Disorders of Erythrocytes
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Blood
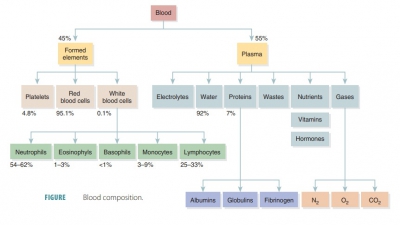
The majority of erythrocyte disorders are classified as either anemia or polycythemia. There are a variety of anemias, and fewer varieties of polycythemias.
Disorders
of Erythrocytes
The majority of erythrocyte disorders are classified as
either anemia or polycythemia. There are a variety of anemias, and fewer varieties
of polycythemias.
Anemias
The term anemia signifies
the blood having an ability to carry oxygen that is too low for normal
metabo-lism. This is not an actual disease, but a sign of some type of
disorder. When a person is anemic, he or she is chilled, fatigued, short of
breath, and often pale. The three causes of anemia include blood loss,
insufficient production of red blood cells, or excessive destruction of red
blood cells.
Blood Loss
Blood loss causes hemorrhagic anemia. When this condition is acute,
blood loss is very rapid, and is treated by replacing this depleted blood.
Chronic hemorrhagic anemia may be caused by small amounts of blood being lost,
but on a persistent basis, such as from a bleeding ulcer or because of
hemorrhoids. After the primary condition is resolved, lost blood cells can be
replaced by normal erythropoiesis. After losing a fair amount of blood, there
would be an increased reticulocyte count.
Insufficient Production of Red Blood Cells
There are a variety of causes that result in insufficient production
of RBCs, including total failure of red bone marrow function, and lack of
essential raw mate-rials such as iron.
■■ Aplastic anemia—red bone marrow destructionor inhibition because of chemicals,
drugs, ioniz-ing radiation, viruses, or most commonly from an unknown cause.
Since all formed elements expe-rience altered development, anemia is usually
present along with defective blood clotting and immunity. Blood transfusions
may be beneficial until stem cells can be harvested from a donor’s blood or
bone marrow, or if umbilical cord blood can be transplanted.
■■ Pernicious anemia—an autoimmune diseasethat is most common in the elderly, in which
the stomach mucosa is destroyed by their own immune systems. In order for
intestinal cells to absorb vitamin B12 require intrinsic factor, which is produced by the mucosal
cells of the stomach. Developing erythrocytes can grow but not divide without
vitamin B12. This causes large, pale cells to develop, which are
known as macro-cytes. Treatment of
pernicious anemia requiresregular intramuscular vitamin B12
injections, or a nasal application of a gel containing this vitamin, once weekly.
Also, a lack of dietary vitamin B12 can cause anemia, but this
usually only occurs in strict vegetarians, since this vitamin is found in large
amounts in fish, poultry, and other meats.
■■ Iron-deficiency anemia—this form of anemiausually follows hemorrhagic
anemia, but may also occur because of inadequate dietary iron or impaired
absorption of iron. Microcytes are
pro-duced, which are a type of erythrocytes that are small and pale, due to
their inability of synthesizing normal amounts of hemoglobin. Iron-deficiency
anemia is treated by increasing dietary iron or by taking iron supplements.
■■ Renal anemia—this form of anemia is causedby lack of erythropoietin (EPO),
which controls production of red blood cells. It often occurs because of renal
disease, in which the kidneys cannot produce enough EPO. Treatment involves the
administration of synthetic EPO.
Excessive Destruction of Red Blood Cells
Hemolytic
anemias involve premature rupture or lysisof erythrocytes. Causes
include abnormal hemo-globin, certain bacterial or parasitic infections, and
transfusions of mismatched blood. When abnormal hemoglobin is produced, there
is usually a genetic cause. The two primary examples are thalassemias and sickle-cell
anemia, which are serious disorders that may be incurable and fatal. These
diseases involve abnormal globin and erythrocytes that are fragile, which
rupture prematurely.
■■ Thalassemias — most
common in people of Mediterranean ancestry, these conditions involve one globin
chain that is absent or has abnormal function. Erythrocytes have less
hemoglobin than normal, and appear thin and delicate. A large variety of
thalassemias occur, which are classified by their hemoglobin chains that are
affected, and where in the chains that this occurs. Some are mild, while others
are so severe that they require monthly blood transfusions.
■■ Sickle cell anemia—
because of a change in one of the 146 amino acids of a beta chain in the
globin molecule, abnormal hemoglobin S (HbS) is formed. When low-oxygen
conditions exist, the beta chains link together, forming stiff rods. The
hemoglobin S becomes sharp and has “spikes.” This causes RBCs to adopt a
crescent shape when they deliver molecules of oxygen, or when oxygen content of
the blood is low, such as during vigorous exercise. The deformed erythrocytes
easily rupture and often block small blood vessels. This interferes with
delivery of oxygen, causing severe bone and chest pain, other severe pain, and
impaired breathing. Infections and stroke often result. For acute sickle-cell
crisis,blood transfusions are still performed regularly.A newer treatment
involves inhalation of nitric oxide to dilate the blood vessels. Sickle cell
anemia mostly affects Africans living in areas of that country where malaria
occurs regularly, and their descendants. Nearly one of every 00 African
-American babies has this disease.
Individuals with two copies of the sickle cell gene have
sickle-cell anemia, but those with only one copy of the gene have sickle-cell
trait, and are more likely to survive malaria. The cells only sickle when the
individual is infected with malaria, or under other abnormal situations. The
sickling reduces likelihood of the malaria para-sites’ survival. It also
increases the ability of mac-rophages to destroy infected RBCs and parasites
inside them. Treatments focus on preventing RBCs from sickling. For example,
fetal hemoglo-bin (HbF) does not sickle, even in people likely to develop
sickle-cell anemia. Therefore, hydroxy-urea can be administered, since it
causes the fetal hemoglobin gene to activate. This greatly relievespain and
severity of sickle-cell complications, by 50%. In children with severe disease,
bone marrow stem cell transplants are risky but may be totally curative. Newer
treatments include orally -administered arginine, which stimulates nitric oxide
production and dilates blood vessels, as well as gene therapy.
Polycythemias
Polycythemia
results in the blood to become slug-gish, due to excessive amounts
of erythrocytes, and elevated hematocrit. A bone marrow cancer called polycythemia vera results in an
extremely high RBCcount, of 8 to 11 million cells per microliter, and also
causes dizziness. Blood volume may be doubled, severely impairing circulation,
and the hematocrit may be as high as 80%. Treatment for severe cases involves therapeutic phlebotomy , in which some
blood is removed from the body. Secondary
polycy-themias involve low oxygen or increased erythropoi-etin. In people
living at high altitudes, it may occur as a normal response to reduced
atmospheric pres-sure and resultant lower oxygen content in the air. In these
individuals, the RBC count is often between 6 and 8 million per microliter.
Artificially induced polycythemia, or blood dop-ing, is often done by athletes who compete in
aerobicevents. The RBCs are partially drawn off and stored. The body replaces
them quickly. A few days before the athletic competition, the stored blood is
reinfused, causing a temporary polycythemia. Theoretically, this should cause
increased oxygen-carrying because of higher hematocrit, and greater speed and
endurance. This does occur, but risks include potential stroke and heart
failure. The practice has been labeled “unethi-cal,” and has since been banned
from competitions such as the Olympics.