in 1960 for the treatment of vaginitis caused by the protozoan Trichmonas vaginalis, and its wider application for the treatment of bacterial anaerobic infections was recognized later. Currently metronidazole is used alone, or quite commonly in combination with other antibiotics, for the treatment of a wide variety of bacterial infections shown in Table 11.7. For the treatment of amoebiasis, giardiasis or trichomonal vaginitis, metronidazole is often used alone. Metronidazole is available in more dosage forms (oral, topical, injectable or suppositories) than most other antibiotics, and by the oral route is often given two or three times daily. Toxicity and side effects are relatively uncommon, although it does exhibit a disulphiram-like reaction with alcohol in some patients.
NITROFURANTOIN
Nitrofurantoin (Figure 11.11G) is the one remaining member of the nitrofuran group of drugs that is still in common use. Like metronidazole, nitrofurantoin requires its nitro group to be reduced in order to exhibit anti-microbial activity, and it too exhibits bactericidal activity by damaging DNA. It has a wide spectrum of activity which includes Gram-positive cocci and many Gram-negative enteric bacteria, but after oral administration the blood levels achieved are very low and a significant fraction of the dose is rapidly excreted in the urine, so its use is restricted to the treatment of cystitis. The size of the drug crystals used in tablet manufacture has an effect on the dissolution of the drug, and it is claimed that the macrocrystalline form affords steadier release. Its antimicrobial activity is substantially greater in acid urine, which unfortunately conflicts with the common symptomatic treatment of cystitis by alkalizing the urine with potassium citrate or similar compounds. Nitrofurantoin is unusual in being one of the few antimicrobial drugs to which resistance has not significantly increased since its introduction, and for this reason there is a degree of renewed interest in it.
Related Topics
