Coagulants
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs Affecting Coagulation, Bleeding And Thrombosis
These are substances which promote coagulation, and are indicated in haemorrhagic states.
COAGULANTS
These are substances
which promote coagulation, and are indicated in haemorrhagic states.
Fresh whole blood or
plasma provide all the factors needed for coagulation and are the best therapy
for deficiency of any clotting factor; also they act immediately. Other drugs
used to restore haemostasis are:
1. Vitamin K
K1 (from
plants, : Phytonadione
fatsoluble) (Phylloquinone)
K3
(synthetic)
Fatsoluble
: Menadione, Acetomenaphthone
Watersoluble : Menadione sod. Bisulfite
: Menadione sod. diphosphate
2. Miscellaneous
Fibrinogen (human)
Antihaemophilic factor
Desmopressin
Adrenochrome monosemicarbazone
Rutin,
Ethamsylate
VITAMIN K
It is a fatsoluble
dietary principle required for the synthesis of clotting factors.
Dam (1929) produced
bleeding disorder in chicken by feeding deficient diet. This was later found to
be due to decreased concentration of prothrombin in blood and that it could be
cured by a fat soluble fraction of hog liver. This factor was called Koagulations vitamin (vit K) and soon
its structure was worked out. A similar vitamin was isolated in 1939 from
alfalfa grass and labelled vit K1, while that from sardine (sea
fish) meal was labelled K2. Synthetic compounds have been produced
and labelled K3.
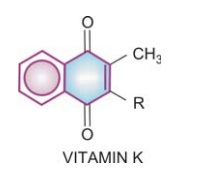
Chemistry And Source
Vit K has a basic
naphthoquinone structure, with or
without a side chain (R) at position 3. The side chain in K1 is phytyl, in K2 prenyl, while in K3 there is
no side chain.
Dietary sources
are—green leafy vegetables, such as cabbage, spinach; and liver, cheese, etc.
Daily Requirement
It is uncertain, because a variable amount of menaquinone
(vit K2) produced by colonic bacteria becomes available. Even 3–10 μg/day external source
may be sufficient. However, the total requirement of an adult has been
estimated to be 50–100 μg/day.
Action
Vit K acts as a cofactor at a late stage in the synthesis by liver of coagulation proteins— prothrombin, factors VII, IX and X. The vit K dependent change (γ carboxylation of glutamate residues of these zymogen proteins; see Fig. 44.2) confers on them the capacity to bind Ca2+ and to get bound to phospholipid surfaces—properties essential for participation in the coagulation cascade.
Utilization
Fat-soluble forms of
vit K are absorbed from the
intestine via lymph and require bile
salts for absorption, while water-soluble forms are absorbed directly into portal
blood. An active transport process in the jejunum has been demonstrated for K1,
while K2 and K3 are absorbed by simple diffusion. Vit K
is only temporarily concentrated in liver, but there are no significant stores
in the body. It is metabolized in liver by side chain cleavage and glucuronide
conjugation; metabolites are excreted in bile and urine.
Deficiency
Deficiency of vit K occurs due to liver disease, obstructive jaundice, malabsorption, long-term
antimicrobial therapy which alters intestinal flora. However, deficient diet is
rarely responsible. The most important manifestation is bleeding tendency due
to lowering of the levels of prothrombin and other clotting factors in blood.
Haematuria is usually first to occur; other common sites of bleeding are
g.i.t., nose and under the skin—ecchymoses.
Preparations
Phytonadione: VITAMINK, KENADION 10
mg/ml for i.m. injection.
Menadione: 0.66 mg in GYNAE CVP
with vit C 75 mg, ferrous gluconate 67 mg, Cal. lactate 300 mg and citras
bioflavonoid 150 mg per cap:
Acetomenaphthone: ACETOMENADIONE 5, 10 mg tab; KAPILIN 10 mg tab.
Menadione sod.
bisulfite: 20 mg, in CADISPERC with vit C 100 mg, adrenochrome
monosemicarbazone, 1 mg, rutin 60 mg, methylhesperidin 40 mg, Cal. phosphate
100 mg per tab.
STYPTOCID 10 mg with
adrenochrome monosemicarbazone 0.5 mg, rutin 50 mg, vit C 37.5 mg, vit D 200
i.u., Cal. phosphate 260 mg per tab.
Use
The only use of vit K
is in prophylaxis and treatment of bleeding
due to deficiency of clotting factors in the following situations:
a)
Dietary Deficiency: of vit K is very rare in adults. However, when it occurs 5–10 mg/day
oral or parenteral vit K rapidly corrects the defects.
b) Prolonged Antimicrobial Therapy: treat in the same way as dietary deficiency of vit K.
c) Obstructive Jaundice
Or Malabsorption Syndromes (sprue, regional
ileitis, steatorrhoea, etc.): vit K 10 mg i.m./day, or orally along with bile
salts.
d) Liver Disease (Cirrhosis, Viral
Hepatitis): associated bleeding responds poorly to vit K. Because of hepatocellular
damage, synthesis of clotting factors is inadequate despite the presence of vit
K. However, vit K may be of some use if its absorption had been affected due to
lack of bile salts.
e)
Newborns: All newborns have low
levels of prothrombin and other clotting
factors. Further decrease occurs in the next few days. The cause is both lower
capacity to synthesize clotting factors as well as deficiency of vit K. The
defect is exaggerated in the premature infant. Vit K 1 mg i.m. soon after birth
has been recommended routinely. Some prefer administering 5–10 mg i.m. to the
mother 4–12 hours before delivery. Haemorrhagic disease of the newborn can be
effectively prevented/treated by such medication.
Menadione (K3)
should not be used for this purpose (see
below).
f)
Overdose Of Oral
Anticoagulants: This is the most important indication of vit K.
Phytonadione (K1) is the preparation of choice, because it acts most
rapidly; dose depends on the severity of hypo-prothrombinaemia (measured INR)
and bleeding. Unnecessary high dose is to be avoided because it will render the
patient unresponsive to oral anticoagulants for several days.
Severe: 10 mg i.m. followed
by 5 mg 4 hourly; bleeding generally
stops in 6–12 hours, but normal levels of coagulation factors are restored only
after 24 hr. This dose of vit-K will block anticoagulant action for 7–10 days.
Moderate: 10 mg i.m. followed
by 5 mg once or twice according to
response.
Mild: Just omit a few doses
of the anticoagulant.
g) Prolonged high dose
salicylate therapy causes hypoprothrombinemia; vit K should be given
prophylactically. If bleeding occurs—treat as for oral anticoagulants.
Toxicity
Rapid i.v. injection of emulsified vit K produces flushing, breathlessness, a sense of
constriction in the chest, fall in BP; few deaths are on record. It is probably
due to emulsion form of the preparation.
Menadione and its watersoluble derivatives can cause haemolysis
in a dosedependent manner. Patients with G6PD deficiency and neonates are
especially susceptible. In the newborn menadione or its salts can precipitate
kernicterus:
·
by inducing haemolysis and increasing
bilirubin load.
·
by competitively inhibiting glucuronidation of
bilirubin. Glucuronide conjugation is, as such, inadequate in neonates.
Because of poor efficacy and higher toxicity, there is little
justification to use menadione and its water-soluble salts for any indication.
Fibrinogen
The fibrinogen fraction of human plasma is employed to control bleeding in haemophilia,
antihaemophilic globulin (AHG) deficiency and acute afibrinogenemic states; 0.5
g is infused i.v.
FIBRINAL 0.5 g/bottle
for i.v. infusion.
Antihaemophilic Factor
It is concentrated human AHG prepared from pooled
human plasma. It is indicated (along with human fibrinogen) in haemophilia and
AHG deficiency. It is highly effective in controlling bleeding episodes, but
action is shortlasting (1 to 2 days).
Dose: 5–10 U/kg by i.v.
infusion, repeated 6–12 hourly.
FIBRINALH, ANTIHAEMOPHILIC FACTOR: 150 U or 200 U + fibrinogen
0.5 g/bottle for i.v. infusion.
Desmopressin
It releases factor
VIII and von Willebrand’s factor from vascular
endothelium and checks bleeding in haemophilia and von Willebrand’s disease.
Adrenochrome Monosemicarbazone
It is believed to reduce capillary fragility,
control oozing from raw surfaces and prevent microvessel bleeding, e.g.
epistaxis, haematuria, retinal haemorrhage, secondary haemorrhage from wounds,
etc. Its efficacy is uncertain.
Dose: 1–5 mg oral, i.m.
STYPTOCHROME 3 mg/2 ml
inj., STYPTOCID: 2 mg/2 ml inj; in CADISPERC, STYPTOCID 1 mg, 0.5 mg tab, with
other ingredients.
Rutin
It is a plant
glycoside claimed to reduce capillary bleeding. It has been
used in a dose of 60 mg oral BD–TDS along with vit C which is believed to
facilitate its action. Its efficacy is uncertain.
In CADISPERC 60 mg
tab, in KERUTINC 100 mg tab, in STYPTOBION 100 mg tab, 200 mg/2 ml inj.
Ethamsylate
It reduces capillary
bleeding when platelets are adequate; probably
exerts anti-hyaluronidase action— improves capillary wall stability, but does
not stabilize fibrin (not an antifibrinolytic). Ethamsylate has been used in
the prevention and treatment of capillary bleeding in menorrhagia, after
abortion, PPH, epistaxis, malena, hematuria and after tooth extraction, but efficacy
is unsubstantiated. Side effects are nausea, rash, headache, and fall in BP
(only after i.v. injection).
Dose: 250–500 mg TDS oral/i.v.; ETHAMSYL, DICYNENE, HEMSYL, K. STAT 250, 500 mg tabs; 250 mg/2 ml
inj.
LOCAL HAEMOSTATICS (STYPTICS)
After injury to
arterioles and other smaller blood vessels, normal haemostasis occurs
successively by contraction of injured vessel wall (lasting few minutes),
adhesion and aggregation of platelets to form a plug, formation of a blood
clot, and finally in due course dissolution of the clot by fibrinolysis.
External bleeding is usually stopped by manual pressure, cotton gauze pressure
pack or by suturing. Control of bleeding may be aided by local haemostatics (styptics) that are substances used to stop
bleeding from a local and approachable site. They are particularly effective on
oozing surfaces, e.g. tooth socket, abrasions, etc. Absorbable materials like fibrin (prepared from human plasma and
dryed as sheet or foam), gelatin foam,
oxidized cellulose (as strips which can
be cut and placed in the wound) provide a meshwork which activates the
clotting mechanism and checks bleeding. Left in situ these materials are absorbed in 1–4 weeks and generally
cause no foreign body reaction. Thrombin obtained
from bovine plasma may be applied as
dry powder or freshly prepared solution to the bleeding surface in
haemophiliacs.
Vasoconstrictors like 0.1% Adr solution may be soaked in sterile cotton gauze and
packed in the bleeding tooth socket or nose in case of epistaxis to check bleeding
when spontaneous vasoconstriction is inadequate. Astringents such as tannic acid or metallic salts are occasionally
applied for bleeding gums, bleeding piles, etc.
SCLEROSING AGENTS
These are irritants, cause inflammation, coagulation and ultimately
fibrosis, when injected into haemorrhoids (piles) or varicose vein mass. They
are used only for local injection.
1. Phenol (5%) in almond oil or peanut oil: 2–5 ml.
2. Ethanolamine
oleate (5% in 25% glycerine and 2% benzyl alcohol): 1–5 ml inj.
3. Sod. tetradecyl sulfate (3% with benzyl alcohol
2%): 0.5–2 ml at each site. SETROL 2 ml inj.
4. Polidocanol (3% inj): 2 ml; ASKLEROL 2 ml inj.
