Choice of an Antimicrobial Agent
| Home | | Pharmacology |Chapter: Essential pharmacology : Antimicrobial Drugs: General Considerations
After having established the need for using a systemic AMA in a patient by assessing that the condition is due to a treatable (mostly bacterial) infection, and that it is not likely to resolve by itself or by local measures (antiseptics, drainage of pus, etc) only, one has to choose a drug from the large number available.
CHOICE OF AN ANTIMICROBIAL AGENT
After having
established the need for using a systemic AMA in a patient by assessing that
the condition is due to a treatable (mostly bacterial) infection, and that it
is not likely to resolve by itself or by local measures (antiseptics, drainage
of pus, etc) only, one has to choose a drug from the large number available.
The choice depends on the peculiarities of the patient, the infecting organism
and the drug.
Patient factors
1. Age may affect kinetics of
many AMAs. Conjugation and
excretion of chloramphenicol is inefficient in the newborn: larger doses
produce gray baby syndrome. Sulfonamides
displace bilirubin from protein
binding sites—can cause kernicterus in the neonate because their bloodbrain
barrier is more permeable. The t½ of aminoglycosides is prolonged in the elderly
and they are more prone to develop VIII nerve toxicity. Tetracyclines deposit
in the developing teeth and bone—discolour and weaken them—are contraindicated
below the age of 6 years.
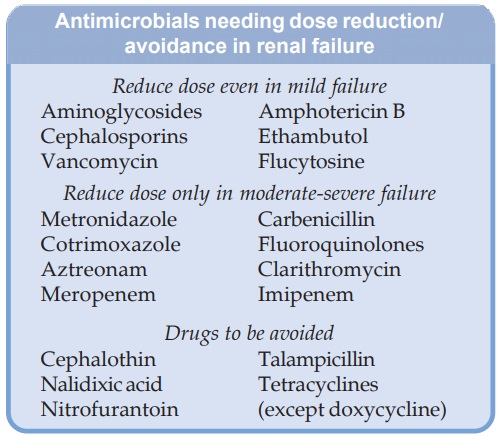
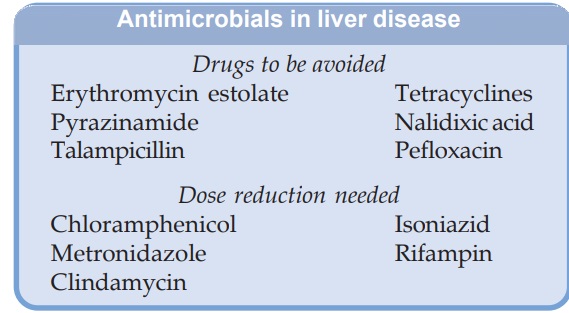
2. Renal And Hepatic Function Cautious use and modification of the
dose of an AMA (with low safety margin) becomes necessary when the organ of its
disposal is defective (see box).
3. Local Factors The conditions
prevailing at the site of infection
greatly affect the action of AMAs.
(a) Presence of pus and secretions decrease the efficacy of most
AMAs, especially sulfonamides and aminoglycosides. Drainage of the abscess
reduces the population of the causative bacteria, suppresses anaerobes by
exposure to oxygen, and improves diffusion of the antibiotic into the abscess.
(b) Presence of necrotic material or foreign body makes
eradication of infection practically impossible.
(c) Haematomas foster bacterial growth; tetracyclines,
penicillins and cephalosporins get bound to the degraded haemoglobin in the
haematoma.
(d) Lowering of pH at the site of infection reduces activity of
macrolide and aminoglycoside antibiotics.
(e) Anaerobic environment in the centre of an abscess impairs
bacterial transport processes which concentrate aminoglycosides in the
bacterial cell, rendering them less susceptible.
(f) Penetration barriers may hamper the access of the AMA to the
site of infection in subacute bacterial endocarditis (SABE), endophthalmitis,
prostatitis. However, trimethoprim and fluoroquinolones attain high
concentration in prostate due to ion trapping.
4. Drug Allergy
History of previous exposure to an AMA should be
obtained. If a drug has caused allergic reaction —it has to be avoided in that
patient, e.g. drug of choice for syphilis in a patient allergic to penicillin
is tetracycline.
βlactams, sulfonamides,
fluoroquinolones and nitrofurantoin frequently cause allergy.
5. Impaired
Host Defence Integrity of host defence plays a
crucial role in overcoming an infection. Pyogenic infections occur readily in
neutropenic patients, while if cellmediated immunity is impaired (e.g. AIDS),
infections by low grade pathogens and intracellular organisms abound. In an
individual with normal host defence, a bacteriostatic AMA may achieve cure;
while intensive therapy with cidal drugs is imperative in those with impaired
host defence (conditions given on p. 672) or when the organisms are protected
by a barrier—as in SABE. Even then complete eradication of the organism may not
occur.
6. Pregnancy
All AMAs should be avoided in the pregnant because
of risk to the foetus. Penicillins, many cephalosporins and erythromycin are
safe, while safety data on most others is not available. Therefore,
manufacturers label ‘contraindicated during pregnancy’. Tetracyclines carry
risk of acute yellow atrophy of liver, pancreatitis and kidney damage in the
mother. They also cause teeth and bone deformities in the offspring.
Aminoglycosides can cause foetal ear damage. Animal studies indicate increased
risk to the foetus, especially with fluoroquinolones, cotrimoxazole, chloramphenicol,
sulfonamides and nitrofurantoin. Though metronidazole has not been found
teratogenic, its mutagenic potential warrants caution in its use during
pregnancy.
7. Genetic
Factors Primaquine, nitrofurantoin, sulfonamides,
chloramphenicol and fluoroquinolones are likely to produce haemolysis in G6PD
deficient patient.
Organism-Related Considerations
Each AMA has a specific effect on a limited number of microbes.
Successful chemotherapy must be rational and demands a diagnosis. However, most
of the time, definitive bacteriological diagnosis is not available before
initiating treatment. Bacteriological testing is time consuming, expensive and
appropriate samples of infected material for bacteriology may not be
obtainable. A clinical diagnosis should first be made, at least tentatively,
and the likely pathogen guessed. The following line of action may be taken:
1. Clinical Diagnosis Itself
Directs Choice Of The AMA The infecting organism and its sensitivity are not variable, e.g. syphilis, chancroid, diphtheria,
tetanus, plague, cholera, trachoma thrush, tuberculosis, lobar pneumonia,
leprosy, amoebiasis, herpes simplex, etc.
2. A Good Guess Can Be Made from the clinical features and local
experience about the type of organism and its sensitivity: tonsillitis, otitis
media, boils, vaginitis, urethritis; the most appropriate specific AMA should
be prescribed and the response watched for. A gram stained smear examination of
infected material may help to aid the choice.
3. Choice
To Be Based On Bacteriological Examination No guess can be made
about the infecting organism or its
sensitivity, e.g. bronchopneumonia, empyema, meningitis, osteomyelitis, urinary
tract infection, wound infection, etc. In these situations, an AMA should be
selected on the basis of culture and sensitivity testing; but this may not be
always possible.
a)
Bacteriological services not available: empirical therapy to cover all likely organisms
with a broadspectrum drug like fluoroquinolone, tetracycline or a combination
such as penicillin + streptomycin or gentamicin + a cephalosporin may be used
(with metronidazole if anaerobes are suspected). Further therapy is modified on
the basis of clinical response; but hasty and arbitrary changes in therapy
should be avoided.
b) Bacteriological services available, but
treatment cannot be delayed: as in serious infections like meningitis, septicaemias, etc.,
specimens for bacteriological examination should be sent and empirical therapy
started provisionally as in (a). In case of inadequate response, the AMA should
be changed later in the light of bacteriological findings.
c)
Bacteriological services are available and treatment can be delayed for a few
days: as in chronic urinary tract
infection; it is better to wait for the culture and sensitivity report; start
definitive therapy thereafter.
Bacteriological Sensitivity Testing
This is generally done by diskagar diffusion method using
standardized concentrations of antibiotics based on clinically attained plasma
concentrations of these. As such, they serve only as guides and cannot be
blindly extrapolated to the clinical situation in every patient and for every
organism. Broth cultures with breakpoint
concentration (concentration that demarcates between sensitive and resistant
bacteria) of antibiotics probably yield more reliable results. Breakpoint
concentrations are based on clinically attainable serum concentrations of the
antibiotic.
Minimum inhibitory concentration (MIC), i.e the lowest concentration of an antibiotic which
prevents visible growth of a bacterium determined in microwell culture plates
using serial dilutions of the antibiotic is more informative, but not estimated
routinely.
Minimum bactericidal concentration (MBC), of the antibiotic is determined by
subculturing from tubes with no visible growth. If the organism is killed, no
growth will occur; but if it was only inhibited in the parent culture—it will
grow on subculturing in antibioticfree medium. MBC is the concentration of the
antibiotic which kills 99.9% of the bacteria. A small difference between MIC
and MBC indicates that the antibiotic is primarily bactericidal, while a large
difference indicates bacteriostatic action. MBC is not used to guide selection
of antibiotics in clinical practice.
Post-antibiotic effect (PAE) After a brief exposure if the organism is placed in antibioticfree medium, it starts multiplying
again, but after a lag period which depends on the antibiotic as well as the
organism. This lag period in growth resumption is known as ‘post-antibiotic
effect’ and is the time required for re-attainment of logarithmic growth. A
long PAE has been noted with fluoroquinolones, aminoglycosides and βlactam antibiotics.
Drug Factors
When any one of a
number of AMAs could be used to treat an infection, choice among them is based
upon specific properties of these AMAs:
1. Spectrum Of Activity: For definitive therapy,
a narrow-spectrum drug
which selectively affects the concerned organism is preferred, because it is
generally more effective than a broad-spectrum AMA, and is less likely to
disturb the normal microbial flora. However, for empirical therapy, often a
broad-spectrum drug has to be used to cover all likely pathogens.
2. Type Of
Activity: Many infections in patients with normal host
defence respond equally well to bacteriostatic and bactericidal AMAs. But
several acute infections resolve faster with a cidal than a static drug,
because the cidal drug directly reduces the number of bacteria at the site of
infection, while the static drug only prevents increase in their number. Many
bactericidal drugs exert prolonged post-antibiotic effect so that maintenance
of drug level continuously above the MIC is not essential. With bacteriostatic
AMAs the bacteria start multiplying quickly when drug level falls below the
MIC, resulting in relapse of infection.
A bactericidal antibiotic is clearly superior to bacteriostatic
one in treating patients with impaired host defence, life-threatening
infections, infections at less accessible sites (SABE) or when carrier state is
possible (typhoid).
3. Sensitivity
Of The Organism: assessed on the basis of MIC values
(if available) and consideration of postantibiotic effect.
4. Relative
Toxicity: Obviously, a less toxic antibiotic is preferred, e.g. a βlactam over an aminoglycoside
or erythromycin over clindamycin.
5. Pharmacokinetic Profile: For optimum action the antibiotic has to be present at the site
of infection in sufficient concentration for an adequate length of time. This
depends on their pharmacokinetic characteristics. Most antibiotics are given at
2 to 4 halflife intervals—thus attaining therapeutic concentrations only intermittently.
For many organisms, aminoglycosides and fluoroquinolones produce ‘concentration-dependent
inhibition’—inhibitory effect depends on the ratio of peak concentration to the
MIC; the same daily dose of gentamicin produces better action when given as a
single dose than if it is divided into 2–3 portions. On the other hand, βlactams, glycopeptides
and macrolides produce ‘time-dependent inhibition’—antimicrobial action depends
on the length of time the concentration remains above MIC; division of daily
dose has better effect. However, the doses should be so spaced that the surviving
organisms again start multiplying and a cidal action is exerted.
Penetration to the
site of infection also depends on the pharmacokinetic properties of the drug. A
drug which penetrates better and attains higher concentration at the site of
infection is likely to be more effective. The fluoroquinolones have excellent
tissue penetration—attain high concentrations in soft tissues, lungs, prostate,
joints, etc. Ciprofloxacin and rifampin have very good intracellular
penetration. Cefuroxime, ceftriaxone, chloramphenicol, ciprofloxacin attain
high CSF concentration. On the other hand, penicillins and aminoglycosides
penetrate poorly into CSF unless meninges are inflamed. Ampicillin,
cephalosporins and erythromycin attain high biliary concentration.
6. Route Of
Administration: Many AMAs can be given orally as well
as parenterally, but aminoglycosides, penicillin G, carbenicillin, many
cephalosporins, vancomycin, etc. have to be given by injection only. For less
severe infections, an oral antibiotic is preferable; but for serious
infections, e.g. meningitis, spreading cellulitis, septicaemias, a parenteral
antibiotic may be chosen.
7. Evidence
Of Clinical Efficacy: Relative value of different AMAs in
treating an infection is decided on the basis of comparative clinical trials.
Optimum dosage regimens and duration of treatment are also determined on the
basis of such trials. Reliable clinical trial data, if available, is the final
guide for choice of the antibiotic.
8. Cost: Less expensive drugs
are to be preferred.
Related Topics
