Glomerular Filtration
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Urinary System
Glomerular filtration is a passive process that ini-tiates urine formation in the renal corpuscle. It uses hydrostatic pressure to force fluids and solutes through membranes.
Formation of Urine
The purposes of urine formation are to cleanse the blood and balance the body’s chemical substances. Three steps are involved in urine formation and the regulation of blood composition: glomerular filtra-tion, tubular reabsorption, and tubular secretion.
Glomerular Filtration
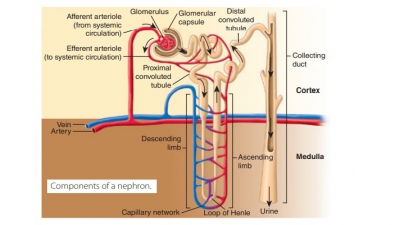
Glomerular filtration is a passive process that ini-tiates urine formation in the renal corpuscle. It uses hydrostatic pressure to force fluids and solutes through membranes. The plasma is filtered by the glomeru-lar capillaries, producing filtrate that is free of cells and proteins. Most of this fluid is reabsorbed into the bloodstream via the colloid osmotic pressure of the plasma. Using two capillaries in series, the neph-rons use glomerular filtration to help produce urine. The first capillary bed filters forming interstitial fluid but does not form it. The filtrate, which is derived from the plasma, moves into the renal tubule to form urine. Every 24 hours, glomerular filtration produces 180 liters or 47 gallons of fluid—this is more than four times the amount of total body water. Less than 1.5 liters, which is lower than 1% of the fluid, leaves the body as urine.
The filtration membrane is located between the interior glomerular capsule, also called Bowman’s capsule, and the blood. It is a porous membrane, allowing water and solutes that are smaller than plasma proteins to freely pass through. Any mac-romolecules caught in the filtration membrane are engulfed by glomerular mesangial cells, which are spe-cialized pericytes. Any molecules smaller than 3 nm in diameter can pass through freely, from the blood into the capsule. These molecules include amino acids, glucose, nitrogenous wastes, and water. An example of a substance that is too large to pass through the filtra-tion membrane is albumin.
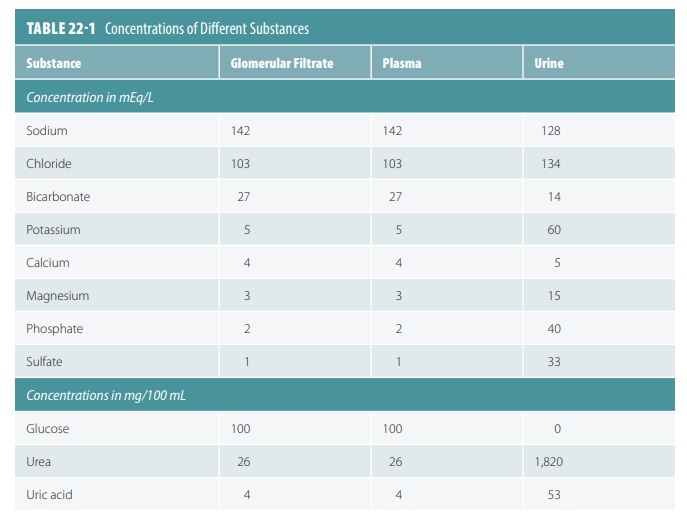
Because of this, these substances are similar in concentration to blood and glomerular filtrate. Glo-merular filtrate is mostly water with the same com-ponents as blood plasma, except for large protein molecules. TABLE 22-1 compares concentrations of substances in glomerular filtrate, plasma, and urine. Molecules larger than 5 nm usually cannot enter the tubules, so plasma proteins remaining in the capillar-ies help to regulate the oncotic or colloid osmotic pres-sure of glomerular blood. Therefore, all water cannot be lost to the capsular spaces. The filtration membrane is probably functioning abnormally when proteins or blood cells become present in the urine.
The outward pressure that affects filtration is the hydrostatic pressure in the glomerular capillaries. This is basically the same as glomerular blood pressure and the strongest force moving water and solutes from the blood across the filtration membrane. Here, the blood pressure is high in the glomerulus, at about 55 mm Hg. In other capillary beds, the pressure is only 26 mm Hg.
The reason for the difference is that the glomerular cap-illaries drain via a high-resistance efferent arteriole with a smaller diameter than the afferent arteriole supplying them. Filtration then occurs along all the length of every glomerular capillary. Reabsorption does not occur as it does in other capillary beds. The colloid osmotic pressure in the glomerular capsular space is nearly zero, because practically no proteins enter the capsule.
The osmolarity of a solution is its osmotic concen-tration or the total number of solute particles per liter. This is usually expressed in osmoles per liter (Osm/L) or milliosmoles per liter (mOsm/L). Body fluids have an osmolarity of approximately 300 mOsm/L, whereas fresh water is 5 mOsm/L and seawater 1,000 mOsm/L.
Glomerular Filtration Rate
The glomerular filtration rate (GFR)is defined as the volume of filtrate that forms every minute by the activ-ities of the two million glomeruli in the kidneys. It is directly proportional to the net filtrationpressure, the total surface area that is available for filtration, and the permeability of the filtration membrane (FIGURE 22-7). The net filtration pressure forces sub-stances out of the glomerulus and is usually positive pressure. Tiny openings called fenestrae in glomer-ular capillary walls make them more permeable than the capillaries of other tissues. Cells called podocytes cover these capillaries, helping to make them imperme-able to plasma proteins. The feet of the podocytes are called pedicels. Materials that pass from the blood, at the glomerulus, must be tiny enough to move through filtration slits between adjacent pedicels.
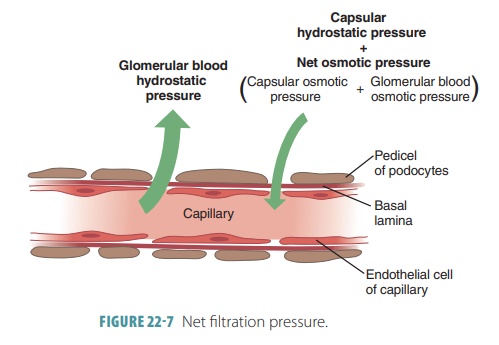
Net filtration pressure is directly proportional to the GFR. All factors related to GFR affect net filtration pressure. Any changes in afferent or efferent arteriole diameters alter the GFR. During filtration through capillary walls, proteins in the plasma raise colloid osmotic pressure with the glomerular capillaries. Anything that decreases plasma colloid osmotic pres-sure increases the filtration rate. The kidneys consume up to 25% of all oxygen the body uses while resting.
Regulation of Glomerular Filtration
The GFR is regulated by intrinsic controls or renal auto-regulation and extrinsic controls via the nervous and endocrine systems. The intrinsic controls occur within the kidneys, whereas the extrinsic controls maintain blood pressure. The GFR must be relatively constant, so the kidneys can manufacture filtrate and maintain extracellular homeostasis. The body’s overall blood pressure must also be relatively constant. If nothing else changes, when the GFR increases, urine output also increases. This reduces blood volume and blood pres-sure. When the GFR decreases, the opposite occurs.
Extreme changes to mean arterial pressure, less than 80 mm Hg or higher than 180 mm Hg, causes the extrinsic controls to dominate to stop damage to the brain and other vital organs. Changing only the glomerular hydrostatic pressure can control the GFR. Therefore, the major mechanisms of pressure control focus on changing the glomerular hydro-static pressure. When it rises, so do both the net filtration pressure and the GFR. The GFR will be reduced to zero if the glomerular hydrostatic pres-sure falls by 18% or greater, meaning it must be con-trolled precisely.
The GFR is kept relatively constant by autoregu-latory mechanisms over the 80–180 mm Hg arterial pressure range. Normal daily changes in exercise activity, posture, or sleep do not result in significant changes in excretion of water and solutes. However, serious hemorrhage that causes extremely low sys-temic blood pressure will result in hypovolemic shock, which cannot be stopped by the intrinsic controls.
Therefore, when mean arterial pressure is lower than 80 mm Hg, extrinsic controls take over and the auto-regulatory mechanisms stop working.
The hormonal and neural mechanisms used in extrinsic controls include the sympathetic nervous system and the renin–angiotensin–aldosterone mech-anism. Although the neural kidney controls help the whole body, the kidneys may suffer as a result. The kid-ney blood vessels are dilated, with their autoregulatory mechanisms dominating control when extracellular fluid volume is normal. At this time, the sympathetic nervous system is resting. Once the extracellular fluid volume becomes lower than 80 mm Hg, blood must be moved or shunted to vital organs. At that point, neural controls override autoregulatory mechanisms, which may reduce kidney blood flow enough to dam-age these organs.
Falling blood pressure causes the sympathetic nerve fibers to release norepinephrine and the adrenal medulla to release epinephrine. As a result, vascular smooth muscles constrict. This increases periph-eral resistance, returning blood pressure to normal. This is the baroreceptor reflex. The GFR decreases from constriction of the afferent arterioles, assist-ing blood volume and pressure to return to normal. The renin–angiotensin–aldosterone mechanism is the primary control that increases blood pressure, yet it regulates GFR indirectly. Inadequate blood pressure means glomerular filtration cannot occur. It causes the granular cells in the juxtaglomerular complex to release renin. This occurs by either direct stimulation of granular cells, stimulation of granular cells via input from activated cells of the macula densa, or reduced stretching of granular cells.
Secretion of renin responds to three types of stimuli:
■■ When special afferent arteriole cells sense a drop in blood pressure
■■ In response to sympathetic stimulation
■■ When the macula densa senses decreased chloride, potassium, and sodium ions that reach the distal tubule
Renin in the bloodstream reacts with the plasma protein angiotensinogen, forming angiotensin I. In the lungs and blood plasma, angiotensin- converting enzyme converts angiotensin I to angiotensin II. Angiotensin II helps maintain sodium and water balance as well as blood pressure. It vaso-constricts the efferent arteriole, raising glomerular capillary hydrostatic pressure. This helps the decrease in GFR. Angiotensin II stimulates the adrenal cortex to secrete aldosterone, encouraging tubular reabsorp-tion of sodium.
1. Explain which types of molecule are trapped by the glomerular filtration membrane and which ones are not.
2. Contrast how glomerular filtration is regulated by intrinsic and extrinsic controls.
3. Describe the two types of extrinsic controls involved in glomerular filtration.