Tissue Membranes
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Levels of Organization : Tissues
Tissue membranes form a barrier or an interface. There are many different types of anatomical membranes. Epithelial membranes are thin structures made up of epithelium and underlying connective tissue. They cover body surfaces and line body cavities. There are four types of membranes: serous, mucous, cutaneous, and synovial.
Tissue
Membranes
Tissue membranes form a barrier
or an interface. There are many different types of anatomical membranes. Epithelial membranes are thin
structures made up of epithelium and underlying connective tis-sue. They cover
body surfaces and line body cavities. There are four types of membranes:
serous, mucous, cutaneous, and synovial.
1. serous
2. mucous
3. cutaneous
4. synovial
Serous Membranes
Serous
membranes line body cavities
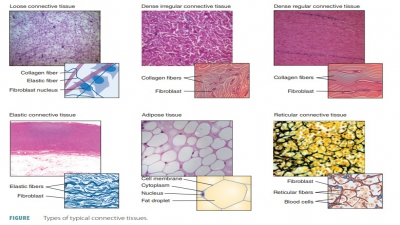
that lack openings to the outside of the body. They consist of simple
squamous epithelium (a mesothelium) and loose connective (areolar) tissue and
secrete watery serous fluid, which lubricates membrane surfaces. Serous fluid
contains enzymes. The serous membranes are extremely thin, yet firmly attached
to body walls and to organs that they cover. Every serous membrane is divided
into the parietal por-tion, lining
the inner surface of a body cavity, and an
opposing, moist visceral portion
or serosa, covering the visceral organs.
The mesothelium cells mix
hyaluronic acid with a fluid from the capillaries of related connective tissue
to produce thin, clear serous fluid
or transu-date. This lubricates opposing
surfaces of the vis-ceral and parietal layers so they can slide across each
other with ease. The total amount of transudate in a healthy individual is very
small. However, after an injury or due to certain diseases, its volume may
increase greatly, resulting in medical complications or even causing new
conditions to develop. The sero-sae are
named for their locations. Examples include
the pericardium (which encloses
the heart), perito-neum (which
encloses the abdominopelvic viscera), and
the pleurae (which line the thoracic
wall and cover the lungs) . One example of serous glands is the parotid
salivary glands.
Mucous Membranes
Mucous
membranes are also known as mucosae. These membranes line body cavities that open to the outside
of the body, including the nose and mouth as well as digestive, respiratory,
urinary, and repro-ductive tubes. Mucous membranes consist of epithe-lium above
the loose connective tissue (the lamina
propria), with goblet cells that
secrete mucus. In some mucosae, the
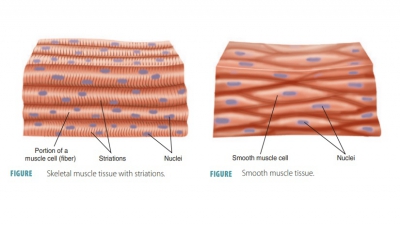
lamina propria lies over a third, deeper layer of smooth muscle cells. Mucous
mem-branes are always wet or moist. The cell composi-tion of mucous membranes
actually varies, but most contain either simple columnar epithelia or
strati-fied squamous epithelia such as in the oral cavity. Mucous membranes may
be adapted for absorption and secretion. Many, but not all, secrete mucus. The
urinary tract is an example of mucosae that do not secrete mucus. It utilizes a
transitional epithelium. Examples of
mucous glands include the submucosal glands of the small intestine and the
sublingual sal-ivary glands. There are also mixed exocrine glands that may produce a serous secretion and
a mucus secretion. One example is the submandibular sali-vary glands.
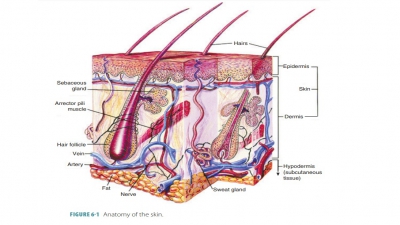
Cutaneous Membrane
The cutaneous
membrane is the skin, which cov-ers the
body surface. It consists of a keratinized strat-ified squamous epithelium,
known as the epidermis. This is
firmly attached to a thick connective tissue layer known as the dermis. The epidermis differs from other
epithelial membranes in that it is dry, thicker, mostly waterproof, and exposed
to the air. The cutaneous membrane is reinforced by a layer of areolar tissue
underneath its dense irregular connec-tive tissue.
Synovial Membranes
Synovial
membranes form an incomplete
lin-ing within the cavities of synovial joints. They are entirely made up of
loose connective tissues. Syno-vial membranes may be the inner of the two
layers of the articular capsule of a synovial joint, with a free smooth surface
lining the joint cavity. They may also be either the superior or inferior
membranes lin-ing the articular capsule of the temporomandibular joint.
Synovial membranes have large areas of the areolar tissue that contains a
matrix of glycoproteins, proteoglycans, and interwoven collagen fibers. The
areolar tissue is separated from the joint cavity by an incomplete layer of
specialized fibroblasts as well as macrophages.
The body’s joints that allow
significant move-ments are very complex, and a fibrous capsule sur-rounds each
of them. The ends of the articulating bones are inside the joint cavity. The
lining of a syno-vial joint is not a true epithelium. It develops within a
connective tissue and has no basement membrane. Separate adjacent cells may be
separated by gaps of up to one millimeter. Fluid and solutes are continuously
exchanged between the synovial fluid and capillaries of underlying connective
tissue.
The surfaces of bones must be
lubricated so that friction does not damage opposing surfaces. Synovial fluid is the clear, viscid, lubricating fluid secreted by synovial membranes, which fills the
joint cavities. It is similar in consistency to that of an egg white. Syno-vial fluid circulates from areolar tissue into
joint cavities through the articular cartilages. It provides oxygen and
nutrients to the chondrocytes. Synovial membranes often have an outer subintima layer (that may be fibrous,
fatty, or loosely areolar) and an inner intima
layer that consists of a sheet of cells that is thin-ner than a sheet of
paper. When the subintima is loose, the intima sits on a pliable membrane.
Joint movement stimulates formation and circulation of synovial fluid. When a
synovial joint is immobilized for a lengthy period of time, the articular
cartilages and synovial membrane begin to degenerate.
1. List the four types of tissue membranes in the body.
2. Which cavities in the body are covered by serous membranes?
3. Define synovial membranes.