Sterile manufacture
| Home | | Hospital pharmacy |Chapter: Hospital pharmacy : Technical services
All terminally sterilised medicines produced in hospitals are made under a manufacturer’s specials licence, except in a few cases where PLs have been obtained.
Sterile manufacture
Scope
All terminally
sterilised medicines produced in hospitals are made under a manufacturer’s
specials licence, except in a few cases where PLs have been obtained. The range
of products made generally reflects gaps in the portfolio of licensed products
available from the pharmaceutical industry. The limited number of specialist
sterile manufacturing units remaining in the NHS pro-vides an essential service
in making available sterile parenteral and topical products that are not
commercially viable for industry to produce. Such products include non-standard
concentrations and presentations of injections and eye drops, specialist
injectables for paediatrics, anaesthetics and palliative care, and various
sterile topical products.
In some cases, NHS
hospital sterile product units have developed prod-ucts to support pharmacy
CIVAS units. These include electrolytes for addition to TPN feeds such as
concentrated sodium chloride injection, potassium phosphate injection and zinc
sulphate injection. A range of sterile bulk solutions for filling into syringes
and other devices is also produced. These include bupivacaine injection,
morphine sulphate injec-tion and fentanyl injection. Sterile manufacture also
supports research, and small runs of experimental drugs in parenteral
formulations are prepared for clinical trial use.
The container and
filling technologies employed in hospital units encom-pass glass vials, glass
ampoules, glass bottles and polyvinyl chloride infusion bags for parenteral
products, and a variety of glass and rigid plastic containers for topical
solutions. No lyophilised presentations are available since freeze-drying
technology is beyond the scope of hospital sterile product units.
Facilities and equipment
In general, the
weighing and solution preparation areas required would be similar to those
described previously for non-sterile manufacture. However, the filling, sealing
and capping stages must be accomplished in a higher-quality environment,
usually EU grade A, to minimise particu-late contamination and reduce the
microbiological load prior to sterilisa-tion. This is usually achieved by local
laminar flow of high-efficiency particulate air-filtered air at the filling
zone. After filling and sealing, containers and their contents are sterilised
by steam in an autoclave (aque-ous solutions) or by dry heat in a hot-air oven
(non-aqueous liquids, powders). The sterilisers and associated monitoring
equipment can be located in a lower-grade environment and are normally sited so
that maintenance staff can access them without the need to enter critical
pro-duction areas.
Dedicated space for
reinspection of the finished product, labelling, pack-ing and quarantine is
also required. Regulatory requirements for sterile pro-duction facilities and
sterilising equipment are strictly defined and require extensive validation.
The design and construction of sterile manufacturing units should only be
undertaken by specialist contractors. The increasing use of automated systems,
particularly for filling, sealing and reinspecting ampoules, and the
sophistication of modern steriliser technology have con-tributed to the rapid
rise in capital and maintenance costs associated with sterile manufacturing
units. National coordination and strategic planning of new units are essential
to maximise the cost-effectiveness of these expensive but important resources.
Process
In addition to the
processes outlined under non-sterile manufacture, above, sterile production
normally includes a filtration process (for liquids) and sterilisation of the
product. These processes are critical to product quality and require rigorous
validation and control. The microbiological bioburden must be minimised,
particularly in the case of injectables, to reduce the release of bacterial
pyrogens into the product, because these will not be destroyed by
sterilisation. This is achieved by limiting the number of viable microorganisms
in starting materials and by minimising the time between preparations of the
bulk product, filling and sterilisation.
The sterilisation
cycle for each batch is clearly monitored to ensure that all containers in the
batch have received the pharmacopoeial-approved temper-ature and time
combinations. Printouts of the load temperature, usually taken at the coolest
location of the autoclave or dry-heat oven, are recorded throughout the cycle
and are scrutinised as part of the release process. Additional measures are
taken to ensure that products sterilised by autoclave or hot-air oven are not
at risk from microbial contamination of cooling water or non-sterile air,
respectively, which could enter through closures during the cooling phase of
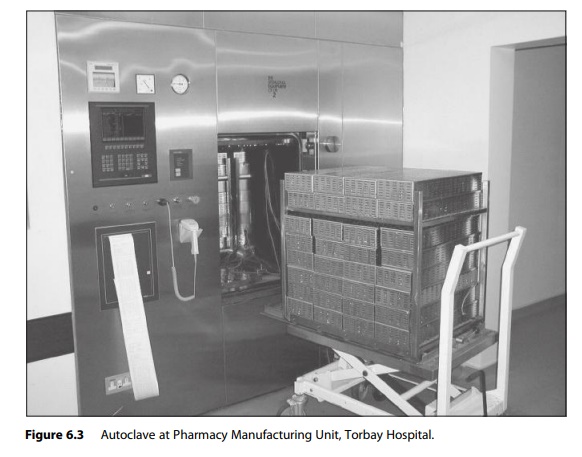
the cycle. Figure 6.3 shows an autoclave and its control systems in a large
sterile production unit.
The QC of sterile products includes analysis of active components, sterility testing, subvisual particulate measurement and tests for the absence of bac-terial pyrogens. This means that batches must be quarantined for at least 14 days (the time taken for sterility test incubation) before release. Production managers and users of sterile products need to consider this when drawing up production schedules and managing stocks.
