Angiotensin Converting Enzyme Inhibitors
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs Affecting Renin-Angiotensin System And Plasma Kinins
Teprotide was the first ACE inhibitor to be synthesized taking a lead from the bradykinin potentiating factor (BPF) found in pit viper venom and the finding that the kininase was also ACE.
ANGIOTENSIN CONVERTING ENZYME
INHIBITORS
Teprotide was the first ACE inhibitor to be synthesized taking a
lead from the bradykinin potentiating factor (BPF) found in pit viper venom and
the finding that the kininase was also ACE. Teprotide, a nonapeptide inhibited
generation of AII from AI and lowered BP. However, it had limitations of
parenteral administration and brief duration of action.
Captopril, an orally
active dipeptide analogue was introduced in 1977 and quickly gained wide usage.
A multitude of ACE inhibitors have since been added, of which—captopril, enalapril, lisinopril,
benazepril, ramipril, fosinopril, trandolapril, imidapril and perindopril are available in India. Some others like quinapril, cilazapril
zofenopril, etc. are marketed in other countries. The pharmacology of captopril
is described as prototype, since most of its effects are class effects common
to all ACE inhibitors.
Captopril
It is a sulfhydryl containing dipeptide surrogate of proline
which abolishes the pressor action of AI but not that of AII: does not block AII
receptors.
Captopril can also increase plasma kinin levels and potentiate
the hypotensive action of exogenously administered bradykinin. Pretreatment
with B2 kinin receptor antagonist has shown that kinins do contribute to the
acute vasodepressor action of ACE inhibitors, but they appear to have little
role in the long-term hypotensive effect, probably because kinins play only a minor
role, if at all, in BP regulation, and another enzyme ‘Kininase I’ (which also
degrades bradykinin) is not inhibited. Nevertheless, elevated kinins (and PGs
whose synthesis is enhanced by kinins) may be responsible for cough and
angioedema induced by ACE inhibitors in susceptible individuals. ACE inhibitors
interfere with degradation of substance P also.
Captopril lowers BP,
but in the short-term, magnitude of response is dependent on Na+
status and the level of renin-angiotensin activity. In normotensive Na+
replete individuals, the fall in BP attending initial few doses of ACE
inhibitors is modest. This is more marked when Na+ has been depleted
by dietary restriction or diuretics. A greater fall in BP occurs in
renovascular, accelerated and malignant hypertension. In essential hypertension
it has been found that RAS is overactive in 20%, normal in 60% and hypoactive
in the rest. Thus, it contributes to maintenance of vascular tone in over 80%
cases and its inhibition results in lowering of BP. However, in the long-term
no correlation has been observed between plasma renin activity (PRA) and
magnitude of fall in BP due to captopril.
Captopril induced
hypotension is a result of decrease in total peripheral resistance. The
arterioles dilate and compliance of larger arteries is increased. Both systolic
and diastolic BP fall. It has no effect on cardiac output. Cardiovascular
reflexes are not interfered with and there is little dilatation of capacitance
vessels. As such, postural hypotension is not a problem. Reflex sympathetic
stimulation does not occur despite vasodilatation. They can be safely used in
patients with ischaemic heart disease. The renal blood flow is not compromized
even when BP falls substantially. This is due to greater dilatation of renal vessels
(AII markedly constricts them). Cerebral and coronary blood flow are also not
compromized.
Reflex (postural)
changes in plasma aldosterone are abolished and basal levels are decreased as a
consequence of loss of its regulation by AII. However, physiologically sufficient
mineralocorticoid is still secreted under the influence of ACTH and plasma K+
. Levels of plasma renin and AI are increased as a compensatory measure, but the
physiological significance of this appears to be minor (most actions are exerted
through generation of AII).
Pharmacokinetics
About 70% of orally
administered captopril is absorbed. Presence of food in stomach reduces its
bioavailability. Penetration in brain is poor. It is partly metabolized and
partly excreted unchanged in urine. The plasma t½ is ~2 hours, but actions last
for 6–12 hours.
Adverse Effects
The adverse effect
profile of all ACE inhibitors is
similar. Captopril is well tolerated by most patients, especially if daily dose
is kept below 150 mg.
Hypotension: an initial sharp fall in BP occurs especially in diuretic treated and CHF
patients; persistent hypotension may be troublesome in MI patients.
Hyperkalaemia: more likely in patients with impaired renal function and in those
taking K+ sparing diuretics, NSAIDs or β blockers. In others
significant rise in plasma K+ is rare.
Cough: a persistent brassy cough occurs in 4–16% patients within 1–8 weeks, often
requires discontinuation of the drug—subsides 4– 6 days thereafter. It is not
dose related and appears to be caused by inhibition of bradykinin/substance P
breakdown in the lungs of susceptible individuals.
Rashes,
urticaria: occur in 1–4%
recipients; does not usually warrant
drug discontinuation.
Angioedema: resulting in swelling
of lips, mouth, nose, larynx may develop
within hours to few days in 0.06–0.5% patients; may cause airway obstruction;
treat with Adr, antihistaminics, corticosteroids according to need.
Dysgeusia: reversible loss or alteration of taste sensation due to captopril has an
incidence of 0.5–3%; lower incidence with other ACE inhibitors has been noted.
Foetopathic: foetal growth retardation, hypoplasia of
organs and foetal death may occur if ACE inhibitors are given during later half
of pregnancy. A recent report indicates 2.7fold higher malformation rate in
foetuses exposed to ACE inhibitors in the first trimester. ACE inhibitors must
be stopped when the woman conceives.
Headache,
Dizziness, Nausea And Bowel Upset:
each reported in 1–4%
patients.
Granulocytopenia
and Proteinuria: are rare, but warrant withdrawal. Renal disease
predisposes to these adverse effects. However, ACE inhibitors retard diabetic
nephropathy, reduce attendant proteinuria, and are renoprotective.
Acute
Renal Failure: is precipitated by ACE inhibitors in patients with bilateral
renal artery stenosis due to dilatation of efferent arterioles and fall in
glomerular filtration pressure. ACE inhibitors are contraindicated in such
patients.
Interactions
Indomethacin (and
other NSAIDs) attenuate the
hypotensive action. Incidents of renal failure have been reported when a NSAID
was given to patients (especially elderly) receiving ACE inhibitor + diuretic.
Hyperkalaemia can occur if K+ supplements/K+ sparing
diuretics are given with captopril. Antacids reduce bioavailability of
captopril, while ACE inhibitors reduce Li+ clearance and predispose
to its toxicity.
Dose 25 mg BD, increased
gradually upto 50 mg TDS according to
response. In patients on diuretics and in CHF patients it is wise to start with
6.25 mg BD to avoid marked fall in BP initially. Tablets should be taken 1 hr
before or 2 hr after a meal. It has become less popular due to need for
twice/thrice daily dosing and possibly higher incidence of side effects
compared to other ACE inhibitors. ANGIOPRIL 25 mg tab, ACETEN, CAPOTRIL 12.5, 25
mg tab.
Other ACE Inhibitors
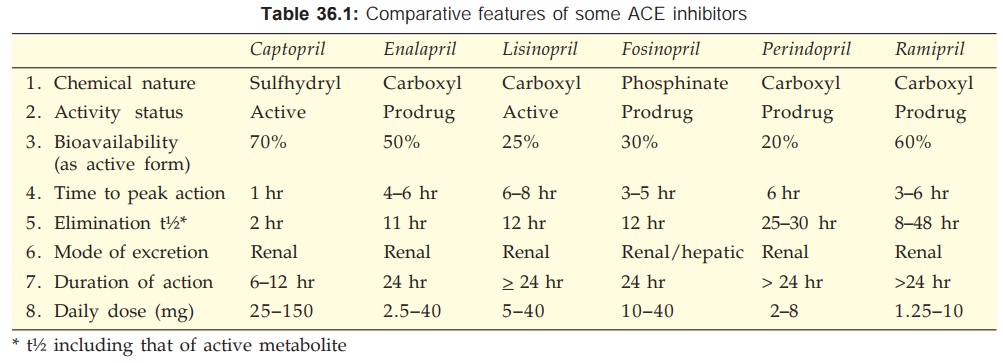
Differences among ACE inhibitors are primarily pharmacokinetic
reflected in time course of their action; no single drug is superior to others.
Enalapril
This is the second ACE inhibitor to be introduced. It is a
prodrug—converted in the body to enalaprilat
(a tripeptide analogue), which is not used as such orally because of poor
absorption, but is marketed as injectable preparation in some countries. Enalapril
has the same pharmacological, therapeutic and adverse effect profile as
captopril, but may offer certain advantages:
·
More potent, effective dose 5–20 mg OD or BD.
·
Its absorption is not affected by food.
·
Onset of action is slower (due to need for conversion
to active metabolite), less liable to cause abrupt first dose hypotension.
·
Has a longer duration of action: most hypertensives
can be treated with single daily dose.
·
Rashes and loss of taste are probably less frequent.
ENAPRIL, ENVAS, ENAM
2.5, 5, 10, 20 mg tab.
Lisinopril
It is the lysine
derivative of enalaprilat: does not require hydrolysis to become active ACE
inhibitor. Its oral absorption is slow (making first dose hypotension less
likely) and incomplete, but unaffected by food. The duration of action is
considerably longer, permitting single daily dose and ensuring uniform
hypotensive action round the clock. A reduction in venous return, cardiac
contractility and cardiac output has been noted after few weeks of lisinopril
use.
LINVAS, LISTRIL, LIPRIL 2.5, 5, 10 mg tab, LISORIL 2.5, 5, 10,
20 mg tab.
Perindopril
Another long-acting
ACE inhibitor with a slow onset of
action: less chance of first dose hypotension. Though 66–95% of orally
administered perindopril is absorbed, only about 20% is converted to the active
metabolite perindoprilat. Extensive
metabolism to other inactive products
occurs. Efficacy and tolerance of perindopril are similar to other ACE
inhibitors.
COVERSYL 2, 4 mg tab.
Fosinopril
This ACE inhibitor is
unique in being a phosphinate
compound that is glucuronide conjugated and eliminated both by liver and
kidney. The t½ is not altered by renal impairment; dose remains the same.
However, like most others, it is a prodrug suitable for once daily
administration. First dose hypotension is more likely.
Dose: Initially 10 mg
(elderly 5 mg) OD; maximum 40 mg/day.
FOSINACE, FOVAS 10, 20
mg tabs.
Trandolapril
It is a carboxyl
prodrug that is 40–60% bioavailable
in the active form. Absorption is delayed but not decreased by food. The peak
effect occurs at 4–6 hours. It is partly metabolized and eliminated both in
urine and faeces. The plasma t½ of active metabolite is 16– 24 hours, suitable
for once daily dosing.
Dose: 2–4 mg (max 8 mg) OD; ZETPRIL 1, 2 mg tabs.
Ramipril
The distinctive
feature of this long-acting ACE inhibitor is its extensive tissue distribution.
It may thus inhibit local RAS to a greater extent. Whether this confirs any
therapeutic advantage is not known. The plasma t½ of its active metabolite
ramiprilat is 8–18 hours, but terminel t½ is longer due to slow release of
tissue bound drug.
CARDACE, RAMIRIL,
CORPRIL, R.PRIL 1.25, 2.5, 5 mg caps.
Imidapril
The oral
bioavailability of this long-acting prodrug ACE inhibitor is 40%, that is
reduced by taking with meals. The peak effect occurs at 6–8 hours and plasma t½
is >24 hours.
Dose: Initially 5 mg OD taken
1 hour before food; usual maintenance
dose 10 mg OD.
TANATRIL 5, 10 mg
tabs.
Benazepril
Another non-sulfhydryl
prodrug ACE inhibitor; has a
bioavailability of 37% and is excreted by kidney with a t½ of 10–12 hr.
Dose: 10 mg initially, max
20–40 mg/day;
BENACE 5, 10, 20 mg tab.
Uses
Hypertension
The ACE inhibitors are
now first line drugs in
all grades of hypertension. About 50% patients of essential hypertension
respond to monotherapy with ACE inhibitors and majority of the rest to their
combination with diuretics or β blockers. The hypotensive effect of lower
doses develops gradually over 2–3 weeks. They offer the following advantages:
• Lack of postural hypotension, electrolyte disturbances,
feeling of weakness and CNS effects.
• Safety in asthmatics, diabetics and peripheral vascular
disease patients.
• Recent evidence indicates that long-term ACE inhibitor therapy
has the potential to reduce incidence of type 2 diabetes in high risk subjects.
• Prevention of secondary hyperaldosteronism and K+
loss due to diuretics.
• Renal blood flow is well maintained.
• They reverse left
ventricular hypertrophy and the increased walltolumen ratio of blood vessels
that occurs in hypertensive patients.
• No hyperuricaemia, no deleterious effect on plasma lipid
profile.
• No rebound hypertension on withdrawal.
• Minimum
worsening of quality
of life parameters like general
wellbeing, work performance, sleep, sexual performance, etc.
Large multicentric trials have confirmed that ACE inhibitors
reduce cardiovascular morbidity and increase life expectancy of hypertensive patients.
It appears that by their specific effect on myocardial and vascular cell
growth/remodeling, they have greater protective potential than other classes of
antihypertensive drugs.
ACE inhibitors are highly effective and first choice drugs in renovascular
and resistant hypertension. They are particularly suitable for diabetic hypertensives
in whom they reduce cardiovascular complications more than other
antihypertensive drugs, probably by improving endothelial function.
CHF
ACE inhibitors cause
both arteriolar and venodilatation in
CHF patients: reduce afterload as well as preload. Haemodynamic measurements in
severe CHF patients have shown reduction in right atrial pressure, pulmonary
arterial pressure, pulmonary capillary wedge pressure, systemic vascular
resistance, systolic wall stress and systemic BP. Though they have no direct
myocardial action, stroke volume and cardiac output are increased, while heart
rate is reduced. Accumulated salt and water are lost due to improved renal
perfusion and abolition of mineralocorticoid mediated Na+ retention.
Cardiac work as measured by heart rate × pressure product is reduced; thereby,
exercise capacity of CHF patients is enhanced. Beneficial effects are well sustained
with chronic therapy and the NYHA functional class of most patients is
improved.
Robust multicentric
trials have shown that ACE inhibitors retard the progression of left
ventricular systolic dysfunction and prolong survival of CHF patients of all
grades (I to IV). Unless contraindicated, ACE inhibitors are now advocated by
several professional bodies, including American Heart Association and American
College of Cardiology, as first line drugs in all patients with symptomatic as
well as asymptomatic left ventricular inadequacy. A diuretic, β blocker with or
without digitalis may be added according to need. ACE inhibitors reduce
episodes of decompensation, myocardial infarction and sudden death. In addition
to improved haemodynamics, long-term benefits of ACE inhibitors accrue from
withdrawal of AII mediated ventricular hypertrophy, remodeling, accelerated
myocyte apoptosis and fibrosis. Indirect benefits occur due to reduction in
sympathetic activation and aldosterone levels.
The Assessment of Treatment
with Lisinopril and Survival (ATLAS) trial on 3164 heart failure patients (NYHA
class II to IV) has shown that high dose lisinopril (32.5–35 mg/ day) given for
39–58 months was more effective in reducing all cause mortality,
hospitalization for heart failure and risk of MI than lower dose (2.5–5
mg/day). To afford maximum protection against progression of heart failure, the
dose of ACE inhibitors needs to be titrated to nearly the upper limit of
recommended dose range, as shown in other mega trials like GISSI3, SOLVD, AIRE,
etc. as well. ACE inhibitors are effective in reducing development of
ventricular dysfunction, heart failure and related mortality in post-MI
patients also (SAVE, TRACE, AIRE trials).
Myocardial Infarction (MI)
Several megatrials have established that oral ACE inhibitors
administered while MI is evolving (within 24 hr of an attack) and continued for
6 weeks reduce early as well as long-term mortality, irrespective of presence
or absence of systolic dysfunction, provided hypotension is avoided. In high
risk patients and those with latent or overt ventricular dysfunction (CHF)
extension of therapy continues to afford survival benefit over years. In
unstable angina/non-ST segment elevation MI, long-term ACE inhibitor therapy reduces
recurrent MI and need for coronary angioplasty (SAVE and SOLVD trials), though
no benefit was apparent in the shortterm (ISIS4 study). Current evidence shows
that if there are no contraindications, all MI patients stand to gain from ACE
inhibitor therapy, though magnitude of benefit is greatest in those having
associated hypertension and/or diabetes.
Prophylaxis
In High Cardiovascular Risk Subjects
The results of Heart
Outcomes Prevention Evaluation
(HOPE) study in 9297 post-MI and other high risk subjects, but having no left ventricular
dysfunction or heart failure have shown that ramipril reduced cardiac death and
MI or stroke by 22% over a period of 4.5 years. Risk of developing heart
failure or diabetes was also reduced. These results have been confirmed by the EUROPA
trial and appear to hold true even for patients who have undergone coronary
revascularization (APRES trial). Thus, ACE inhibitors are protective in high
cardiovascular risk subjects even when there is no associated hypertension or left
ventricular dysfunction. Protective effect is exerted both on myocardium as
well as vasculature, may involve improved endothelial function, and is
independent of hypotensive action.
Diabetic Nephropathy
Prolonged ACE inhibitor therapy has been found to prevent or
delay endstage renal disease in type I as well as type II diabetics.
Albuminuria (an index of glomerulopathy) remains stable in those treated with
ACE inhibitor, but aggravates in untreated diabetics. Treated patients have
higher creatinine clearance, require less dialysis and have longer life
expectancy. Benefits appear to be due to haemodynamic (systemic and intrarenal)
as well as abnormal mesangial cell growth attenuating effects of ACE
inhibitors. They reduce intraglomerular pressure and hyperfiltration. ACE
inhibitors arrest/partly reverse any degree of albuminuria, but benefits are
restricted after macroalbuminuria in type 2 diabetes has set in. The RAS seems
to accentuate micro and macrovascular complications in diabetics, and ACE inhibitors
have specific organ protective effect by attenuating the same. Deterioration of
retinopathy in diabetics also appears to be retarded by ACE inhibitors. All
patients with diabetic nephropathy, whether hypertensive or normotensive,
deserve ACE inhibitor therapy.
Non-diabetic Nephropathy
There is evidence now that chronic renal failure due to nondiabetic
causes may also be improved by ACE inhibitors. They reduce proteinuria by
decreasing pressure gradient across glomerular capillaries as well as by altering
membrane permeability. This retards disease progression. Among hypertensive nephropathy
patients the incidence of doubling of serum creatinine or end stage renal
failure is significantly lower in those treated with ACE inhibitors than those
treated with other antihypertensives.
Scleroderma Crisis
The marked rise in BP and deterioration of renal function in
scleroderma crisis is mediated by AII. ACE inhibitors produce dramatic
improvement and are life saving in this condition.
Captopril Test
This test has been devised
to obviate the need for renal
angiography for diagnosis of renovascular hypertension. The basis of the test
is—acute blockade of AII formation by captopril results in a reactive increase
in PRA which is much higher in renovascular compared to essential hypertension.
However, this test is only of adjunctive value.
Related Topics
