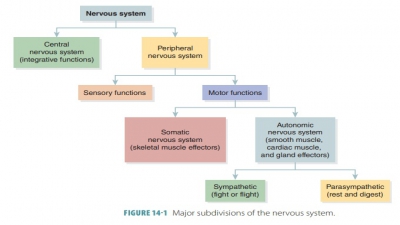
Divisions of the Autonomic Nervous System (ANS)
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Autonomic Nervous System (ANS)
The ANS is divided into the sympathetic and parasympathetic divisions.
Divisions of
the ANS
The ANS is divided into the sympathetic and parasympathetic divisions. Certain visceral organs
have fibers from both divisions,
controlling the acti-vation or inhibition of their actions. The sympathetic
division prepares the body for stressful or emergency situations and is part
of the fight-or-flight respons. This division can change tissue and organ activities by releasing NE at
peripheral synapses and by distributing epinephrine and NE throughout the
body. Sympathetic activation, controlled by the
hypothalamus, occurs when the entire
sympathetic division responds to a crisis situation. When this happens, a
person feels extremely alert, energized, and euphoric. Blood pres-sure,
breathing, and heart rate increase; muscle tone is elevated; and energy
reserves are mobilized for action.
The parasympathetic division
functions in an opposite manner and is part of the rest-and-digest response.
When stress occurs, the sympathetic divi-sion increases heart and breathing
rates. As the stress subsides, the parasympathetic division decreases these
activities. Dual innervation is
applied so the two divi-sions counterbalance the effects of each other. This
utilizes cardiac, pulmonary, esophageal,
celiac, inferior mesenteric, and hypogastric plexuses. Sympathetic and parasympathetic fibers that reach the
heart and lungs pass through the cardiac plexus. Parasympathetic activation is
signified by constricted pupils for better
focusing, increased glandular secretions, raised nutri-ent absorption, and
changes in blood flow that are associated with sexual arousal. In the digestive
tract, smooth muscle activity increases, defecation is stim-ulated, the urinary
bladder contracts, and respiration and heart rate are reduced.
A little-known third division of
the ANS is known as the enteric
nervous system (ENS). It is a network of neurons and
nerve networks in the digestive tract and is influenced by both the sympathetic
and para-sympathetic divisions. The ENS is primarily related to the visceral
reflexes, and has about 100 million neurons and uses all of the
neurotransmitters found in the brain.
Most of the time, the sympathetic
and parasympa-thetic divisions of the ANS have opposite effects such as
excitation versus inhibition. However, these divi-sions may also be
independent, with only one of them innervating certain body structures. They
also may work together and each may control just one stage of a complicated
series of actions. Basically, the sympa-thetic division activates during
emergencies, stress, or exertion, while the parasympathetic division activates
when the body is at rest.
Sympathetic Division
The sympathetic division’s
functions include increased heart rate and respiration, reduced salivation,
clammy skin, and dilation of eye pupils. Mental alertness is dramatically
increased as is the metabolic rate. During physical activity, it constricts
visceral blood vessels and sometimes constricts cutaneous blood vessels. Blood
is moved to active skeletal muscles and the heart, and blood pressure
increases. The sweat glands are activated. Lung bronchioles are dilated,
resulting in increases in ventilation, moving more oxygen to body cells. The
liver releases more glucose into the blood to supply energy to the body.
Simultaneously, it slows down nonessential activities such as motility in the
gastrointestinal tract and the urinary system. The sympathetic division may be
referred to as the “E division” (signifying exercise, emergency, and
excitement).
Parasympathetic Division
The parasympathetic division
keeps energy use by the body to its lowest possible amounts. It controls
digestion of food and elimination of feces and urine. This division stimulates
visceral activity, decreases the metabolic rate, increases salivary and
digestive secre-tions, and increases digestive motility and blood flow. During
digestion, blood pressure and heart rate are lowered while the gastrointestinal
system is active. Also, the pupils of the eyes become constricted and the
lenses are accommodated for close vision. The parasympathetic division may be
referred to as the “D division” (signifying digestion, defecation, and
diuresis). Both divisions antagonize each other’s effects greatly to maintain
homeostasis.
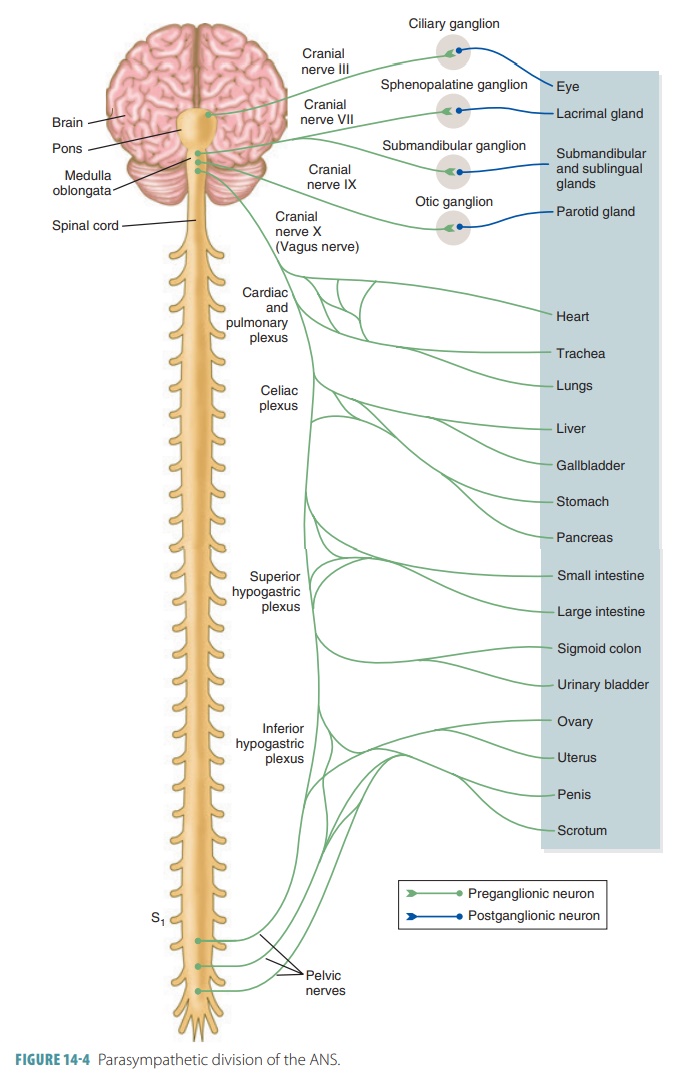
Parasympathetic fibers are
craniosacral, originat-ing in the brain and sacral spinal cord (FIGURE 14-4). They
have long preganglionic and short postganglionic fibers. Parasympathetic
ganglia are mostly located in the visceral effector organs. Overall, the
parasympa-thetic division is simpler than the sympathetic division. It is also
known as the craniosacral division
because its preganglionic fibers emerge from opposite ends of the CNS (the
brain stem and sacral spinal cord). The preganglionic axons run from the CNS,
nearly all the way to the innervated target structures. At these points, axons
synapse with postganglionic neurons of the terminal
ganglia, lying close to or
inside the target organs. Extremely short postganglionic axons emerge from the
terminal ganglia, synapsing with nearby effec-tor cells. In the cranial portion
of the parasympathetic nervous system, preganglionic fibers exist in the facial,
oculomotor, glossopharyngeal, and vagus nerves. Cell bodies of these fibers lie
in related motor cranial nerve nuclei of the brain stem.
Oculomotor Nerves
The parasympathetic fibers of the
oculomotor (III) nerves innervate smooth muscles that cause the pupils of the eyes to constrict and the lenses to bulge, which are
both used when focusing. Cell bodies of the postganglionic neurons lie in the ciliary ganglia inside
the eye orbits.
Facial Nerves
The parasympathetic fibers of the
facial (VII) nerves stimulate large
glands located in the head. Pregangli-onic fibers synapse with postganglionic
neurons in the pterygopalatine
ganglia, which are just
posterior to the maxillae. Preganglionic neurons stimulating sali-vary
glands (submandibular and sublingual) synapse with postganglionic neurons in
the submandibular ganglia.
Glossopharyngeal Nerves
The parasympathetic fibers of the
glossopharyngeal (IX) nerves begin in the inferior salivary nuclei of the medulla. They synapse in the otic ganglia just
infe-rior to the foramen ovale of the skull. The glossopha-ryngeal nerves
innervate the parotid salivary glands.
Vagus Nerves
The two vagus (X) nerves make up between 80% and 90% of the parasympathetic
outflow fibers in the body. Their preganglionic axons begin primarily in the
dor-sal motor nuclei of the medulla. They synapse in termi-nal ganglia that are
mostly located in the target organ walls. Branches of the vagus nerves pass to
the cardiac plexuses, which supply fibers to the heart that slow the heart rate. Other
branches supply the pulmonary plexuses serving the lungs and the
esophageal plexuses serving the
esophagus. Near the esophagus, the main trunks of the vagus nerves join fibers to form anterior and posterior vagal trunks, each with fibers from both vagus nerves. The trunk continues down to the abdominal
cavity, sending fibers through the large abdominal
aortic plexus, which is made up of the celiac, superior mesenteric, and
hypogastric plexuses running along the aorta. The large abdominal aortic plexus
then branches off to the abdominal viscera. The celiac ganglion innervates the
smooth muscles of the stomach, small intestine, liver, pancreas, and the
ascending half of the transverse colon.
The sacral portion of the
parasympathetic division serves the pelvic organs and the distal half of the
large intestine. It arises from the lateral gray matter neurons of the spinal
cord segments S2 to S4. Axons of these neurons continue
through the ventral roots of the spinal nerves to the ventral rami. They branch
to form the pelvic splanchnic nerves that pass through the
inferior hypogastric (pelvic) plexus in the floor of the pelvis.
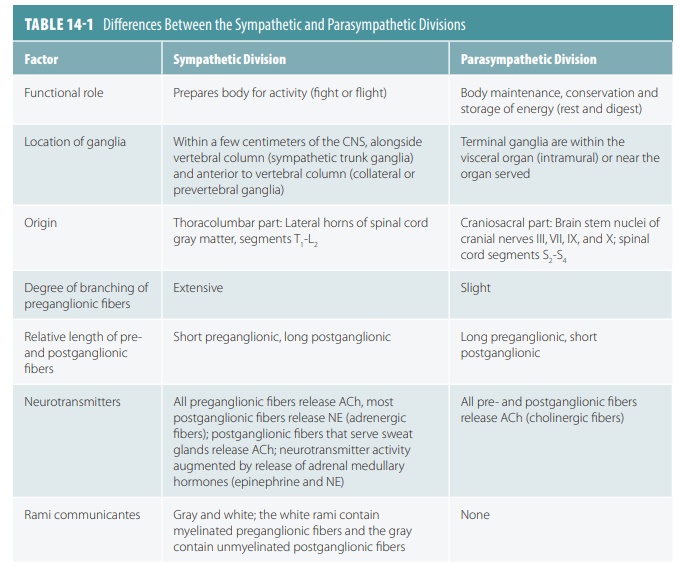
Splanchnic nerves carry fibers that
synapse in collateral ganglia. TABLE 14-1 compares
differences between the sympathetic and parasympathetic divisions.
1. Identify the roles of the
sympathetic and parasympathetic nervous systems.
2. Define the terms “terminal
ganglia” and “lateral horns.”
3. Explain what may occur
with preganglionic and postganglionic neurons when a preganglionic axon reaches
a trunk ganglion.
Related Topics