Quinolones
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Antibiotics And Synthetic Antimicrobial Agents: Their Properties And Uses
The quinolones and the cephalosporins have much in common in terms of their history and development: both classes of antibiotic were first introduced in the early 1960s and the first members of each class, nalidixic acid and cephalothin respectively, had limited applications.
QUINOLONES
The quinolones and the cephalosporins have much in
common in terms of their
history and development: both classes of antibiotic were first introduced in the early 1960s and the first members
of each class,
nalidixic acid and cephalothin
respectively, had limited applications. However, both groups were extensively developed over the next 50
years with four generations of antibiotics being produced in both classes,
each an improvement on its predecessor, so that the quinolones and the cephalosporins are currently amongst
the most widely used
and valuable antibiotics available.
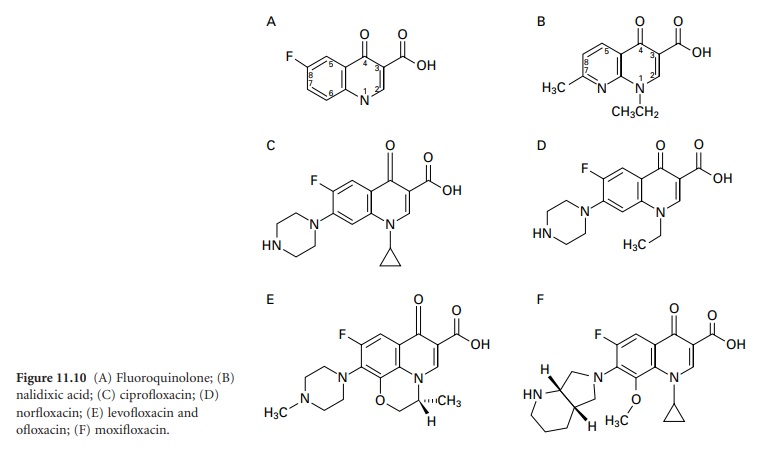
Nalidixic acid (Figure 11.10B)
was developed as a
treatment for urinary tract infections, and it, together with other first-generation quinolones produced in the 1960s and 1970s (e.g.
cinoxacin, acrosoxacin and pipemidic acid), had an antibacterial spectrum that was largely restricted to E. coli and other Enterobacteriaceae.
As with the cephalosporins, there
is no universal acceptance of the
definitions of each
generation of the
antibiotics, so particular quinolones have been assigned
to different generations in various textbooks. There is agreement, however, that the distinguishing feature of the first
generation is the absence
of a fluorine atom at position
6, so they are simply designated ‘quinolones’, whereas
the second, third
and fourth generations are termed fluoroquinolones. The first-generation
drugs are now little used, but those that followed
in the 1980s, e.g. ciprofloxacin, norfloxacin, ofloxacin and
levofloxacin (the L-isomer of ofloxacin) (Figure 11.10C–E), are still very much in use today
and owe their
popularity both to their
greater activity against
E. coli and other
Gram-negative urinary pathogens and their wider
antibacterial spectrum which
includes Gram-positive cocci and Ps.
aeruginosa. The
third-generation quinolones, e.g. moxifloxacin (Figure 11.10F), possess
the attributes of their predecessors but exhibit
greater activity against
Strep. pneumoniae. The fourth generation, e.g. trovafloxacin
(not available in Europe), are
also active against
anaerobes.
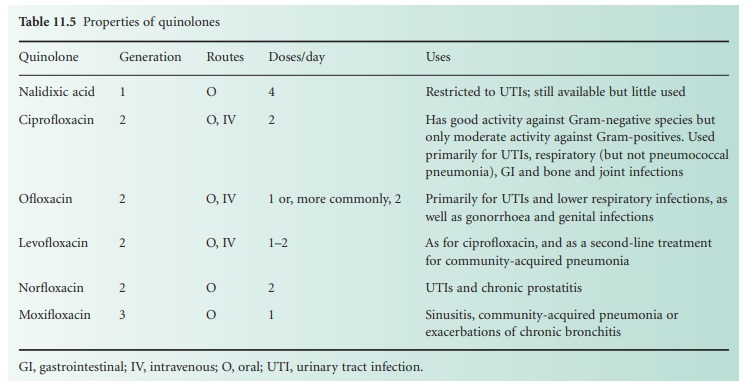
All the quinolones are bactericidal, and act by inhibiting the bacterial enzymes responsible for coiling of DNA; they are all orally active, and several are available as intravenous injections. The first-generation drugs were only used for the treatment of urinary infections, but the much broader spectra of those that followed permitted their use for respiratory, soft tissue, bone and joint, gastrointestinal and sexually transmitted infections as well. Quinolones have been shown to cause rare cases of tendon damage, including rupture, and for this reason are not generally prescribed for children, but their most common minor side effect is gastrointestinal disturbances, which are reported in about 5% of patients. They are relatively susceptible to resistance development, and Gram-positive species tend to mutate to resistance at higher frequencies than Gram-negatives. Some degree of cross-resistance usually occurs, so that bacteria that become resistant to one quinolone are often less susceptible to others. They are now the most widely prescribed antibiotics for adults in the USA, and the growing resistance problem has been attributed in part to their indiscriminate use in human medicine and to cross-resistance between the drugs used for human infections and the several quinolones licensed exclusively for veterinary medicine which have been overused, particularly in Europe, for prophylaxis of bacterial infections in poultry flocks and other intensively reared animals. The characteristics of some of the important quinolones are shown in Table 11.5.
Related Topics
