Maturation Factors - Vit B12 and Folic Acid
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs Affecting Blood And Blood Formation
Deficiency of vit B12 and folic acid, which are B group vitamins, results in megaloblastic anaemia characterized by the presence of large red cell precursors in bone marrow and their large and short-lived progeny in peripheral blood.
MATURATION FACTORS
Deficiency of vit B12 and folic acid, which are B group vitamins, results in megaloblastic
anaemia characterized by the presence of large red cell precursors in bone
marrow and their large and short-lived progeny in peripheral blood. Vit B12 and
folic acid are therefore called maturation factors. The basic defect is in DNA
synthesis. Apart from haemopoietic, other rapidly proliferating tissues also suffer.
VITAMIN-B12
Cyanocobalamin and hydroxocobalamin are complex cobalt
containing compounds present in the diet and referred to as vit B12.
Thomas Addison (1849)
described cases of anaemia not responding to iron. This was later called
‘pernicious’ (incurable, deadly) anaemia and its relation with atrophy of
gastric mucosa was realized. Minot and Murphy (1926) treated such patients by
including liver in diet and received Nobel prize. Castle (1927–32) propounded
the hypothesis that there was an extrinsic
factor present in diet which combined with an intrinsic factor produced by stomach to give rise to the haemopoietic principle. Vit B12 was
isolated in 1948 and was shown to be the extrinsic factor as well as the
haemopoietic principle, the intrinsic factor only helped in its absorption.
Vit B12 occurs as
water soluble, thermostable red crystals. It is synthesized in nature only by
microorganisms; plants and animals acquire it from them.
Dietary sources Liver, kidney, sea
fish, egg yolk, meat, cheese are the
main vit B12 containing constituents of diet. The only vegetable source is
legumes (pulses) which get it from microorganisms harboured in their root
nodules.
Vit B12 is synthesized
by the colonic microflora but this is not available for absorption in man. The
commercial source is Streptomyces griseus;
as a byproduct of streptomycin industry.
Daily requirement: 1–3 μg, pregnancy and lactation 3–5 μg.
Metabolic Functions
Vit B12 is intricately linked with folate metabolism in many ways; megaloblastic
anaemia occurring due to deficiency of either is indistinguishable. In
addition, vit B 12 has some independent metabolic functions as well. The active
coenzyme forms of B12 generated in the body are deoxyadenosylcobalamin (DAB12) and methylcobalamin (methyl
B12).
(i) Vit B12 is essential
for the conversion of homocysteine to methionine
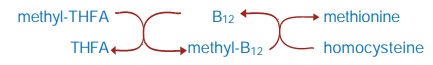
Methionine is needed
as a methyl group donor in many metabolic reactions and for protein synthesis.
This reaction is also critical in making tetrahydrofolic acid (THFA) available
for reutilization. In B12 deficiency THFA gets trapped in the methyl form and a
number of one carbon transfer
reactions suffer (see under folic
acid).
(ii) Purine and
pyrimidine synthesis is affected primarily due to defective ‘one carbon’
transfer because of ‘folate trap’. The most important of these is inavailability
of thymidylate for DNA
production.

This is an important
step in propionic acid metabolism. It links the carbohydrate and lipid
metabolisms. This reaction does not require folate and has been considered to
be responsible for demyelination seen in B12 deficiency, but not in pure folate
deficiency. That myelin is lipoidal, supports this contention.
(iv) Now it appears
that interference with the reaction:

may be more important
in the neurological damage of B12 deficiency, because it is needed in the
synthesis of phospholipids and myelin.
(v) Vit B12 is essential
for cell growth and multiplication.
Utilization OF Vit B12
Vit B12 is present in food as protein conjugates
and is released by cooking or by proteolysis in stomach facilitated by gastric
acid. Intrinsic factor (a glycoprotein, MW60,000) secreted by stomach forms a complex
with B12— attaches to specific receptors present on intestinal mucosal cells
and is absorbed by active carrier mediated transport. This mechanism is
essential for absorption of vit B12 ingested in physiological amounts. However,
when gross excess is taken, a small fraction is absorbed without the help of
intrinsic factor.
Vit B12 is transported in blood in combination with a specific β globulin transcobalamin II (TCII). Congenital
absence of TCII or presence of abnormal protein (TCI or TCIII, in liver and
bone marrow disease) may interfere with delivery of vit B12 to tissues. Vit B
12 is especially taken up by liver cells and stored: about 2/3 to 4/5 of body’s
content (2–8 mg) is present in liver.
Vit B12 is not
degraded in the body. It is excreted mainly in bile (3–7 μg/day); all but 0.5– 1
μg of this is
reabsorbed—considerable enterohepatic circulation occurs. Thus, in the absence
of intrinsic factor or when there is malabsorption, B12 deficiency develops
much more rapidly than when it is due to nutritional deficiency. It takes 3–5
years of total absence of B12 in diet to deplete normal body stores.
Vit B12 is directly and completely absorbed after i.m. or deep
s.c. injection. Normally, only traces of B12 are excreted in urine, but when
pharmacological doses (> 100 μg) are given orally or parenterally—a large
part is excreted in urine, because the plasma protein binding sites get saturated
and free vit B12 is filtered at the glomerulus. Hydroxocobalamin is more
protein bound and better retained than cyanocobalamin.
Deficiency
Vit B12 deficiency
occurs due to:
1. Addisonian
pernicious anaemia: is probably an autoimmune disorder which results in
destruction of gastric parietal cells → absence of intrinsic factor in gastric juice
(along with achlorhydria) → inability to absorb vit B12.
2. Other causes of gastric mucosal damage, e.g. chronic
gastritis, gastric carcinoma, gastrectomy, etc.
3. Malabsorption (damaged intestinal mucosa), bowel resection.
4. Consumption of vit
B12 by abnormal flora in intestine (blind loop syndrome) or fish tape worm.
5. Nutritional deficiency: less common cause.
6. Increased demand: pregnancy, infancy.
Manifestations of deficiency are:
· Megaloblastic anaemia (generally the first
manifestation), neutrophils with hypersegmented nuclei, giant platelets.
·
Glossitis, g.i. disturbances: damage to epithelial
structures.
· Neurological: subacute combined degeneration
of spinal cord; peripheral neuritis—diminished vibration and position sense,
paresthesias, depressed stretch reflexes; mental changes— poor memory, mood
changes, hallucinations, etc. are late effects.
Preparations, Dose, Administration
Cyanocobalamin: REDISOL,
MACRABIN 35 μg/5 ml liq; 100, 500, 1000 μg inj.
Hydroxocobalamin: REDISOLH, MACRABINH
500, 1000 μg inj.
Methylcobalamin: BIOCOBAL, DIACOBAL, METHYLCOBAL
0.5 mg tab.
Methyl B12
is the active coenzyme form of vit B12 for synthesis of methionine and Sadenosyl-methionine
that is needed for integrity of myelin. This preparation of vit B12 in a dose
of 1.5 mg/ day has been especially promoted for correcting the neurological
defects in diabetic, alcoholic and other forms of peripheral neuropathy.
However, in USA and many other countries, it is used only as a nutritional
supplement, and not as a drug.
Combination
preparations of B12 with other vitamins and iron are listed in Tables 43.1 and
67.2. Hydroxocobalamin has been preferred for parenteral use because of better
retention. However, it has been found to induce antibody formation so that vit
B12 becomes metabolically unavailable. It is not recommended in USA,
but used in UK and India.
When vit B12
deficiency is due to lack of intrinsic factor (pernicious anaemia and other
causes), it should be given by i.m. or deep s.c. (but not i.v.) injection.
Parenteral administration is necessary to bypass the defective absorptive
mechanism. Initially 30–100 μg/day for 10 days followed by 100 μg weekly and then
monthly for maintenance—indefinitely or lifelong. When neurological
complications are present, a higher dose (500–1000 μg/day) has been used,
but the response is not superior to conventional doses.
In other types of
deficiency 10–30 μg/day may be used orally. The prophylactic dose is 3–10 μg/ day.
Uses
1. Treatment of vit
B12 deficiency: vit B12 is used as outlined above. It is wise to add 1–5 mg of
oral folic acid and an iron preparation, because reinstitution of brisk
haemopoiesis may unmask deficiency of these factors. Response to vit B12 is
dramatic—symptomatic improvement starts in 2 days: appetite improves, patient
feels better; mucosal lesions heal in 1–2 weeks; reticulocyte count increases;
Hb% and haematocrit rise progressively; platelet count normalises in 10 days
and WBC count in 2–3 weeks. Time taken for complete recovery of anaemia depends
on the severity of disease to start with. Neurological parameters improve more
slowly—may take several months; full recovery may not occur if vit B12
deficiency has been severe or had persisted for long.
2. Prophylaxis: needs to be given only when there are definite
predisposing factors for development of deficiency (see above).
3. Mega doses of vit
B12 have been used in neuropathies, psychiatric disorders, cutaneous sarcoid
and as a general tonic to allay fatigue, improve growth—value is questionable.
4. Tobacco amblyopia: hydroxocobalamin is of some benefit—it
probably traps cyanide derived from tobacco to form cyanocobalamin.
Adverse Effects
Even large doses of
vit B12 are quite safe. Allergic reactions have occurred
on injection, probably due to contaminants. Anaphylactoid reactions (probably
to sulfite contained in the formulation) have occurred on i.v. injection: this
route should not be employed.
FOLIC ACID
It occurs as yellow crystals which are insoluble in water, but
its sodium salt is freely water soluble. Chemically it is Pteroyl glutamic acid (PGA) consisting of pteridine + para-amino benzoic
acid (PABA) + glutamic acid.
Wills (1932–37) had
found that liver extract contained a factor, other than vit B12, which could
cure megaloblastic anaemia. Mitchell in 1941 isolated an anti-anaemia principle
from spinach and called it ‘folic acid’ (from leaf). Later the Will’s factor
was shown to be identical to folic acid.
Dietary Sources Liver, green leafy
vegetables (spinach), egg, meat, milk. It is
synthesized by gut flora, but this is largely unavailable for absorption.
Daily Requirement of an adult is <
0.1 mg but dietary allowance of
0.2 mg/day is recommended. During pregnancy, lactation or any condition of high
metabolic activity, 0.8 mg/ day is considered appropriate.
Utilization
Folic acid is present
in food as polyglutamates; the additional glutamate residues are split off
primarily in the upper intestine before being absorbed. Reduction to DHFA and
methylation also occurs at this site. It is transported in blood mostly as
methyl-THFA which is partly bound to plasma proteins. Small, physiological
amounts of folate are absorbed by specific carrier mediated active transport in
the intestinal mucosa. Large pharmacological doses may gain entry by passive
diffusion, but only a fraction is absorbed.
Folic acid is rapidly
extracted by tissues and stored in cells as polyglutamates. Liver takes up a
large part and secretes methyl-THFA in bile which is mostly reabsorbed from
intestine: enterohepatic circulation occurs. Alcohol interferes with release of
methyl-THFA from hepatocytes. The total body store of folates is 5–10 mg.
Normally, only traces are excreted, but when pharmacological doses are given,
50–90% of a dose may be excreted in urine.
Metabolic Functions
Folic acid is inactive
as such and is reduced to
the coenzyme form in two steps: FA → DHFA → THFA by folate reductase
(FRase) and dihydrofolate reductase (DHFRase). THFA mediates a number of one carbon transfer reactions by
carrying a methyl group as an adduct (see
under vit. B12 also).
1. Conversion of
homocysteine to methionine: vit B12 acts as an intermediary carrier of methyl
group. This is the most important reaction which releases THFA from the
methylated form.
2. Generation of
thymidylate, an essential constituent of DNA:
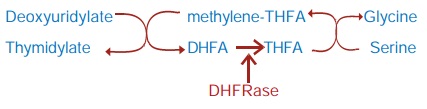
3. Conversion of
serine to glycine: needs THFA and results in the formation of methylene-THFA
which is utilized in thymidylate synthesis.
4. Purine synthesis: de novo building of purine ring requires
formyl-THFA and methenyl-THFA (generated from methylene-THFA) to introduce
carbon units at position 2 and 8.
5. Generation and
utilization of ‘formate pool’.
6. Histidine
metabolism: for mediating formimino group transfer.
Ascorbic acid protects
folates in the reduced form. Other cofactors, e.g. pyridoxal, etc. are required
for some of the above reactions.
Deficiency
Folate deficiency
occurs due to:
·
Inadequate dietary intake
· Malabsorption: especially involving upper
intestine— coeliac disease, tropical sprue, regional ileitis, etc. Deficiency
develops more rapidly as both dietary and biliary folate is not absorbed.
·
Biliary fistula; bile containing folate for
recirculation is drained.
· Chronic alcoholism: intake of folate is
generally poor. Moreover, its release from liver cells and recirculation are
interfered.
· Increased demand: pregnancy, lactation, rapid
growth periods, haemolytic anaemia and other diseases with high cell turnover
rates.
· Drug induced: prolonged therapy with anticonvulsants
(phenytoin, phenobarbitone, primidone) and oral contraceptives—interfere with
absorption and storage of folate.
Manifestations Of Deficiency Are:
· Megaloblastic anaemia, indistinguishable from
that due to vit B12 deficiency. However, folate deficiency develops more
rapidly if external supply is cut off: body stores last 3–4 months only. In
malabsorptive conditions megaloblastosis may appear in weeks.
·
Epithelial damage: glossitis, enteritis, diarrhoea,
steatorrhoea.
· Neural tube defects, including spina bifida in
the offspring, due to maternal folate deficiency.
· General debility, weight loss, sterility. However,
neurological symptoms do not appear in pure folate deficiency.
Preparations And Dose
Folic acid: FOLVITE, FOLITAB 5 mg
tab;
Liquid oral
preparations and injectables are available only in combination formulation (see Tables 43.1 and 67.2). Oral therapy
is adequate except when malabsorption is present or in severely ill
patient—given i.m.
Dose: therapeutic 2 to 5
mg/day, prophylactic 0.5 mg/ day.
Folinic acid; CALCIUM LEUCOVORIN 3
mg/ml inj.
FASTOVORIN 3 mg, 15 mg
amps, 50 mg vial; RECOVORIN 15 mg tab, 15 mg, 50 mg vial for inj.
Uses
1. Megaloblastic
Anaemias due to:
· Nutritional folate deficiency; manifests earlier
than vit B12 deficiency. Response occurs as quickly as with vit B12.
·
Increased demand: pregnancy, lactation,
infancy, during treatment of severe iron deficiency anaemia, haemolytic
anaemias.
· Pernicious anaemia: folate stores may be low
and deficiency may be unmasked when vit B12 induces brisk haemopoiesis: it has
only secondary and adjuvant role in this condition.
· Folic acid should never be given alone to patients
with vit B12 deficiency—haematological response may occur, but neurological
defect may progress due to diversion of meagre amount of vit B12 present in
body to haemopoiesis.
· Malabsorption syndromes: Tropical sprue,
coeliac disease, idiopathic steatorrhoea, etc.
· Antiepileptic therapy: Megaloblastic anaemia
can occur due to prolonged phenytoin/ phenobarbitone therapy (see Ch. No. 30). This is treated by
folic acid, but large doses should be avoided as they may antagonize
anticonvulsant effect.
2. Prophylaxis of folate deficiency:
Only when definite predisposing
factors are present. Routine folate supplementation (1 mg/day) is recommended
during pregnancy to reduce the risk of neural tube defects in the newborn.
3. Methotrexate Toxicity
Folinic acid (Leucovorin, citrovorum factor, 5formylTHFA) is an
active coenzyme form which does not need to be reduced by DHFRase before it can
act. Methotrexate is a DHFRase inhibitor; its toxicity is not counteracted by
folic acid, but antagonized by folinic acid.
Folinic acid is expensive and not needed for the correction of
simple folate deficiency for which folic acid is good enough.
4. Citrovorum Factor Rescue
In certain malignancies,
high dose of methotrexate is injected i.v. and is followed within ½–1 hour with
1–3 mg i.v. of folinic acid to rescue the normal cells. It is ineffective if
given > 3 hours after methotrexate.
Adverse Effects
Oral folic acid is entirely nontoxic. Injections
rarely cause sensitivity reactions.
Shotgun Antianaemia Preparations
A large number of formulations containing varying quantities
of iron, vit B12, folic acid and may be other vitamins and nutrients
are marketed and promoted. They are liable to be used indiscriminately without
proper assessment of needs of the patient, and investigating the cause of
anaemia. Most preparations contain one or all ingredients in low amounts; thus,
an incomplete response can occur. Diagnosis and assessment of the patient can
become impossible thereafter.
