Gastrointestinal Infections
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Clinical Uses Of Antimicrobial Drugs
The gut is vulnerable to infection by viruses, bacteria, parasites and occasionally fungi. Virus infections are the most prevalent but are not susceptible to chemotherapeutic intervention. Bacterial infections are more readily recognized and raise questions concerning the role of antibiotic management. Parasitic infections of the gut are beyond the scope of this article.
GASTROINTESTINAL INFECTIONS
The gut is vulnerable to infection by viruses, bacteria, parasites and occasionally fungi. Virus infections are the most prevalent but are not susceptible to chemotherapeutic intervention. Bacterial infections are
more readily recognized and raise questions concerning the
role of antibiotic management. Parasitic infections of the gut are
beyond
the scope of this article.
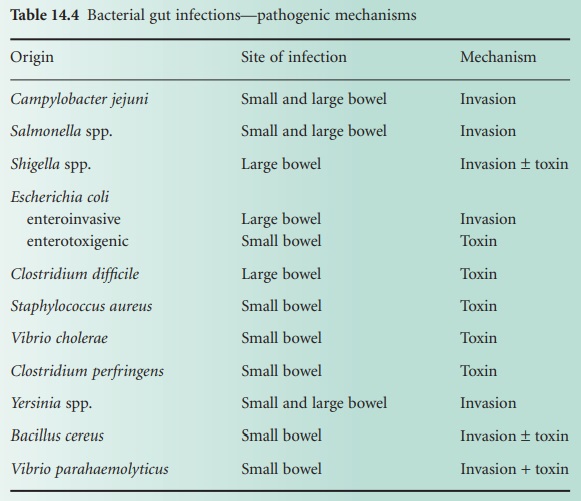
Bacteria cause
disease of the gut as a result
of either mucosal invasion or toxin production or a combination of the two mechanisms, as summarized in Table 14.4.
Treatment is largely directed
at replacing and maintaining an adequate
intake of fluid
and electrolytes. Antibiotics are generally not recommended for infective gastroenteritis, but deserve consideration where they have been demonstrated
to abbreviate the acute disease
or to prevent complications including prolonged gastrointestinal excretion of the pathogen where
this poses a public health hazard.
It should
be emphasized that most gut infections are self-limiting. However, attacks can be severe and may result in hospitalization.
Antibiotics are used to treat severe Campylobacter and Shigella infections; erythromycin and ciprofloxacin, respectively, are the preferred agents. Such treatment abbreviates the disease
and eliminates gut excretion in Shigella
infection. However,
in severe Campylobacter infection the data are currently equivocal, although
the clinical impression favours the use of erythromycin for severe infections. The role of antibiotics for Campylobacter and Shigella infections
should be contrasted with gastrointestinal salmonellosis, for which antibiotics are contraindicated as they do not
abbreviate symptoms, are associated with more prolonged gut excretion and introduce the risk of adverse
drug reactions. However, in severe salmonellosis, especially at extremes of age, systemic
toxaemia and bloodstream infection can
occur and under
these circumstances treatment with either ciprofloxacin or trimethoprim is appropriate.
Typhoid
and paratyphoid fevers
(known as enteric fevers), although acquired
by ingestion of salmonellae,
Sal. enterica serovar Typhi and Sal. enterica
serovar Paratyphi, respectively, are largely systemic
infections and antibiotic therapy is mandatory; ciprofloxacin is now the drug of choice although
trimethoprim or chloramphenicol are satisfactory
alternatives. Prolonged gut excretion of Sal. enterica
serovar Typhi is a well-known
complication of typhoid fever
and is a major public health hazard in developing countries. Treatment with ciprofloxacin or high-dose ampicillin can eliminate the gall bladder excretion which is the major site of persistent infection in carriers. However, the presence of gallstones reduces the chance of cure.
Cholera is a serious infection causing epidemics throughout Asia. Although a toxin-mediated
disease, largely controlled with replacement of fluid and electrolyte losses,
tetracycline has proved effective
in eliminating the causative vibrio from the bowel,
thereby abbreviating the course of the illness
and reducing the total fluid
and electrolyte losses.
Traveller’s diarrhoea may be caused by one of many
gastrointestinal
pathogens (Table 14.4). However,
enterotoxigenic Escherichia coli is
the most common pathogen. While it is generally short-lived, traveller’s
diarrhoea can seriously mar a brief period
abroad, be it for holiday
or business purposes. Although not universally accepted, the use of short-course trimethoprim or quinolone such as
ciprofloxacin can abbreviate an attack in patients with severe disease.
Related Topics
