Tubular Secretion
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Urinary System
Tubular secretion selectively moves substances from the blood in the peritubular capillary via the filtrate into the renal tubule.
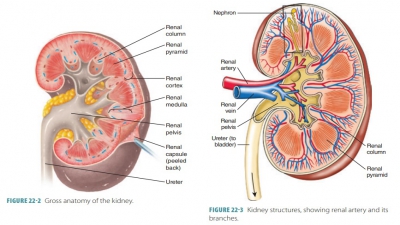
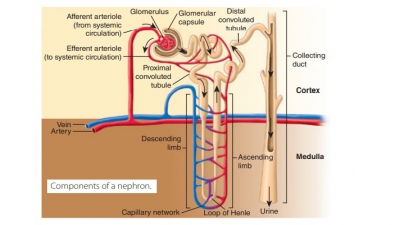
Formation of Urine
The purposes of urine formation are to cleanse the blood and balance the body’s chemical substances. Three steps are involved in urine formation and the regulation of blood composition: glomerular filtra-tion, tubular reabsorption, and tubular secretion.
Tubular Secretion
Tubular secretion selectively moves substances from the blood in the peritubular capillary via the filtrate into the renal tubule. These substances include hydro-gen, ammonia, potassium ions, creatinine, and various organic acids and bases. Certain substances synthe-sized in the tubule cells such as bicarbonate are also secreted. Although essentially the opposite of tubular reabsorption, it also occurs along the length of the renal tubule and collecting duct. Some substances that the body must excrete, such as hydrogen ions and some toxins, are removed more quickly than through filtration. The proximal convoluted tubule is the main site of excretion, except for potassium. The cortical sec-tions of the collecting ducts are also active in secretion.
Tubular secretion is important for four major pro-cesses: disposing of substances, eliminating undesirable substances, removing excessive potassium, and con-trolling blood pH. Tubular secretion disposes of cer-tain drugs and metabolites that may be tightly bound to plasma proteins. Because these proteins are usually not filtered, the bound substances are also not filtered, and therefore must be secreted. Tubular secretion eliminates undesirable substances or end products that have been passively reabsorbed (FIGURE 22-9). Exam-ples include the nitrogenous wastes, and also urea and uric acid. Nephron processing of urea is complicated, but basically up to 50% of filtrate urea is excreted.
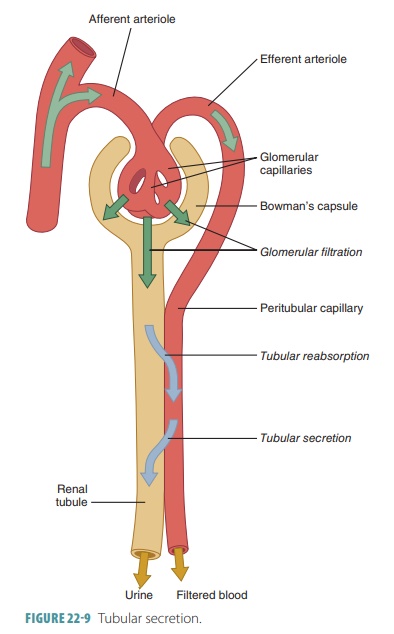
Tubular secretion also removes excessive potas-sium from the body. Nearly all potassium ions in the filtrate are reabsorbed in the proximal convoluted tubule and ascending nephron loop. Therefore, almost all potassium in the urine is derived from active tubu-lar secretion into the last portions of the distal con-voluted tubule and collecting ducts. This secretion is controlled by aldosterone. When blood pH drops toward being acidic, renal tubule cells actively secrete more hydrogen ions into the filtrate. They retain and generate more bicarbonate, which is a base. There-fore, blood pH rises and the urine drains off any excess hydrogen. In the opposite situation, blood pH approaching alkalinity causes chloride ions to be reab-sorbed instead of bicarbonate. The bicarbonate then leaves the body via the urine.
At the distal convoluted tubule, potassium ions are removed from the peritubular fluid in exchange for sodium ions from the tubular fluid. The potas-sium ions then diffuse through potassium leak channels. Hydrogen ions generated by carbonic acid dissociation are secreted in exchange for sodium ions in the tubular fluid. This acidifies the tubular fluid while blood pH is elevated. Because production of lactic acid and ketone bodies during postabsorp-tion can cause acidosis, both the proximal and distal convoluted tubules deaminate amino acids to strip off the amino groups. The reaction sequence binds hydrogen ions and yields ammonium and bicarbon-ate ions. The ammonium ions are pumped into the tubular fluid, whereas the bicarbonate ions enter the bloodstream via the peritubular fluid. There-fore, tubular deamination provides carbon chains for catabolism while generating bicarbonate ions to increase the plasma’s buffering capacity.
Function of the Vasa Recta
The vasa recta functions to return solutes and water reabsorbed in the renal medulla to the bloodstream without changing the concentration gradient. These long, straight capillaries are parallel to the long nephron loop of the juxtamedullary nephrons. When blood enters the vasa recta from the peritu-bular capillaries, its osmotic concentration is nearly 300 mOsm per liter. Blood descending into the medulla gradually increases in osmotic concentra-tion when the peritubular fluid’s solute concentra-tion rises. This increase utilizes solute absorption as well as water loss. Solute absorption is the main fac-tor since plasma proteins control the osmotic flow of water from the blood.
Blood that ascends toward the cortex slowly decreases its osmotic concentration, as there is a decline in solute concentration of the peritubular fluid. This also involves both solute diffusion and osmosis. However, osmosis is the main factor here, since the presence of plasma proteins has no opposition to the osmotic flow of water into the blood. Overall, the results inside the vasa recta are:
■■ Some solutes absorbed in the descending portiondo not diffuse out in its ascending portion
■■ More water moves into the ascending portion than moves out in the descending portion
Therefore, the vasa recta carries water as well as sol-utes out of the medulla. Normally, removal of solutes and water by the vasa recta allows for precise bal-ancing of solute reabsorption and osmosis inside the medulla.
1. Where does most reabsorption occur in the nephron?
2. Contrast the primary and secondary active transport processes.
3. Explain how movement of sodium ions controls reabsorption of water and solutes.