Respiratory Tract Infections
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Clinical Uses Of Antimicrobial Drugs
Infections of the respiratory tract are among the commonest of infections, and account for much consultation in general practice and a high percentage of acute hospital admissions. They are divided into infections of the upper respiratory tract, involving the ears, throat, nasal sinuses and the trachea, and the lower respiratory tract (LRT), where they affect the airways, lungs and pleura.
RESPIRATORY TRACT INFECTIONS
Infections of the respiratory tract are among the commonest of infections,
and account for much consultation in general practice and a high percentage of
acute hospital admissions. They are divided into infections of the upper
respiratory tract, involving the ears, throat, nasal sinuses and the trachea,
and the lower respiratory tract (LRT), where they affect the airways, lungs and
pleura.
a)
Upper Respiratory
Tract Infections
Acute pharyngitis presents a diagnostic
and therapeutic dilemma. The majority of sore throats are caused by a variety
of viruses; fewer than 20% are bacterial and hence potentially responsive to
antibiotic therapy. However, antibiotics are widely prescribed and this
reflects the difficulty in discriminating streptococcal from non-streptococcal
infections clinically in the absence of microbiological documentation.
Nonetheless, Strep. pyogenes is the most
important bacterial pathogen and this responds to oral penicillin. However, up
to 10 days’ treatment is required for its eradication from the throat. This
requirement causes problems with compliance as symptomatic improvement generally
occurs within 2–3 days.
Although viral infections are important causes of both otitis media and
sinusitis, they are generally self limiting. Bacterial infections may
complicate viral illnesses, and are also primary causes of ear and sinus
infections. Streptococcus pneumoniae and Haemophilus influenzae are the
commonest bacterial pathogens. Amoxicillin is widely prescribed for these
infections as it is microbiologically active, penetrates the middle ear and
sinuses, is well tolerated and has proved effective.
b)
Lower Respiratory
Tract Infections
Infections of the LRT include pneumonia, lung abscess, bronchitis,
bronchiectasis and infective complications of cystic fibrosis. Each presents a
specific diagnostic and therapeutic challenge, which reflects the variety of
pathogens involved and the frequent difficulties in establishing an accurate
microbial diagnosis. The laboratory diagnosis of LRT infections is largely
dependent upon culturing sputum. Unfortunately this may be contaminated with
the normal bacterial flora of the upper respiratory tract during expectoration.
In hospitalized patients, the empirical use of antibiotics before admission
substantially diminishes the value of sputum culture and may result in
overgrowth by non-pathogenic microbes, thus causing difficulty with the
interpretation of sputum culture results. Alternative diagnostic samples
include needle aspiration of sputum directly from the trachea or of fluid
within the pleural cavity. Blood may also be cultured and serum examined for
antibody responses or microbial antigens. In the community, few patients will
have their LRT infection diagnosed microbiologically and the choice of
antibiotic is based on clinical diagnosis.
i)
Pneumonia
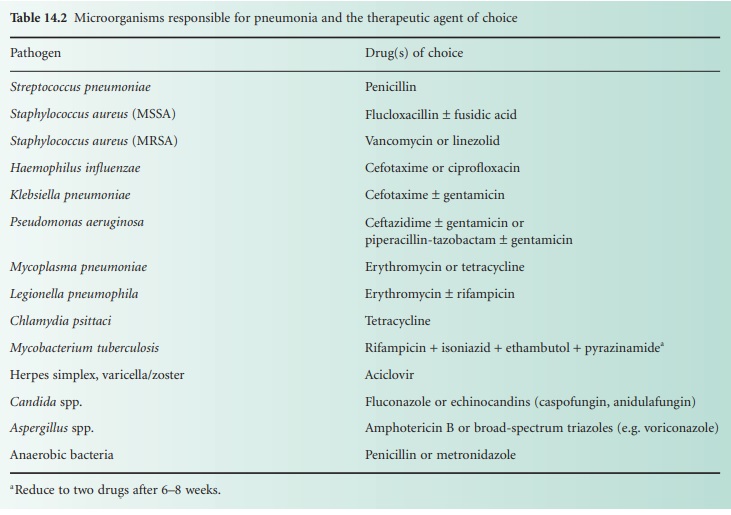
The range of pathogens causing acute
pneumonia includes viruses, bacteria and, in the immuno-compromised host,
parasites and fungi. Table 14.2 summarizes
these pathogens and indicates drugs appropriate for their treatment. Clinical
assessment includes details of the evolution of the infection, any evidence of
a recent viral infection, the age of the patient and risk factors such as
corticosteroid therapy or pre-existing lung disease. The extent of the pneumonia,
as assessed clinically or by X ray, is also important.
Streptococcus pneumoniae remains the commonest cause of pneumonia and still responds well
to penicillin despite a global increase in isolates showing reduced susceptibility
to this agent. So called ‘respiratory quinolones’ such as levofloxacin and
moxifloxacin, which exhibit increased activity against Gram positive organisms
compared to ciprofloxacin, are an alternative. A number of atypical infections
may cause pneumonia and include Mycoplasma pneumoniae,
Legionella pneumophila, psittacosis and occasionally Q fever.
With psittacosis there may be a history of contact with parrots or budgerigars;
while legionnaires’ disease has often been acquired during hotel holidays in
the Mediterranean area. The atypical pneumonias, unlike pneumococcal pneumonia,
do not respond to penicillin. Legionnaires’ disease is treated with
erythromycin and, in the presence of severe pneumonia, rifampicin is added to
the regimen. Mycoplasma infections are best treated with either erythromycin or
tetracycline, while the latter drug is indicated for both psittacosis and Q
fever.
ii)
Lung abscess
Destruction of lung tissue may lead to
abscess formation and is a feature of aerobic Gram-negative bacillary and Staph. aureus infections. In addition, aspiration
of oropharyngeal secretion can lead to chronic low grade sepsis with abscess
formation and the expectoration of foul smelling sputum that characterizes
anaerobic sepsis. The latter condition responds to high dose penicillin, which
is active against most of the normal oropharyngeal flora, while metronidazole
may be appropriate for strictly anaerobic infections. In the case of aerobic
Gram-negative bacillary sepsis, aminoglycosides, with or without a
broad-spectrum cephalosporin, are the agents of choice. Acute staphylococcal
pneumonia is an extremely serious infection and requires treatment with high
dose flucloxacillin alone or in combination with fusidic acid.
iii)
Cystic fibrosis
Cystic fibrosis is a multisystem
congenital abnormality that often affects the lungs and results in recurrent
infections, initially with Staph. aureus, subsequently with H. influenzae and
eventually leads on to recurrent Pseudomonas aeruginosa infection.
The last organism is associated with copious quantities of purulent sputum that
are extremely difficult to expectorate. Ps. aeruginosa is a co factor in the
progressive lung damage that is eventually fatal in these patients. Repeated
courses of antibiotics are prescribed and although they have improved the
quality and longevity of life, infections caused by Ps. aeruginosa are
difficult to treat and require repeated hospitalization and administration of
parenteral antibiotics such as an aminoglycoside, either alone or in
combination with an antipseudomonal penicillin or cephalosporin. The dose of
aminoglycosides tolerated by these patients is often higher than in normal
individuals and is associated with larger volumes of distribution for these and
other agents. Some benefit may also be obtained from inhaled aerosolized antibiotics.
Unfortunately drug resistance may emerge and makes drug selection more
dependent upon laboratory guidance.
Related Topics
