Classifications of Connective Tissue
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Levels of Organization : Tissues
Connective tissues are classified based on their physical properties. The three general categories of connective tissues are connective tissue proper, supporting connective tissues, and fluid connective tissues.

Classifications
of Connective Tissue
Connective tissues are classified
based on their physical properties. The three general categories of
connective tissues are connective tissue proper, supporting connective
tissues, and fluid connective tissues.
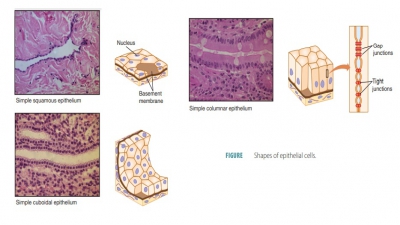
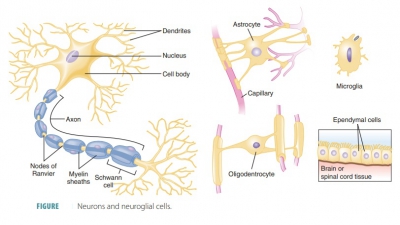
Connective Tissue Proper
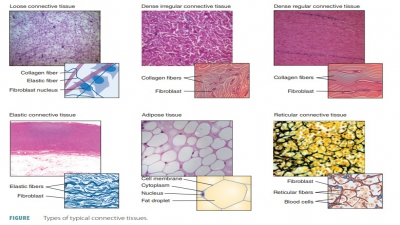
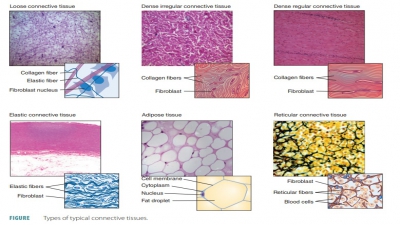
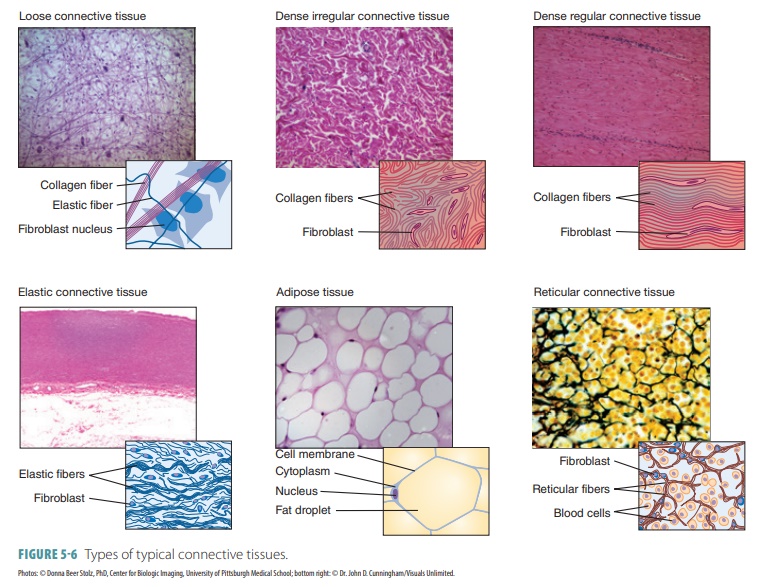
Connective tissue proper includes those connective tissues with many types of cells and extracellular fibers in a syrup-like ground substance. This includes fat and the fibrous tissue of ligaments. All mature connective tissues, except for bone, cartilage, and blood, are con-nective tissue proper. Certain cells, including fibro-blasts, fibrocytes, adipocytes, and mesenchymal cells, aid in local maintenance, repair, and storage of energy. These cells remain in connective tissue permanently. Nonpermanent cells include macrophages, mast cells, lymphocytes, plasma cells, and microphages. These cells defend and repair tissue damage, migrating through healthy connective tissues to collect at sites of tissue injury. The numbers and types of these cells are varied at any given moment. Connective tissue proper is divided into dense connective tissue and loose con-nective tissue (FIGURE 5-6).
Dense Connective Tissue. Dense connective tissue
contains many
collagenous fibers and appears white. Its fine network of elastic fibers contains few cells
and is very strong. The forms of dense connec-tive tissue include dense
regular, dense irregular, and elastic. In the tendons and ligaments, dense
connec-tive tissue binds muscles to bones and bones to other bones. It also
exists in the eyeballs and deep skin layers. Dense connective tissue has a poor
blood supply and is repaired very slowly as a result. Because it has prom-inent
fibers, dense connective tissue is also known as fibrous connective tissue or
collagenous tissue.
■■ Dense regular connective tissue:
This tissue has tightly packed
collagen fiber bundles that run in the same direction, pulling in one parallel
direction. These bundles appear as flexible white structures that have great
resistance to any tension. Between the collagen fibers are lines of
fibroblasts. These cells manufacture the fibers continually as well as small
amounts of ground substance. Col-lagen fibers are wavy in appearance and allow
a small amount of tissue stretching. They have few cells (except for
fibroblasts) and poor vascular-ization. However, they have high tensile
strength and form the tendons (cords
attaching muscles to bones), aponeuroses
(flat tendons that attach muscles to each other or to bones), and ligaments (which bind bones together at
the joints). There is more elastin in ligaments, meaning they stretch to a
greater degree than tendons. Dense regular connective tissue forms fascia, the fibrous mem-brane around muscles, muscle groups,
nerves, and blood vessels.
■■Dense
irregular connective tissue: This tis-sue resembles dense regular connective tissue, but has
much thicker bundles of collagen fibers arranged in an irregular pattern. They
run in more than one plane, forming sheets in areas of the body where tension
occurs from a variety of different directions. Dense irregular tissue is found
in the dermis, fibrous joint
capsules, and in the fibrous coverings of the bones, cartilages, kidneys,
muscles, and nerves. Around cartilages, dense irregular connective tissue forms
a sheath called the perichondrium.
Around bones, it forms the periosteum.
■■ Elastic connective tissue: This tissue actually describes the dense regular connective tissue of cer-tain ligaments, which are able to stretch extensively.These include the ligaments connecting adjacent vertebrae. Also, this type of connective tissue is found in many large artery walls.
Loose Connective Tissue.
Loose
connective tissue
fills spaces between
organs, supports epithe-lia, and protects the specialized cells of many organs.
Loose connective tissue surrounds and supports blood vessels and nerves. It
stores lipids and creates a route for diffusion of various materials. Loose
connective tissue includes adipose (fat) tissue, areolar tissue, and reticular connective tissue.
■■ Adipose tissue: This tissue
lies beneath the skin, between
muscles, around the kidneys, behind the eyes, in certain membranes of the
abdomen, on the heart’s surface, and around some of the body’s joints. It
functions as a cushion for these body parts and, in total, comprises
approximately 18% of an average adult’s body weight. Up to 50% of body weight
can be that of the adipose tissue before the person is termed
morbidly obese. Adipose tissue is also important for storing energy in fat molecules
(triglycerides).
Adipocytes (fat cells) make up approximately
90% of adipose tissue, which has a
simple matrix. Its cells are packed together tightly, resembling a wire fence.
Most of each adipocyte’s volume is filled with one drop of nearly pure
triglyceride, which displaces its nucleus and organelles to one side. In the
entire human body, the mature adi-pocyte is one of the largest cells. They
become “plump” as they take up fat and more wrinkled when they release it.
Adipose tissue has high met-abolic activity because of its rich
vascularization. It usually accumulates in subcutaneous tissue but may develop
anywhere in the body that has ade-quate areolar tissue. The number of
adipocytes varies widely between different connective tissues, body regions,
and among individuals.
Under the skin, abundant fat
supplies general nutrients to the body. Small fat deposits supply nutrients to
highly active organs such as the heart, lymph nodes, certain muscles, and bone
marrow. Often, these local deposits have large amounts of special lipids needed
for their activities. This type of adipose tissue is also described as white adipose tissue or white fat. It
differs from brown adipose tissue (brown
fat) in that white fat stores nutrients
mostly for other cells. Brown fat has many mito-chondria, which warm the
body by using lipid fuels to heat the bloodstream instead of producing
adenosine triphosphate molecules. Brown fat is richly vascular. It is found
mostly on the backs of infants, as at this early stage of life infants cannot produce
body heat by shivering. In adults, only very small amounts of brown fat are
present. This is located primarily above the collarbones, on the neck, on the
abdomen, and around the spine.
In adults, adipocytes do not
divide. Fat cells present in peripheral tissues are determined when an
individual is only a few weeks old. This may be based on the infant’s diet.
Since loose connective tissue also contains mesenchymal cells, when
cir-culating lipid levels are chronically elevated, the mesenchymal cells divide.
This causes the devel-opment of cells that will differentiate into fat cells.
Therefore, areas of areolar tissue become adipose tissue when nutrition is more
than adequate. This also occurs in adults.
■■ Areolar tissue: This tissue
binds skin to underlying organs and
fills in spaces between muscles. It is found beneath most layers of the
epithelium and is simi-lar to adipose tissue in both structure and function,
but lacks the nutrient-storing capability of the adi-pose tissue. It also
supports other tissues, holds body fluids, defends against infection, and
stores nutrients as fat. Fibroblasts, mast cells, and macrophages are the
primary cells in the areolar
tissue that act as barriers to
pathogens. Fat cells are either single or in clusters, and mast cells are
present as large, darkly stained cytoplasmic granules. Other cell types are
also present, but in lower concentrations.
Areolar tissue has loose fibers,
and the remain-der of its matrix appears “empty,” containing only its ground
substance. This looseness allows the tissue to act as a water and salt
reservoir for nearby body tis-sues. It can hold about the same amount of fluid
as is present in the entire bloodstream. Basically, all body cells get nutrients
from this tissue fluid and release their wastes into it. Hyaluronic acid is
present in high concentrations, which makes its ground substance thick
(viscous), slowly cellular movement through it. Certain white blood cells,
therefore, secrete hyal-uronidase, an
enzyme that liquefies the ground sub-stance somewhat so they can pass through
it more easily. Certain bacteria can also do this. Inflamma-tion in a body
region causes the areolar tissue to absorb excess fluids, so the area becomes
swollen (the condition known as edema).
There is more are-olar connective tissue throughout the body than any other
type. It holds body parts together while letting them move freely over each
other; encases glands, nerves, and small blood vessels; and forms the sub-cutaneous
tissue. Most epithelia rest on areolar tissue and it is also present in all
mucous membranes.
■■ Reticular connective tissue:
This tissue helps to cre-ate a framework inside internal organs such as the
spleen and liver and in the lymph nodes and bone marrow. It appears similar to
the areolar tissue, but only has reticular fibers in its matrix, forming a
delicate network containing scattered reticular cells (fibroblasts). Even
though reticular fibers are found throughout the body, reticular tissue is only
found in certain areas. Reticular tissue forms an internal framework (stroma) supporting free lym-phocytes and
other blood cells.
Supporting Connective Tissue
Supporting
connective tissue differs from
con-nective tissue proper because it has a less diverse cell population and a
matrix that contains many more densely packaged fibers. The supporting
connective tissue protects soft tissues and some or all of the body’s weight.
The two types of supporting connective tissue are cartilage and bone.
Cartilage. Cartilage is a tough but flexible connective tissue with a
gelatinous matrix that con-tains an abundance of fibers. It supports, frames,
and attaches to many underlying tissues and bones. Mature cartilage cells,
known as chondrocytes, lie totally inside the extracellular matrix, within cavities called lacunae.
Cartilage is enclosed in a covering called the perichondrium, which provides nutrients via diffusion. It has no
direct blood supply, so car-tilage heals very slowly. Cartilage protects the
body from excessive tension and compression and is harder than dense connective
tissue but softer than bone. It also lacks nerve fibers. The ground substance
of car-tilage has great amounts of chondroitin sulfate and hyaluronic acid
bound firmly within its collagen (and elastic) fibers. There is a large amount
of tissue fluid in its matrix. Surprisingly, cartilage is made up of about 80%
water, which allows it to recover after being com-pressed and nourishes its
cells. There are three major types of cartilage: hyaline, elastic, and
fibrocartilage.
■■ Hyaline
cartilage: This is found on
the ends of
bones in many joints,
the soft portion (tip) of the nose, and in the respiratory passages’ supporting
rings. It is important for bone growth. Hyaline cartilage is the most common
type of cartilage in the body (FIGURE 5-7). Hyaline cartilage is com-monly referred to as gristle. Its matrix appears “glassy,”
with a bluish white color. However, under a microscope, a large number of
collagen fibers are seen. Only 1% to 10% of its volume is made up of
chondrocytes. Hyaline cartilage is partially pliable and provides firm support.
On the ends of long bones, it is known as articular
cartilage, because it absorbs compression at the joints. It also connects
the ribs to the sternum. Most of the skeletons of human embryos consist of
hyaline cartilage before the formation of the bones. During childhood, skeletal
hyaline cartilage persists as the epiphyseal
plates, which are continually growing
regions near the ends of the long
bones.
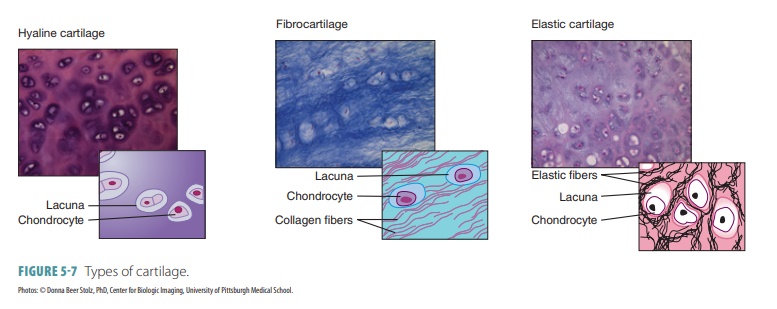
■■ Elastic
cartilage: This is flexible
and provides the framework for the pinna of the ear and the epiglottis of the larynx. Although
nearly identical to hyaline cartilage, elastic cartilage has much more elastin.
It is not only mostly located where a large amount of stretching capacity is
needed, but it also supplies significant strength to various body structures.
■■ Fibrocartilage: This is a tough form of cartilage that absorbs shock in the intervertebral discs of the spinal column,
spongy cartilages (menisci) of the knees, and in the pelvic girdle. It is a
structural “halfway point” between hyaline cartilage and dense regular
connective tissues. Fibrocartilage contains rows of chondrocytes that alternate
with rows of thick collagen fibers. It is able to be compressed and also to
resist tension. Fibrocartilage is located wherever there is a need for extreme support
or to withstand heavy pressure.
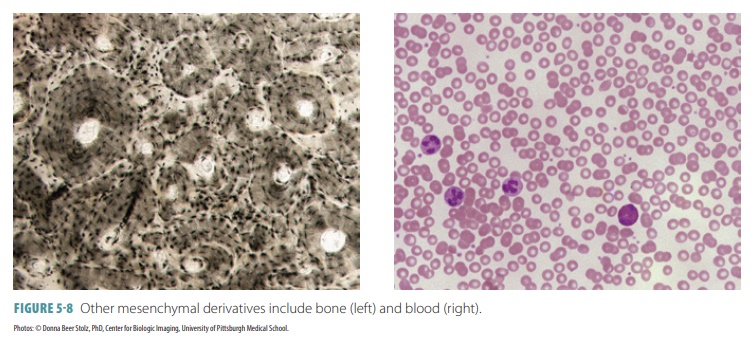
Bone Bone (osseous tissue) is the most rigid type of connective tissue, with a high mineral content that makes it harder than other types. Bone tissue establishes the framework of the body. Bone consists of a matrix of con-nective tissue, blood vessels, and minerals (particularly calcium and phosphorus). The bone matrix is more rigid and harder than other types of connective tissue matrices because of two elements: increased amounts of collagen fibers and the presence of bone salts, which are inorganic calcium salts. The bones also store fat and synthesize blood cells, and they attach to muscles and protect and support vital body structures.
Bone marrow is the soft tissue that fills the
inside of bones and is the site of
production of red blood cells, platelets, and most white blood cells. Bone
cells or osteocytes contain a small amount of ground sub-stance; but they actually consist
of a dense and miner-alized matrix. These cells are located in the lacunae of
the bone matrix. The osteocytes and layers of the extra-cellular matrix form a
cylinder-shaped osteon (also called a Haversian system;
FIGURE 5-8). They have con-centric rings of bony matrix (lamellae) that surround central canals. These canals contain blood
vessels and nerves. Many osteons that are cemented together form the substance
of bone. Bone is well supplied by blood vessels, unlike cartilage. The organic
portion of the matrix is formed by osteoblasts, followed by deposi-tion of bone salts on and between the fibers.
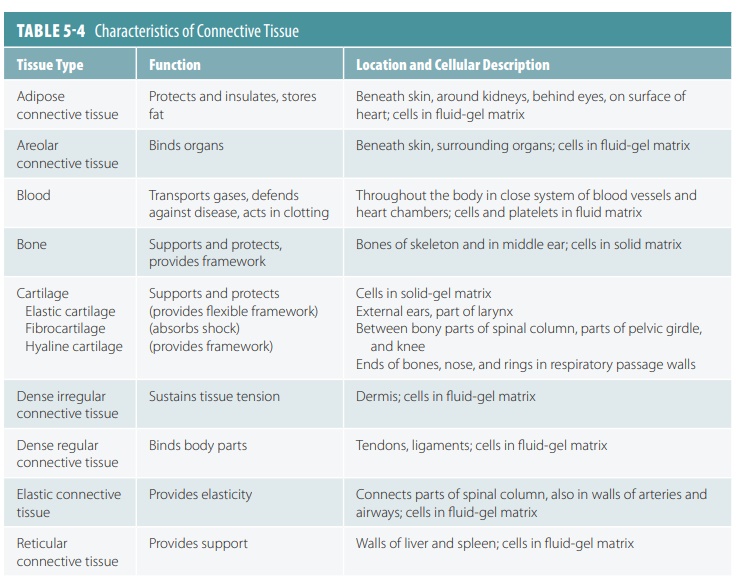
Fluid Connective Tissues
Fluid connective tissues have distinctive popula-tions of cells suspended in a water matrix. This contains dissolved proteins and may be of two types: blood or lymph. Blood and lymph are fluid connective tissues that contain distinctive collections of cells in a fluid matrix. They transport many materials between inte-rior body cells and other cells that exchange substances with the external environment, maintaining a stable internal environment. Blood contains formed elements (red blood cells, white blood cells, and platelets) that are suspended in a liquid extracellular matrix known as blood plasma. Together, the formed elements and blood plasma make up the blood. Most blood cells are formed in the red bone marrow. Red blood cells (erythrocytes) are the most prevalent type of blood cells. Blood is clas-sified as a connective tissue because it develops from mesenchyme. During blood clotting, the fibers of blood (soluble protein molecules) form visible fiber-like structures. During an infection, the number of lympho-cytes, plasma cells, microphages, and macrophages will increase in the infected area. Lymph forms as intersti-tial fluid entering the lymphatic vessels, which return the lymph to the cardiovascular system. Unlike other connective tissues, blood and lymph do not connect structures or provide any mechanical support. TABLE 5-4 summarizes the characteristics of connective tissue.
1. What
are the functions of connective tissue?
2. What
are the primary blast cell types of connective tissue?
3. What
are the three types of cartilage?
4. Name
the three types of fibers that make up connective tissues.
5. Which
types of connective tissue have a fluid matrix?