Treatment of Epilepsies
| Home | | Pharmacology |Chapter: Essential pharmacology : Antiepileptic Drugs
Antiepileptic drugs suppress seizures, but do not cure the disorder; the disease may fadeout though after years of successful control. The aim of drugs is to control and totally prevent all seizure activity at an acceptable level of side effects.
TREATMENT OF EPILEPSIES
Antiepileptic drugs suppress seizures, but do not cure the
disorder; the disease may fadeout though after years of successful control. The
aim of drugs is to control and totally prevent all seizure activity at an
acceptable level of side effects. With the currently available drugs, this can
be achieved in about half of the patients. Another 20–30% attain partial
control, while the rest remain resistant. The cause of epilepsy should be
searched in the patient; if found and treatable, an attempt to remove it should
be made. Some general principles of symptomatic treatment with antiepileptic drugs
are:
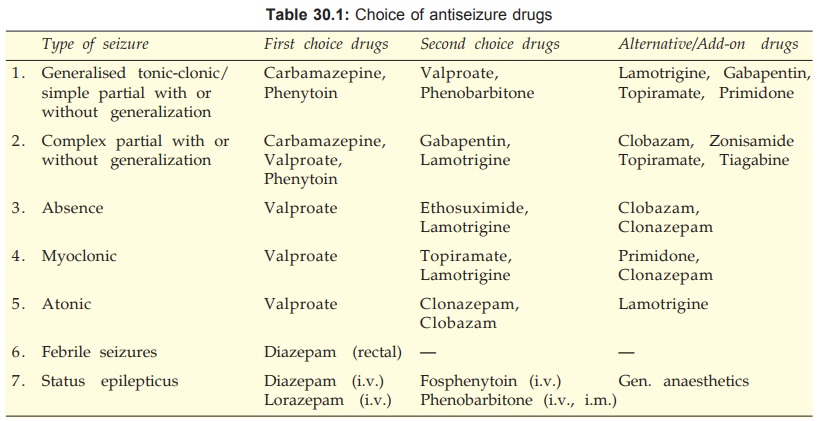
1.
Choice of drug (Table 30.1) and dose is
according to the seizure type(s) and need of the individual patient.
2. Initiate treatment early, because each seizure
episode increases the propensity to further attacks, probably by a process akin
to kindling. Start with a single drug, preferably at low dose— gradually
increase dose till full control of seizures or side effects appear. If full
control is not obtained at maximum tolerated dose of one drug, substitute
another drug. Use combinations when all reasonable monotherapy fails. Combining
drugs with different mechanisms of action, such as those which prolong Na+
channel inactivation with those facilitating GABA appears more appropriate.
Pharmacokinetic interactions among anticonvulsants are common; dose adjustments
guided by therapeutic drug monitoring are warranted.
3. Therapy should be as simple as possible. A seizure diary
should be maintained.
4. All drug withdrawals should be gradual (except
in case of toxicity), abrupt stoppage of therapy without introducing another
effective drug can precipitate status epilepticus. Prolonged therapy (may be
lifelong, or at least 3 years after the last seizure) is needed. Withdrawal may
be attempted in selected cases. Factors favourable to withdrawal are—childhood
epilepsy, absence of family history, primary generalized tonic-clonic epilepsy,
recent onset at start of treatment, absence of cerebral disorder and normal EEG.
Even then recurrence rates of 12–40% have been reported.
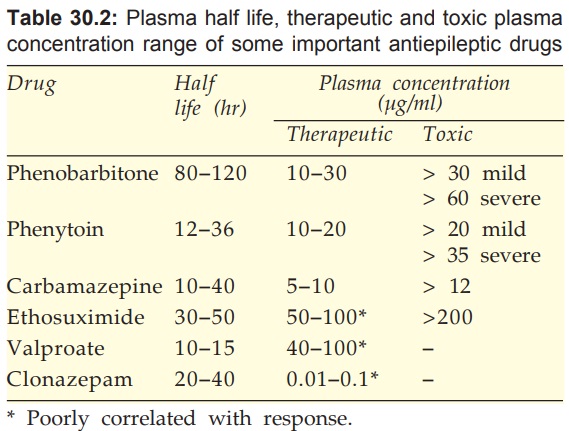
5. Dose regulation may be facilitated by monitoring of steady state
plasma drug levels. Monitoring is useful because:
•
Therapeutic range of concentrations has been
defined for many drugs.
•
There is marked individual variation in the plasma
concentration attained with the same daily dose.
•
Compliance among epileptic patients is often
poor.
Plasma levels given in Table 30.2 are to serve as rough guides:
6. When women on antiepileptic therapy conceive, antiepileptic
drugs should not be stopped. Though, most antiseizure drugs have been shown to
increase the incidence of birth defects, discontinuation of therapy carries a high
risk of status epilepticus. Fits occurring during pregnancy themselves increase
birth defects and may cause mental retardation in the offspring (anoxia occurs
during seizures). An attempt to reduce the dose of drugs should be cautiously
made. It may be advisable to substitute valproate.
Prophylactic folic acid supplementation in 2nd and 3rd trimester
along with vit. K in the last month of pregnancy is recommended, particularly
in women receiving antiepileptic drugs to minimise neural tube defects and bleeding
disorder respectively in the neonate.
7. Individual seizure episodes do not require
any treatment. During an attack of tonic-clonic seizures, the first priority is
to prevent injury due to fall or biting. The patient should be put in prone or
lateral position and a gag should be placed between the teeth. The head should
be turned and patency of airway ensured. The attack usually passes off in 2–3
min, but the patient may not be roadworthy for a couple of hours.
A. Generalised Tonic-Clonic And Simple Partial Seizures
In large comparative
trials, considering both
efficacy and toxicity, carbamazepine and phenytoin have scored highest,
phenobarbitone was intermediate, while primidone was lowest. Carbamazepine was
the best in partial seizures, while valproate was equally effective in
secondarily GTCS. Valproate is a good second line drug but should be used
cautiously in young children for fear of hepatic toxicity. Carbamazepine is
preferred in young girls because of cosmetic side effects of phenytoin.
Lamotrigine, gabapentin and topiramate have emerged as good
alternatives. Newer drugs are to be used as addon therapy in cases with
incomplete/poor response or even as monotherapy in selected patients to avoid
drug interactions and side effects. The newer drugs are less sedating and
produce fewer side effects.
Complete control can be obtained in upto 90% patients with
generalized seizures, but in only 50% or less patients with partial seizures.
Phenobarbitone, phenytoin, valproate and carbamazepine have been
used to treat early post head injury seizures. Phenobarbitone and phenytoin are
often prescribed empirically for prophylaxis of lateonset (8 days to 2 yrs
later) posttraumatic epilepsy, but risk/benefit ratio of such use is not clear.
Decision has to be taken on individual basis.
B. Complex Partial Seizures
This type of epilepsy is difficult to control completely;
relapses are more common on withdrawal. Carbamazepine is the preferred drug,
but phenytoin or valproate may have to be added to it. Phenobarbitone or primidone
could be used with one of the above drugs. The newer drugs clobazam,
lamotrigine, gabapentin and topiramate may be added in refractory cases.
C. Absence Seizures
Ethosuximide and valproate
are equally efficacious, but the latter is more commonly used because it would
also prevent kindling and emergence of GTCS. Valproate is clearly superior in
mixed absence and GTCS, which is more common than pure absence seizures.
Lamotrigine has emerged as a good alternative. Clonazepam is a second line drug
limited by its sedative property and development of tolerance. Clobazam is an
alternative with promise of more sustained response.
D. Myoclonic And Atonic Seizures
Valproate
is the preferred drug and lamotrigine is an effective alternative. Topiramate
may be added in case of poor response. Primidone and clonazepam are occasionally
used.
E. Febrile Convulsions
Some children, especially
under 5 years age, develop convulsions during fever. These may recur every time
with fever and few may become chronic epileptics. Every attempt should be made
to see that they do not develop fever,
but when they do, the temperature should not be allowed to rise by using
paracetamol and external cooling.
The best treatment of febrile convulsions is rectal diazepam 0.5
mg/kg given at the onset of convulsions. The i.v. preparation can be used; a
rectal solution (5 mg in 2.5 ml) in tubes is available in the UK. Seizures
generally stop in 5 min; if not another dose may be given. The drug is repeated
12 hourly for 4 doses. If fever is prolonged a gap of 24–48 hr is given before
starting next series of doses.
In recurrent cases or those at particular risk of developing
epilepsy—intermittent prophylaxis with diazepam (oral or rectal) started at the
onset of fever is recommended. Chronic prophylaxis with phenobarbitone
advocated earlier has been abandoned, because of poor efficacy and behavioral
side effects.
F. Infantile Spasms (Hypsarrhythmia)
Therapy is unsatisfactory,
antiepileptic drugs are generally useless. Corticosteroids afford symptomatic
relief. Valproate and clonazepam have adjuvant value. Vigabatrin has some
efficacy.
G. Status Epilepticus
In status epilepticus seizure activity occurs for >30 min, or two
or more seizures occur without recovery of consciousness. Recurrent tonic-clonic
convulsions without recovery of consciousness in between is an emergency; fits
have to be controlled as quickly as possible to prevent death and permanent
brain damage.
•
Diazepam 10 mg i.v. bolus injection (2 mg/
min) followed by fractional doses every 10 min or slow infusion titrated to
control the fits has been the standard treatment. However, it redistributes
rapidly so that anticonvulsant effect starts fading after 20 min. Lorazepam is
less lipid soluble with slow redistribution: anticonvulsant effect of i.v. dose
lasts for 6–12 hours. It is therefore preferred; 0.1 mg/kg (injected at 2 mg/
min) is effective in 75–90% cases.
•
Phenobarbitone (100–200 mg i.m./i.v.) or
phenytoin (25–50 mg/min in a running saline i.v. line; not to be mixed with
glucose solution because it precipitates. Fosphenytoin is used in its place
now; maximum 1000 mg phenytoin equivalent). These drugs act more slowly; may be
used alternatively to diazepam/lorazepam or substituted for them after the
convulsions have been controlled.
•
Refractory cases may be treated with i.v.
midazolam/propofol/thiopentone anaesthesia, with or without curarization.
• General measures, including maintenance of
airway (intubation if required), oxygenation, fluid and electrolyte balance,
BP, normal cardiac rhythm, euglycaemia and care of the unconscious must be taken.
