Non-sterile manufacture
| Home | | Hospital pharmacy |Chapter: Hospital pharmacy : Technical services
The manufacture of traditional non-sterile oral liquids and topical prep-arations, usually in accordance with British Pharmaceutical Codex formulae, has declined in the hospital sector over recent years.
Non-sterile manufacture
Scope
The manufacture of
traditional non-sterile oral liquids and topical prep-arations, usually in
accordance with British Pharmaceutical Codex formulae, has declined in the
hospital sector over recent years. This is largely due to the commercial
availability of licensed products and also the growth of non-sterile specials
manufacturing services operated commercially. How-ever, a non-sterile
production service is still required to support several clinical specialties,
particularly dermatology and paediatric. Many dermatol-ogists have their own
variants of standard preparations, often differing only in the type of diluents
or base used or in the concentration of active components. Although there is
little scientific evidence to support the use of these non-standard
preparations, custom, practice and clinical experience have, until recently,
provided a continuing demand. Attempts are being made to reduce the range of
products used to allow standardisation and simplification. The British
Association of Dermatologists’ preferred list was issued in 2008 to support
this approach.
Conversely, the
clinical justification for using medicines outside their licensed indications
for adults in the paediatric setting is well accepted. The unit dose of
commercially available preparations of medicines designed for adult use is
usually too large for paediatrics. Also, some of the larger tablets and
capsules would be difficult for children to swallow. Safe and reproducible
paediatric dosing therefore requires preparations of lower dose, usually in the
form of oral liquids, suspensions or powders.
Department of Health
information reported in 2002 suggested that dermatology preparations (coal tar,
salicylic acid and dithranol) were the most frequently prepared non-sterile
products by hospital pharmacy depart-ments, although in recent years most of
these preparations have become commercially available. Some hospitals have
developed commercial non-sterile manufacturing units to supply other hospitals
and community phar-macies. This type of activity helps to offset the costs of
maintaining facilities of a high standard and meeting the regulatory
requirements of MHRA specials licences.
In some hospitals,
dispensary services have been reorganised and extem-poraneous dispensing work
has been transferred to the technical services section. A wide range of
non-commercially available extemporaneous prep-arations is required for
individual patients, including oral liquids, creams, ointments, powders,
suppositories and pessaries. This approach provides variety and clinical
interest for manufacturing staff and ensures that extem-poraneous products are
produced in accordance with the principles of good manufacturing practice.
Facilities and equipment
Typically, non-sterile
manufacture is carried out in a European Union (EU) grade D environment with a
single stage change. Although some units require production staff to wear
sterilised coverall gowns, most centres rely on clean two-piece gowns of
low-lint-shedding material, over-shoes, hats and gloves. To reduce the
microbiological bioburden, drains and potable water supplies are excluded from
production areas and all surfaces should have a smooth impervious finish to
facilitate effective cleaning. Weighing areas should be separate from the main
production area (linked to it with a pass-through hatch) and should be fitted
with localised dust extraction. Although containers for non-sterile products
are not reused, a facility for washing and drying containers before use may be
required. Separate areas should be provided for labelling and reinspection of
products.
The Rules and
Guidance for Good Pharmaceutical Manufacture and Distribution strongly
recommend the use of stainless-steel measures and mixing vessels to avoid the
risk of contaminating product with spicules from glass equipment.8
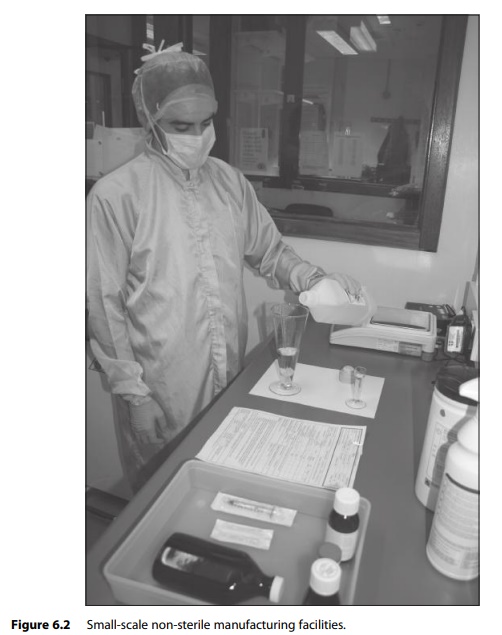
Large-scale manufacture will require the use of industrial mixers and
homogenisers. Automated liquid filling lines may be deployed for large-scale
liquid handling and some units with a significant output of creams and
ointments have also invested in tube-filling and seal-ing equipment. Figure 6.2
illustrates small-scale non-sterile manufacturing facilities.
Process
All raw materials,
containers and labels used in the production process must be approved by the
person responsible for QC. To reduce the micro-biological bioburden, limits are
placed on the level of microbiological contamination of raw materials and only
sterile water (usually water for irrigation BP) or freshly distilled water is
used for manufacture. All prod-uct formulae, storage conditions and shelf-life
assignments require prior QC approval.
The manufacturing
process is controlled through the use of approved standard operating procedures
and batch documents. Particular care is re-quired to ensure that mixing
processes produce a homogeneous product for distribution into the individual
containers that constitute the batch. This process must be validated for each
product type to ensure uniformity of content in the finished batch. The
avoidance of cross-contamination between different products is also essential.
Only one batch may be prepared in a designated work area at any one time and
the cleaning of equipment and work surfaces must be carefully validated and
monitored.
Filled containers
should be visually inspected for product homogeneity and the absence of any
extraneous matter. The security of container closures should be checked and the
quality and accuracy of labels determined against a master label for the
product. It is essential that the batch documentation includes reconciliation
between the amounts of raw materials, number of containers and number of labels
used in the process and the yield of finished product. All variations must be
recorded and investigated.
Although some
regulators have attempted to discourage non-sterile manufacturing in hospital
pharmacies, there are compelling reasons why sufficient capacity in this
activity is retained. The ongoing need for paedi-atric doses of both new and
existing medicines that are commercially avail-able in adult doses must be
recognised. There is also a requirement to formulate medicines for patients
with particular clinical needs, such as patients with dysphagia. It is
preferable for these medicines to be produced by trained pharmacy staff in
appropriate facilities, using fully documented procedures, than to have
undocumented manipulation taking place in clinical areas by nursing staff.
