Treatment of Urinary Tract Infections
| Home | | Pharmacology |Chapter: Essential pharmacology : Macrolide, Lincosamide, Glycopeptide And Other Antibacterial Antibiotics; Urinary Antiseptics
The general principles of use of AMAs for urinary tract infections (UTIs) remain the same as for any other infection. Some specific considerations are highlighted below.
TREATMENT OF URINARY TRACT INFECTIONS
The general principles of use of AMAs for urinary tract
infections (UTIs) remain the same as for any other infection. Some specific
considerations are highlighted below.
Most UTIs are caused by gram-negative bacteria, especially
coliforms. Majority of acute infections involve a single organism (commonest is
E. coli); chronic and recurrent
infections may be mixed infections. Acute infections are largely self limiting;
high urine flow rates with frequent bladder voiding may suffice. Many single
dose antimicrobial treatments have been successfully tried, but a three day
regimen is considered optimal for lower UTIs. Upper UTIs require more aggressive
and longer treatment. In any case, treatment for more than 2 weeks is seldom
warranted.
Bacteriological investigations are very important to direct the
choice of drug. Though, treatment may not wait till report comes, urine sample
must be collected for bacteriology before commencing therapy. Most AMAs attain
high concentrations in urine, smaller than usual doses may be effective in
lower UTIs—antibacterial action in urine is sufficient, mucosa takes care of
itself. In upper UTI (pyelonephritis) antimicrobial activity in kidney tissue
is needed—doses are similar to any systemic infection.
The least toxic and cheaper AMA should be used just long enough
to eradicate the pathogen. It is advisable to select a drug which does not disrupt
normal gut and perineal flora. If recurrences are frequent, chronic suppressive
treatment with cotrimoxazole, nitrofurantoin, methenamine, cephalexin or
norfloxacin may be given.
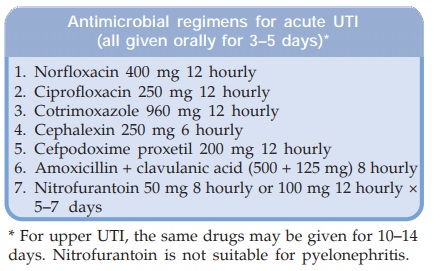
The commonly used antimicrobial regimens for empirical therapy
of uncomplicated acute UTI are given in the box.
The status of AMAs (other than urinary antiseptics) in urinary
tract infections is summarized below:
Sulfonamides
Dependability in acute UTIs has decreased: not
used now as single drug. May occasionally be employed for suppressive and
prophylactic therapy.
Cotrimoxazole
Though response rate
and use have declined, it
may be employed empirically in acute UTI without bacteriological data, because
majority of urinary pathogens, including C.
trachomatis, are covered by
cotrimoxazole. It should not be used
to treat UTI during pregnancy.
Quinolones
The first generation
FQs, especially norfloxacin and ciprofloxacin are highly effective and
currently the most popular drugs, because of potent action against gram-negative
bacilli and low cost. Nalidixic acid is also employed. However, to preserve
their efficacy, use should be restricted. FQs are particularly valuable in
complicated cases, those with prostatitis or indwelling catheters and for
bacteria resistant to cotrimoxazole/ampicillin. The FQs should not be given to
pregnant women.
Ampicillin/Amoxicillin
Frequently used in the past as first choice
drug for initial treatment of acute infections without bacteriological data,
but higher failure and relapse rates have made them unreliable for empirical
therapy. Many E. coli strains are now
ampicillin-resistant. Amoxicillin + clavulanic acid is more frequently
employed.
Cloxacillin
Use is restricted to
penicillinase producing staphylococcal infection, which is uncommon in
urinary tract.
Piperacillin/Carbenicillin
Only in serious Pseudomonas infection in patients
with indwelling catheters or chronic obstruction, and in hospitalized patients.
Cephalosporins
Use is increasing,
especially in women with
nosocomial Klebsiella and Proteus infections; should normally be used
only on the basis of sensitivity report, but empirical use for community
acquired infection is also common. Some guidelines recommend them as
alternative drugs.
Gentamicin
Very effective against
most urinary pathogens including
Pseudomonas. However, because of narrow
margin of safety and need for parenteral administration, it is generally used
only on the basis of in vitro
bacteriological sensitivity testing. The newer aminoglycosides may be needed
for hospital-acquired infections.
Chloramphenicol
Though effective in many cases, use should be restricted,
for fear of toxicity, to pyelonephritis in cases where the causative bacteria
is sensitive only to this antibiotic.
Tetracyclines
They are seldom
effective now, because most urinary pathogens
have become resistant. Though broad spectrum, they are used only on the basis
of sensitivity report and in Ch. No.
trachomatis cystitis.
Urinary pH In Relation To Use Of AMAs
Certain AMAs act better in acidic urine, while others in alkaline
urine. However, specific intervention to produce urine of desired reaction (by
administering acidifying or alkalinizing agents) is seldom required (except for
methenamine), because most drugs used in UTI attain high concentration in urine
and minor changes in urinary pH do not affect clinical outcome. In case of
inadequate response or in complicated cases, measurement of urinary pH and
appropriate corrective measure may help.
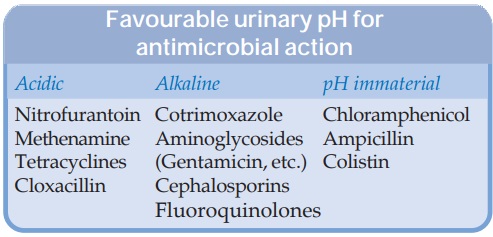
In certain urease
positive Proteus (they split urea
present in urine into NH3) infections it is impossible to acidify
urine. In such cases, acidification should not be attempted and drugs which act
better at higher pH should be used.
Urinary Infection In Patients With
Renal Impairment
This is relatively
difficult to treat because most AMAs attain lower urinary concentration.
Methenamine mandelate, tetracyclines (except doxycycline) and certain
cephalosporins are contraindicated.
Nitrofurantoin, nalidixic
acid and aminoglycosides are better avoided. Still, every effort must be made
to cure the infection, because if it persists, kidneys may be further damaged.
Bacteriological testing and followup cultures are a must to select the
appropriate drug and to ensure eradication of the pathogen. Potassium salts and
acidifying agents are contraindicated.
Prophylaxis For Urinary Tract Infection
This may be given
when:
· Catheterization or
instrumentation inflicting trauma to the lining of the urinary tract is
performed; bacteremia frequently occurs and injured lining is especially
susceptible.
· Indwelling catheters
are placed.
· Uncorrectable
abnormalities of the urinary tract are present.
· Inoperable prostate
enlargement or other chronic obstruction causes urinary stasis.
